Federal, Provincial, Territorial Public Health Response Plan for Ongoing Management of COVID-19
Download in PDF format
(5.77 MB, 79 pages)
Organization: Public Health Agency of Canada
Date published: 2022-03-31
Table of contents
- List of acronyms and abbreviations
- Executive summary
- Introduction
- Context
- COVID-19 response goals and objectives
- Forward planning
- Addressing the consequences of pandemic response
- COVID-19 FPT response components
- Assessment and evaluation
- Appendix 1: Modelling support for forward planning
- Appendix 2: Epidemiological drivers
- Appendix 3: Planning for the reasonable worst case scenario
- Appendix 4: COVID-19 response planning with Indigenous communities
- Appendix 5: Surveillance
- Appendix 6: Laboratory response activities
- Appendix 7: Public health measures
- Appendix 8: Infection prevention and control
- Appendix 9: Vaccination
- Appendix 10: International border and travel health measures
- Appendix 11: Health care systems infrastructure
- Appendix 12: Communications and outreach
- Appendix 13: Research
- References
List of acronyms and abbreviations
- AEFI
- adverse events following immunization
- CIC
- Canadian Immunization Committee
- CPIP
- Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector
- FPT
- federal, provincial, territorial
- FPT PHRPBE
- Federal, Provincial, Territorial Public Health Response Plan for Biological Events
- IPC
- infection prevention and control
- ISC
- Indigenous Services Canada
- LAC
- Logistics Advisory Committee
- NACI
- National Advisory Committee on Immunization
- PHA(s)
- public health authority(ies)
- PHAC
- Public Health Agency of Canada
- PHM(s)
- public health measure(s)
- P/T
- provincial/territorial
- PT
- Province, Territory
- SAC
- Special Advisory Committee
- TAC
- Technical Advisory Committee
- VOC(s)
- variant(s) of concern
- WHO
- World Health Organization
- 2SLGBTQI+
- two-Spirit, lesbian, gay, bisexual, transgender, queer (or questioning), intersexed plus
Executive summary
This document is the third edition of the federal, provincial, territorial (FPT) plan which was developed in collaboration with federal, provincial and territorial public health officials via the FPT Special Advisory Committee (SAC) on COVID-19, First Nations, Inuit and Métis partners, and health system partners, for these and other stakeholders. It is an evergreen document that is intended to provide a Pan-Canadian forward planning approach for ongoing management of COVID-19 in Canada and facilitate awareness and coordination both within and beyond the public health sector.
This edition focuses on the transition from the acute response to waves of COVID-19 activity occurring in a largely susceptible Canadian population, towards a more sustainable long-term response to the ongoing presence of COVID-19 in the context of increased population immunity and other public health priorities. This is referred to as the Transition phase, and while acute response needs may be reduced during this time, there is a need to maintain readiness to respond to any new COVID-19 risks while addressing ongoing response and recovery needs. Much like other technical guidance, this document may require updating as our scientific knowledge of the SARS-CoV-2 pathogen and duration of immunity due to the COVID-19 vaccines and previous infections increases, and the epidemiological picture evolves in Canada and globally.
The plan acknowledges jurisdictional roles and responsibilities, and therefore provincial/territorial (P/T) flexibility and customization are expected. The autonomy of provinces and territories with respect to management of their respective health systems is acknowledged; this document is not intended to convey any requirements or obligations. First Nations, Inuit and Métis communities may choose to adapt approaches to the specific needs and contexts of their communities, as highlighted in the sections focusing on planning with Indigenous Communities.
Key elements of this edition of the plan include:
- public health objectives for the Transition phase;
- forward planning assumptions;
- planning for ongoing response, recovery and readiness;
- a section on addressing the consequences of pandemic response; and
- appendices with updated summaries of each main component of the public health response (i.e., Surveillance, Laboratory Response Activities, Public Health Measures, Infection Prevention and Control and Clinical Care Guidance, Vaccination, International Border and Travel Health Measures, Health Care Systems Infrastructure, Risk Communications and Outreach, and Research).
The pandemic response goal, to minimize serious illness and overall deaths while minimizing societal disruption as a result of the COVID-19 pandemic, highlights the need to balance the impact of COVID-19 in terms of both severe outcomes and societal disruption. The ability to achieve this balance has been challenging during the response and is likely to be one of the key lessons learned for future pandemic responses.
Vaccination and public health measures (PHMs) have been successful in reducing the number of cases of COVID-19 and associated serious illness and deaths in Canada, however, the Omicron-driven wave necessitated the re-implementation of restrictive measures in many jurisdictions in order to ensure health care systems did not become overwhelmed. The COVID-19 response has been unprecedented with the swift implementation and public adoption of response measures. However, use of these measures now needs to be de-escalated or adapted in the context of: decreasing incidence of infection, circulation of a less virulent variant, high vaccination coverage, infection-acquired immunity, public fatigue with the pandemic response Footnote 1Footnote 2Footnote 3 Footnote 4Footnote 5 , and the unintended physical and mental health consequences of the pandemic response Footnote 6Footnote 7 Footnote 8. At the same time there is a need to plan ahead for the potential for repeated emergence of new variants of concern (VOCs) that may be more transmissible, severe, and/or immune-evasive. This will involve evaluating the menu of options for public health measure (i.e., pharmaceutical and non-pharmaceutical) with consideration of the triggers and timing of each. It is expected that jurisdictions may not enact broad, restrictive measures unless absolutely necessary (e.g., if there is high observed severity).
The World Health Organization (WHO) promotes use of a risk-based approach across the continuum of pandemic phases, including the Alert phase, Pandemic phase, Transition phase and Interpandemic phase. Footnote 9 This edition of the plan promotes a risk management approach, which involves considering the likelihood and impacts of potential threats like new VOCs, while also mitigating the impact of realized risks.
As jurisdictions move out of the acute response phase and start to focus on recovery and preparedness for the routine management of COVID-19 in the Canadian population, there is a need to monitor, assess and revisit COVID-19 risks in the context of other public health priorities. This is reflected in the updated ongoing management objectives for the Transition phase. In particular, recovery activities need to address health consequences and risks, backlogs within health care systems and the impact of interrupted public health program delivery, that have occurred over the course of the pandemic response.
The disproportionate impact of both health outcomes and response measures, on some groups within Canada Footnote 10 Footnote 11 has been another key observation over the course of the pandemic to date. The restrictive nature of many of the response measures have had some negative health, well-being and societal consequences for groups such as: older adults, essential workers, children and youth, racialized populations, Indigenous Peoples, people living with disabilities, women, Two-Spirit, lesbian, gay, bisexual, transgender, queer (or questioning), intersexed plus (2SLGBTQI+) communities, people who use drugs, people living on low incomes, newcomers to Canada, and people who are experiencing homelessness and/or under-housed. Footnote 12 Footnote 13 Footnote 14
An overall lack of public health and health care capacity, in particular surge capacity, in Canada, both in terms of human resources and infrastructure, has been clearly illustrated clearly during this pandemic but particularly with the Omicron-driven wave.
The deleterious impact the COVID-19 pandemic response has had on the mental and physical health of responders, given its duration and intensity, and how this might affect recovery efforts and future response capacity, also requires consideration. This is the time to document “lessons learned” and to think broadly about system-wide improvements. How lessons learned will be addressed by current responders and effectively “passed on” to decision-makers, the next cohort of responders (e.g., students in health disciplines) and society at large, needs to be a part of this multi-faceted process.
Introduction
The purpose of the Federal, Provincial, Territorial Public Health Response Plan for Ongoing Management of COVID-19, is to provide federal, provincial and territorial public health officials, First Nations, Inuit and Métis partners, health system partners and other stakeholders with a Pan-Canadian forward planning approach for ongoing management of COVID-19 in Canada. This plan promotes a long-term risk management approach.
The first edition covered immediate planning imperatives for the fall/winter 2020 period and the second edition focused largely on preparedness for variants of concern (VOCs). This third edition focuses on the transition from the acute response to waves of COVID-19 activity occurring in a largely susceptible Canadian population, towards a more sustainable long-term response to the ongoing presence of COVID-19 in the context of increased population immunity and other public health priorities.
As an evergreen document this third edition reflects that scientific knowledge of the SARS-CoV-2 pathogen has increased, the epidemiological picture has further evolved in Canada and globally, the understanding of the disproportionate impact the pandemic has had on marginalized population groups has grown Footnote 15 Footnote 16 , risk mitigation strategies have shifted, and new medical countermeasures have become available (i.e., vaccines, therapeutics and diagnostics). It recognizes the need to balance the strategies and measures necessary to minimize COVID-19 risks against the need to address the public health and societal impacts of the sustained pandemic and the unintended consequences of the measures that have been required to mitigate risks to date.
Referencing the World Health Organization’s (WHO) “Continuum of Pandemic Phases”, previously developed for pandemic influenza preparedness, response and recovery; this document focuses on FPT public health activities that are needed for the “Transition phase”. This is the phase between the acute pandemic response and the phase where COVID-19 is able to be managed like other common infectious diseases in Canada. While acute response needs may be reduced during this time, there is a need to maintain readiness to respond to any new COVID-19 risks while addressing ongoing response and recovery needs. The Transition phase may occur over years, not months, and the emergence of new VOCs and/or impact of waning immunity that may be associated with increased disease activity and possibly increased severity, could necessitate a return to more acute response type activities during this time frame.
The timing of the transition may be varied across Canada due to differences in epidemiology, availability of health care resources, and risk tolerance. This edition of the Plan is informed by the current context, and experience and evidence gained over the course of the pandemic response. As with previous editions, this third edition also draws on existing intergovernmental pandemic preparedness, public health emergency planning and data, information and resource sharing agreements, arrangements and protocols in addition to the Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector (CPIP). It is assumed that an ongoing (but appropriately scaled) FPT coordinated response structure and activities as outlined in the FPT Public Health Response Plan for Biological Events (FPT PHRPBE), will be needed to support the ongoing response, recovery and readiness requirements during the Transition phase.
As with other FPT plans, this document outlines overarching objectives, acknowledges jurisdictional roles and responsibilities, identifies when cohesive FPT approaches are anticipated and when provincial/territorial (P/T) flexibility and customization are expected. The autonomy of provinces and territories with respect to management of their respective health systems is acknowledged; this document is not intended to convey any requirements or obligations. This document has been developed to facilitate planning for the management of COVID-19 that is not only flexible and adaptive but driven by the assessment of COVID-19 risks in the Canadian population going forward.
Context
COVID-19 continues to represent an unprecedented challenge to the health, social and economic well-being of Canadians, and the global community. More than two years into the pandemic, the Canadian response has been strengthened by the availability of vaccines, testing, and therapeutics but further challenged by the emergence of highly transmissible and immune evasive VOCs.
The availability of vaccines and rollout of population-based vaccine programs that prioritized reducing the health impact in people at higher risk for poor health outcomes first, had a significant impact on COVID-19 associated serious illness and overall deaths experienced in Canada. A high level of adherence to the recommended public health measures (PHMs) remained essential, especially when the Omicron variant of concern (VOC), which was associated with increased transmission and decreased vaccine effectiveness (primarily effectiveness against transmission) and some therapeutics, emerged.
Mitigating the impact of COVID-19 in Canada continues to require a comprehensive, integrated and cross-sectoral “whole-of-society”, “whole-of-government” strategy that focuses on what is within our span of control while trying to reduce the risk and impact of what is not. The context of our planning, therefore, is primarily Canadian-centric but recognizes that the global situation has a significant effect on our response activities, the risk of resurgence, and the duration of the Transition phase in Canada.
Omicron
The Omicron-driven wave highlighted the need for ongoing adjustments and tailoring of the response as the risk profile changes. The Omicron variant, although causing less severe disease among infected individuals, still threatened to exceed health care delivery capacity limits due to the sheer number of people infected with this highly transmissible, immune evasive VOC. Omicron arrived prior to the winter holiday season while considerable Delta VOC activity was ongoing and when a pandemic fatigued Canadian population was spending more time indoors, and gathering in large numbers. This increased the risk of transmission at a time when vaccine-induced protection had started to wane and booster dose programs had not yet been broadly implemented. To mitigate the risks associated with Omicron, booster dose programs were quickly expanded across the country and restrictive PHMs were re-instated, but were unsustained in many jurisdictions. Rapid antigen test use was expanded as overloaded public health systems largely shifted surveillance and testing strategies away from individual case and contact identification and management. Focusing on outbreak response in high-risk settings, and measures to reduce overload of health care systems due to community circulation of Omicron, became the priority in many jurisdictions.
Disproportionate impacts and societal consequences
From the start of the pandemic, Canada implemented extraordinary broad and restrictive community-based PHMs (e.g., school closure, restrictions on gatherings, workplace/ business restrictions). Restrictive community-based PHMs were maintained or re-implemented in many jurisdictions in response to Omicron. Many of these measures have had unintended negative health, well-being and societal consequences, Footnote 17 Footnote 18 Footnote 19 despite implementation of a significant level of societal support measures (e.g., income support, housing support, and expansion of social services such as mental health and food assistance).
The unintended, yet largely foreseeable, societal consequences of the pandemic response, have affected virtually the entire population. However, diverse groups within Canada have been disproportionately impacted by the pandemic, in part due to pre-existing inequities that were exacerbated by the pandemic. Footnote 20 Footnote 21 These groups include but are not limited to: older adults , essential workers, children and youth, racialized populations, Indigenous populations, people living with disabilities, women, 2SLGBTQI+ communities, people who use drugs, people living on low incomes , newcomers to Canada and people who are experiencing homelessness and/or under-housed. Footnote 22 Footnote 23 Footnote 24 As a result, their recovery as well as preparedness for future pandemics may require a more intensive and expansive approach that focuses on reducing inequities and building resilience.
Societal disruption
Societal disruption was associated not only with high levels of disease activity, but also the restrictive measures implemented to reduce transmission during these periods. The closure or reduced access to workplaces, businesses, schools and daycares, and recreational facilities, disrupted normal routines, and often created confusion as recommendations and requirements changed over time and differed between jurisdictions. Paradoxically, many of those experiencing these disruptions were those least at risk of severe disease (e.g., school aged children, healthy young adults).Footnote 25
Health care worker absenteeism from the workplace, due to the need to isolate or quarantine, further compromised already reduced health care capacity even in well resourced jurisdictions. Similarly, absenteeism amongst other essential service providers led to business continuity challenges.
The initial acceptance of necessary but disruptive response measures was impressive and beneficial as Canadians were learning about the impact of SARS-CoV-2 in our population and how best to reduce it. However, it is uncertain if the same level of personal sacrifice and societal disruption will be widely acceptable in the future. It is important that forward plans revisit the triggers and timing of measures implemented to reduce serious illness that also carry broader societal consequences. Even with the availability of economic and other supports, there is a limit to the public tolerance of these measures that are known to disrupt societal routines and functioning.
Risk framework
The WHO’s Pandemic Influenza Risk Management Guidance, encourages a risk-based approach to planning across a continuum of pandemic phases. The WHO phases (Figure 1) are intended to represent how the global incidence of cases (with all waves of pandemic activity collapsed into one pandemic phase) progresses over time and consequently provides a framework for the WHO's risk assessment of the global situation. This terminology, developed as part of influenza pandemic planning, has been less prominent during the COVID-19 pandemic, but still provides a useful context for transition planning. Specifically, this terminology and risk framework can be utilized at FPT tables to foster a Pan-Canadian approach to describing the current situation and planning by phase based on the level of pandemic, epidemic and ongoing level of disease activity in Canada.
Figure 1: The continuum of pandemic phasesFootnote 26
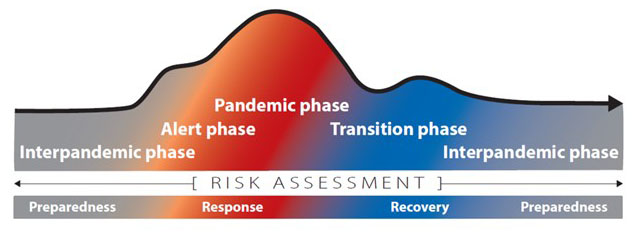
Figure 1: Text description
| Phase | COVID-19 incidence | Focus of activity |
|---|---|---|
| Interpandemic | Low, stable, predictable | Preparedness |
| Alert | Increased and less stable and unpredictable | Preparedness and response initiation |
| Pandemic | Waves of high incidence, low predictability | Response |
| Transition | Lower and stabilizing | Ongoing response, and recovery |
| Interpandemic | Low, stable and more predictable | Recovery and preparedness |
We carry out risk assessments through all pandemic phases.
The Transition phase is the phase between the acute pandemic response and the phase where COVID-19 is able to be managed like other common infectious diseases in Canada; the latter being the Interpandemic phase. The Interpandemic phase is not intended to represent the period between waves of pandemic activity; rather, it is the time between new pandemics which has ranged from 10-40 years for influenza but has not been established for SARS-CoV-2 since this is the first documented pandemic caused by a coronavirus. The WHO characterizes the Transition phase as the time at which “as the assessed global risk reduces, de-escalation of global actions may occur, and reduction in response activities or movement towards recovery actions by countries may be appropriate, according to their own risk assessments”.
Within Canada, federal and P/T risk assessments can now be informed by a substantial evidence base that when combined with local/regional epidemiological data, response experience and impact analysis, will help determine a risk-based approach for recovery and ongoing preparedness activities through the transition and interpandemic phases. However, uncertainty will continue to factor into risk assessments going forward since the emergence of VOCs with varied epidemiological characteristics need to be considered and the incidence and impact of COVID-19 during the Transition and Interpandemic phases will not be known until it is observed over a number of months to years. Given these caveats and recognizing that risk tolerance will likely vary between jurisdictions and over time, this document proposes planning based on achieving FPT objectives, using risk-based approaches for the use of measures and the communication of public health recommendations.
Response governance and concept of operations
Throughout the response the FPT Public Health Response Plan for Biological Events, has provided the framework for our FPT governance and concept of operations. This governance structure, which includes the Special Advisory Committee, Technical Advisory Committee (TAC), Logistics Advisory Committee (LAC) and Public Health Network Communications Group and associated secretariats has facilitated the coordination of the public health response. The frequent meeting of these groups have enabled real-time discussion of evidence, risk and strategic planning which has led to a robust response. These forums for developing broad recommendations, approving response related products (e.g., guidance, risk communications, operational protocols), assessing risk and information sharing, have been functioning at a “Level – 4 Emergency” FPT response level throughout the pandemic. As expected, provinces and territories (PTs) have adapted the FPT products and PHAC guidance products approved in these forums for use as needed in their jurisdictions. This has resulted in variations in the level of application and differences in timing of use of these products but nevertheless the structure has ensured thorough consideration and discussion of all aspects of the public health response.
As many PTs have now shifted into the Transition phase based on assessed risks and observed transmission levels, it will be important to consider whether (and when) the level of FPT response can be scaled back from a Level 4 - Emergency response to a Level 3 - Escalated response as part of forward planning. The concept of operations, supports ongoing review of the required FPT response level in the form of a feedback loop that includes ongoing monitoring of risks and necessary risk mitigation activities.
Previous waves
Before looking forward, it is important to think about the epidemiological characteristics and key drivers of previous waves, as these essentially are different scenarios that we have already faced and can potentially learn from the response to each. Specifically, there is a need to examine the triggers and timing of response measures implemented in each previous wave and subsequently, the impact these had on reducing serious illness, but also the societal consequences of the measures.
Figure 2 depicts the number of cases and prevalence of hospitalization due to COVID-19 in the Canada over time. Although influenced by testing capacity and policies, the data is sufficient to summarize the national trends in incidence and severity, recognizing that the impact of the waves varied between PTs. Each significant wave was driven by a change in variant and/or contact rates (i.e., degree of interaction between people outside of households). The impact of vaccination, which has included a relative reduction in severe disease (i.e., requiring hospitalization), is not clearly evident in the figure due to the underestimate of Omicron incidence. Also, testing in hospitals may have identified those with Omicron who were admitted for another reason which could affect the death data.
Figure 2: Pandemic waves and key drivers of COVID-19 impact
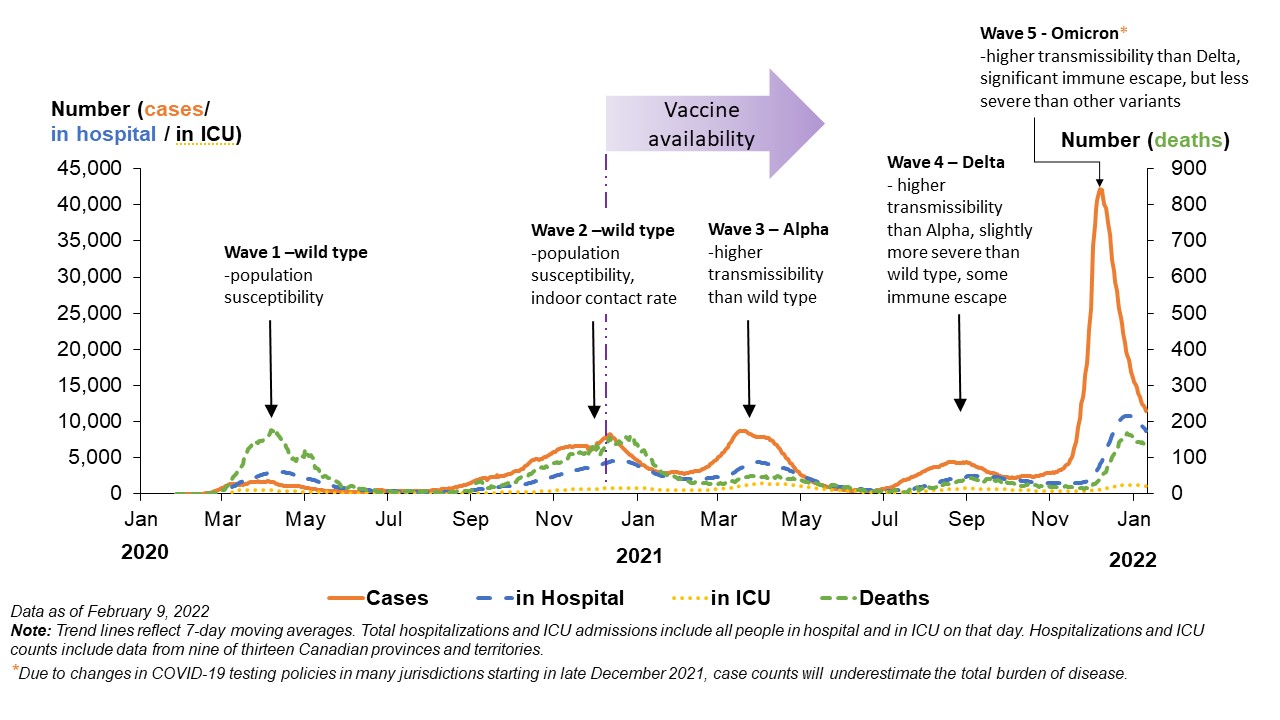
Figure 2: Text description
| Wave | COVID-19 type | Date range | Driver | 7-day avg peak incidence | 7-day avg peak | 7-day avg peak incidence |
|---|---|---|---|---|---|---|
| 1 | Wild | March to June 2020 | Population susceptibility | 1,373 (April 10, 2020) | 3,021 (May 11, 2020) | 177 (May 6, 2020) |
| 2 | Wild | September 2020 to January 2021 | Population susceptibility, increased indoor contact rate | 8,261 (Jan. 10, 2021) | 4,732 (Jan. 17, 2021) | 162 (Jan. 26, 2021) |
| 3 | Alpha | January to June 2021 | Higher transmissibility than wild type | 8,730 (April 17, 2021) | 4,396 (April 28, 2021) | 50 (April 29, 2021) |
| 4 | Delta | July to October 2021 | Higher transmissibility than Alpha Slightly more severe than wild type Some immune escape |
4,365 (Sept. 29, 2021) | 2,504 (Oct. 11, 2021) | 49 (Oct. 18, 2021) |
| 5 | Omicron | November 2021 to present | Higher transmissibility than Delta Slightly more severe than wild type (but less severe than other variants) |
42,191 (Jan. 6, 2022) | 10,839 (Jan. 26, 2022) | 168 (Jan. 26, 2022) |
Note: Trend lines reflect 7-day moving averages. Total hospitalizations and ICU admissions include all people in hospital and in ICU on that day. Hospitalization and ICU counts include data from nine of thirteen Canadian provinces and territories. Cases in ICU tend to follow the same trend as the numbers in hospital however there are not clear peaks and therefore not presented in the data table. They represent a small fraction of hospitalized cases.
Omicron footnote: due to changes in COVID-19 testing policies in many jurisdictions starting in late December 2021, case counts will underestimate the total burden of disease.
COVID-19 response goal and objectives
Goal
Canada’s goal for responding to the COVID-19 pandemic is based on that established for pandemic influenza in the Canadian Pandemic Influenza Preparedness: Planning Guidance for the Health Sector document (last updated August 2018). The goal is:
- To minimize serious illness and overall deaths while minimizing societal disruption as a result of the COVID-19 pandemic.
This goal has guided FPT public health response actions during the pandemic phase in Canada, with an emphasis on minimization of serious illness and death. Measures and strategies implemented with this goal in mind have helped reduce the incidence of COVID-19 in Canada and associated serious illness and deaths.
Reducing the health impact of COVID-19 while minimizing societal disruption has been extremely challenging especially as “pandemic fatigue” Footnote 27 Footnote 28 has increased and led to related challenges with respect to public adherence to recommended measures. Recognizing that some groups of Canadians face disproportionate barriers in their ability to adhere to these measures, has influenced the way local response measures have been implemented (e.g., off hour vaccination clinics for shift workers, mobile or pop-up clinics). Strategies to address these barriers will be an important lesson to carry forward for future responses and planning documents.
The goal statement, which highlights the need to balance the impact of COVID-19 in terms of both health outcomes and societal disruption, will lead to shifts in emphasis during the Transition phase. During periods of lower disease activity, the amount of serious illness should be manageable within our existing health care systems and with the use of therapeutics. Therefore, the use of measures that are known to have disruptive impacts in our society (i.e., restrictive measures) should be limited. However, given the ongoing risk of a virulent VOC with immune escape properties, there may be a need to re-shift the emphasis back to a focus on minimizing serious illness and death.
Objectives
As jurisdictions move out of the acute response phase and start to focus on recovery and preparedness for managing COVID-19 as a routine infectious disease in Canada, there is a need to revisit ongoing management objectives in the context of other public health priorities – many of which have not received adequate resources during the pandemic response phase.
Transition phase
The Transition phase is a challenging time. The risk of resurgence will remain uncertain, but must be planned for as the level of protection provided by vaccination and/or previous infection decreases over time in the Canadian population and while pandemic activity continues globally. There will be a need for multiple concurrent public health activities, all dependent on a largely exhausted public health work force, all in the context of ongoing uncertainties regarding new variants.
Reducing COVID-19 associated serious illness to a locally manageable level (i.e., that can be managed without disruption of other public health and health care services and programs), while maintaining surveillance and readiness for any resurgence, and strengthening risk assessment capacity, are key objectives during the Transition phase. However, during this phase there is also the need to concurrently address recovery activities, documenting “lessons learned” for future reflection, and starting to resume public health programs that were inadequately resourced due to the need to re-direct resources towards COVID-19 pandemic response and may have large unmet needs. This also includes starting to address ongoing health system capacity and data collection challenges. Any reliance on State of Emergency status to achieve the necessary support for the pandemic response should be considered and accounted for prior to discontinuing this declared State in order to ensure Transition phase objectives will be met.
The following public health objectives aim to mitigate risks during the Transition phase.
Approach:
- To take risk and evidence based public health action to reduce the morbidity and mortality of COVID-19 to a locally low, manageable and tolerable level, while minimizing or mitigating the negative physical and mental health consequences of these actions especially amongst populations in situations of vulnerability; and,
- To work collaboratively with the international community to support response and recovery in other countries.
Tools/measures/resources:
- To identify and address, with dedicated health resources, the unintended mental and physical health consequences and risks that have occurred over the course of the pandemic response, as part of current response and recovery activities;
- To continue delivering COVID-19 vaccination programs as recommended, in an efficient, equitable manner;
- To support the administration of therapeutics in an efficient, equitable manner;
- To use testing strategies and genomic surveillance to optimize the management of ongoing risks (e.g., to facilitate early treatment of those at high-risk of severe disease; to prevent introduction into congregate living settings; to detect potential VOCs; to assess wastewater as an indicator of community disease activity; to support targeted test, trace and isolate interventions, should a future variant have characteristics that justify doing so);
- To replenish and support access to vaccines, personal protective equipment, testing, and COVID-19 therapeutics as needed;
- To examine COVID-19 related risks in the context of other public health risks and re-balance resources as needed to identify and address priorities;
- To bolster positive individual health behaviours and facilitate incorporation of individual, business and institutional changes into everyday practices; and,
- To use mathematical modeling to help inform preparations for different epidemiological patterns that may occur during the Interpandemic phase in Canada.
Readiness:
- To ensure ongoing surveillance to facilitate early detection of resurgence signals and to inform risk assessments; and,
- To ensure readiness and capacity to respond appropriately to new risks (e.g., emergence of new VOCs) and manage ongoing residual risks.
Recovery and evaluation:
- To support recovery and physical and mental health of pandemic responders;
- To foster public understanding of ongoing risks while managing expectations for the recovery period (e.g., duration and potential need to re-implement pandemic response measures) and changes to improve resilience as COVID-19 transitions to an ongoing, more predictable, infectious disease in Canada; and,
- To document lessons learned and start forward planning aimed at improving future response capacity, efficiency and addressing response elements identified as gaps or weaknesses in after action evaluative reports/activities.
Within health care systems there will be a need to focus on clearing “backlogs” of services and care that was interrupted or delayed due to the need to re-allocate resources for treatment of COVID-19 cases and increasing future surge capacity. Canada’s research, surveillance, national collaborating centres, public health agencies, health care and laboratory systems will continue to provide necessary supports during the Transition phase.
Interpandemic phase
The onset of the Interpandemic phase will likely be identifiable only with retrospective data analysis. While coronaviruses routinely circulate and cause illness in the Canadian population, COVID-19 has newly emerged and therefore what the ongoing/stabilized epidemiology will be in the future is not yet known. For planning purposes it is important to consider different epidemiological patterns that may occur during the Interpandemic phase in Canada. Mathematical modeling and scenario based planning can help inform these preparations, however it is clear that monitoring the epidemiology of COVID-19 in the context of other diseases and ensuring a readiness to respond to signals of concern will be necessary on an ongoing basis.
Pandemic recovery activities may still be occurring during this phase, however, the focus should shift towards achieving preparedness-oriented objectives. During this phase it will be important to examine and implement broad improvements in public health and health care systems; particularly those that increase surge capacity and resilience. System-wide improvements that aim to reduce the disproportionate impact experienced by several diverse populations during the COVID-19 pandemic phase should also be prioritized as these improvements have the potential for immediate (non-COVID specific) benefits to health status. Furthermore, public health objectives in this phase should include addressing post-pandemic recommendations (“lessons learned”) and measures that not only improve capacity but also efficiency and timeliness of response components. Robust situational awareness and linkages across the health sector will also improve preparedness during this phase.
Upon reaching the Interpandemic phase, our public health objectives will shift to mitigate risks and improve preparedness for a broad range of risks. Anticipated objectives for the Interpandemic phase include:
- To ensure an ongoing state of readiness to identify risk signals;
- To prepare to mitigate risks to the extent possible through a cycle of timely, informed risk assessment, capacity assessment and preparedness activities;
- To build capacity and improve efficiency within the public health and health care systems to ensure ongoing health priorities are sufficiently resourced and surge capacity is available to address response needs for future epidemics and pandemics;
- To examine ongoing acquisition and stockpiling needs;
- To improve linkages (e.g., data, professional networks, research community) and connectivity across health sector to foster real-time data analysis and rapid scale-up during response periods;
- To modernize and improve efficiency of data management and risk assessment processes;
- To update pandemic guidance products aimed at preparedness, response and recovery with a focus on addressing elements identified as gaps or weaknesses in after action evaluative reports/activities (i.e., integrate lessons learned for the COVID-19 response); and,
- To work with other sectors to strengthen the social and economic services and policies that promote and protect health, prevent disease and build resilience (e.g., adequate housing, employment and income supports).
While not within the scope of public health planning, it should be noted that health care settings should also consider actions during the Interpandemic phase that will increase preparedness for infectious disease management in their settings. This could include revising and/or increasing training in infection prevention and control practices to be better protect health care workers and patients/residents from disease transmission and addressing infrastructure needs (including space and ventilation components).
Forward planning
Transition phase activities must simultaneously address: ongoing response, recovery and readiness needs in order to achieve the numerous objectives for this phase. Therefore, forward planning must be comprehensive with recognition that flexibility and nimbleness are critical since some needs may become higher priority than others at different points during the phase. Prioritization may also be necessary during this potentially long transition period, due to reliance on an exhausted and/or reduced public health workforce.
Planning assumptions and areas of uncertainty
This third edition of the plan aims to support consistent but flexible public health planning at all levels of government in order to support long-term COVID-19 response, recovery and readiness activities. Plans should reflect a combination of cohesive FPT approaches and objectives with regionally and locally adaptable actions; taking into account the needs of diverse groups within Canada on the basis of health status, age, gender, race/ethnicity, culture, ability status, and other socio-economic and demographic factors.
Table 1 identifies forward planning assumptions that aim to provide a basis for planning in the Canadian context following the Omicron-driven wave. The areas of uncertainty, listed in Table 2, help identify current unknowns and areas where the evidence base is rapidly expanding but is not at the point where it can support a planning assumption. Given these areas of evolving evidence and knowledge, operational plans need to include flexible elements or placeholders that can be updated over time and as knowledge and experience increase. Both planning assumptions and areas of uncertainty require validation and/or updating and may be triggers for re-visiting and modifying plans.
Table 1: Summary of planning assumptions
Forward planning assumptions
Epidemiology and risk:
- Transmission of COVID-19 will be ongoing, however the baseline level of transmission, as well as the impact, frequency or timing of resurgences are as yet unknown.
- COVID-19 adds a continuous net burden on health care.
- Epidemiology of the Transition phase could include surges in disease activity (due to outbreaks and/or new variants).
- Viral evolution is to be expected.
- Timing of phases (progression through and duration of) may vary between PTs and may not be a linear progression from response to transition to interpandemic.
- The proportion of infected individuals experiencing asymptomatic, symptomatic or severe disease could vary significantly based on the infecting variant. Transmission by asymptomatic and pre-symptomatic cases will continue to occur.
- The risk factors for severe disease will not change significantly over time (i.e., including with the emergence of new variants).
- There will be ongoing risk of internationally-imported COVID-19 cases that will vary with the global epidemic risk (e.g. the risk in neighboring countries, the level of global immunity etc.).
Impact and interventions:
- Public health management during the Transition phase will shift from a focus on requirements to recommendations and support for individual evidence and risk-based decision-making.
- A strong surveillance system is needed during the Transition phase.
- The vaccination strategy will continue to evolve based on new evidence, availability of new vaccines and related supply, and the epidemiological situation in Canada.
- Vaccination can reduce the incidence and impact of long-COVID.
- Recovery activities include addressing unintended consequences and risks, backlogs with health care systems and the impact of interrupted public health program delivery that have occurred over the course of the pandemic response.
- There is ongoing potential for emergence of new variants that may require a shift of focus from recovery actions back to response actions. This shift will be risk-based with consideration of other public health priorities.
- There will continue to be a Pan-Canadian approach to prioritization/targeting of any limited resource which will be based on an ethics framework. Policy development around prioritizing limited resources will also be informed by other logistical, epidemiological and societal considerations, for example the Declaration of the Rights of Indigenous Peoples.
- Response and recovery measures implemented in one jurisdiction could have an impact on neighbouring jurisdictions, even if they themselves do not implement that measure.
- Initiatives to address human resource and infrastructure needs will be required to build health care and public health system capacity.
- Ongoing/long term management of COVID-19 will require public health programs to mitigate surges in the demand for hospital resources.
- Determining an acceptable level of risk together with ongoing assessment of the global epidemic risk will inform ongoing management activities at international borders.
Immunity:
- A significant level of population immunity, together with PHMs and other measures will be required to reduce COVID-19 transmission to levels that are manageable without disruption to health systems and broader societal function.
- A variant that has significant genotypic and/or phenotypic changes (i.e., through mutation, recombination, or evolution from an earlier ancestor) compared to previously circulating SARS-CoV-2 variants, increases the risk of immune escape.
- Circulation of a variant with immune escape properties means that the proportion of the population that is susceptible to infection with this new variant will be increased.
- The level of immunity in the population (achieved through prior vaccination or infection) will wane over time.
- Circulating neutralizing antibodies and cellular immunity are key to providing protection against infection and severe disease, respectively, with other immune mechanisms contributing to each as well. Both are generally effectively induced by intramuscular vaccination, but vaccine-induced protection against variants may vary and protection, particularly against infection and also somewhat against severe disease, is expected to decrease over time.
- The level of protection received from vaccination will correlate in the short term with the number of appropriately spaced doses received and time from receipt of their last dose. This level may be affected by the immune competence of the individual, the intervals between the doses they received, the products received and the time since last dose.
- Infection stimulates the immune response (i.e., production of antibodies and cellular immune response), and is likely to induce mucosal as well as systemic immunity in immunocompetent individuals.
- Infection-induced immunity varies by a host of factors (age, severity of the illness, underlying medical conditions, vaccination status).
- Infection-induced immunity may offer good level of protection but compared to vaccination it is less consistent and predictable.
- Infection in addition to being vaccinated confers better protection than infection alone.
- Population immunity is function of the combination of individuals with varied levels of protection achieved through vaccination (with various products and/or combinations of products with varying effectiveness) and differing histories of prior infection.
Table 2: Summary of areas of uncertainty
Areas of uncertainty
- The epidemiology of COVID-19 endemicity in Canada- meaning the baseline level of transmission, as well as the impact, frequency or timing of resurgences (e.g., whether and when COVID-19 will eventually have a seasonal pattern similar to other respiratory infections).
- How ongoing circulation of SARS-CoV-2 will interact with other respiratory viruses (e.g., influenza, RSV), and the impact this will have on health care service demand during seasonal peaks and on population immunity.
- The epidemiology of other respiratory viruses after 2 years of limited circulation.
- The prevalence of Post-COVID Condition/Long-COVID in our population and the impact this sustained manifestation of COVID sequelae will have on morbidity, mortality, future health system resources, the workforce/economy and society in general.
- The level of COVID-19 morbidity and mortality considered acceptable/tolerable by the Canadian population.
- The level of PHMs that Canadians will tolerate and use of PHMs in the absence of mandates.
- The degree to which new variants will require adjustments to the response, recovery and ongoing preparedness activities in order to achieve objectives.
- The effectiveness of mucosal vaccines and whether they elicit better protection against infection and elicit immune protection against illness.
- There may be a limit to the protection received from repeated vaccination.
- Immune correlates of protection against infection or severe disease.
- How effective different current and new vaccines and therapeutics will be in response to new VOCs.
- The deleterious impact the COVID-19 pandemic response has had on the mental and physical health of Canadians, including those disproportionately impacted.
- How the deleterious impact the COVID-19 pandemic has had on responders might impact recovery efforts and future response capacity.
- Whether the lessons “observed” (i.e., not yet “learned”) can be addressed by current responders and effectively “passed on” to decision makers, the next cohort of responders, (e.g., students in health disciplines) and society at large.
- The extent of provincial and territorial formal review and inquiry processes.
- The extent to which the pandemic will catalyze change in various sectors to address social determinants of health and conditions for marginalized, racialized, Indigenous or harder to reach communities.
- The degree to which public trust in public health leaders, approaches and science in general has been negatively and positively impacted, and the duration of these impacts.
Planning for ongoing COVID-19 risks, response and readiness needs
Ongoing COVID-19 response activities and readiness for detection and response to resurgences of COVID-19, must continue to be addressed during the Transition phase. Throughout this period of transition towards more predictable COVID-19 disease activity in Canada it is important to consider that:
- the timing/specific characteristics of potential new variants is unpredictable, therefore transition to a relatively stable pattern of disease will likely take years, not months;
- immune escape variants can be expected to emerge over time – this may be a key driver of any increased spread, although increased intrinsic transmissibility is also possible;
- variants with higher severity remain possible and whether the intrinsic virulence of the variant causes an increase in observed severity in our population, will be determined by a number of factors (i.e., who is getting infected, residual protection from vaccination and past infections, and the effectiveness of tools and measures implemented);
- genetically-divergent variants could suddenly emerge (e.g., from zoonotic sources, evolution in immune compromised hosts); and,
- determining the epidemiology of a new variants will require time and will therefore challenge our ability to make timely risk-based decisions without a high level of uncertainty.
Population immunity
Population immunity will be considered significant when it is sufficient to decrease and sustain COVID-19 activity in Canada at a level where it can be managed concomitantly with other public health issues and without straining public health and health care resources. However, population immunity is a product of the combined immunity of all individuals in a population and to some degree the protective herd immunity effect when a high proportion of individuals are well protected at the same time (and mixing with unprotected individuals). Individuals will have varied levels of protection achieved through:
- vaccination - with products/combinations of products, with varying effectiveness, and in people with varied immune competence, and
- prior infection(s).
The protection achieved through vaccination or infection will wane over time and may be insufficient to prevent infection with a new VOC, as was seen with Omicron. For these reasons, there are multiple scenarios for the future of COVID-19 in Canada, and at this point it is not possible to predict with any certainty which scenario or combination of scenarios we will experience. This is not unique to Canada and similar conclusions have been reached by other countries. Footnote 29
Ongoing transmission
Given the shifts in the level of population immunity that can be expected to occur over time, ongoing transmission, due to imported cases, outbreaks and changes in contact rates amongst susceptible populations, is anticipated. It is also expected that waves of infection may continue to occur predominantly due to the introduction and spread of new variants. The frequency and amplitude of these waves of infection will depend on:
- the characteristics of the variant; in particular the degree of immune evasion will impact the size of the susceptible population and together with intrinsic transmissibility, the subsequent degree of spread, and
- the timing of, triggers for, and effectiveness of tools/measures implemented to reduce transmission and prevent serious illness and deaths.
Mathematical modelling supports planning our response to epidemics and outbreaks, and the COVID-19 pandemic has demonstrated the important role and need for the full range of modelling tools required to support decision-making during a complex public heath crisis. This role and the types of models currently in use are described in Appendix 1: Modelling Support for Forward Planning.
For forward planning purposes, it is helpful to think about a range of possible scenarios and the key drivers/characteristics of each; keeping in mind how the characteristics of the circulating variant (or variants) may manifest in Canada based on our level of population immunity at the time. Figure 3, depicts possible patterns of incidence, hospitalizations and the level of population immunity. The possibility of an “off season” wave is depicted in Figure 3 with a dotted orange line for case incidence and a corresponding dotted blue line for hospitalization prevalence.
Figure 3: Possible patterns of incidence, hospitalizations and population immunity
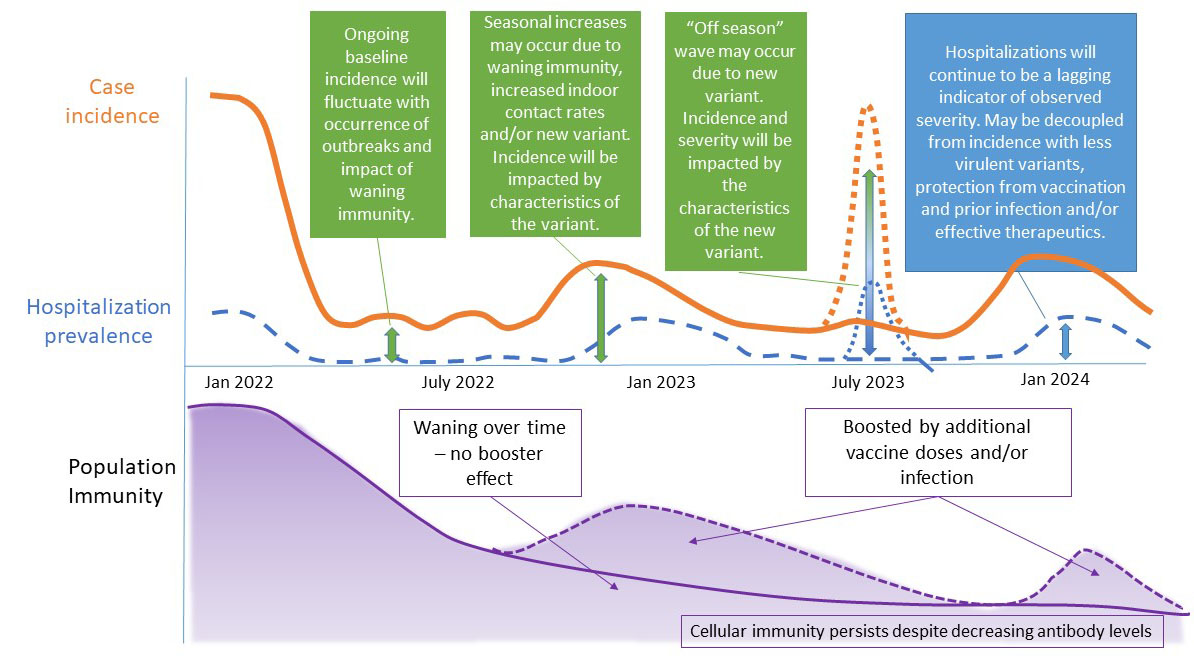
Figure 3: Text description
This figure is an illustration of possible patterns of case incidence and hospitalization prevalence, for the time period between January 2022 and January 2024.
| Time of year | Case incidence | Hospitalization prevalence | Population immunity |
|---|---|---|---|
Spring 2022 |
Low or declining after a winter surge in cases. |
Low/Medium |
Very high currently (following wave of Omicron cases and vaccination booster doses) |
Summer 2022, 2023 |
Ongoing baseline incidence will fluctuate with occurrence of outbreaks and impact of waning immunity. Always possibility of a resurgence due to a new VOC. |
Declining/low, unless there is an “off season” surge in cases that causes severe disease requiring hospitalization. |
Will wane slowing in the absence of vaccine boosters and/or infections. |
Fall/Winter 2022, 2023, 2024 |
Seasonal increases may occur due to waning immunity, increased indoor contact rates and/or new VOC (characteristics of new VOC would impact incidence). |
Would be a lagging indicator compared to incidence and may be decoupled from surges in incidence based on: virulence of circulating variant, protection from vaccination or prior infection and effectiveness of therapeutics. |
Will wane slowing in the absence of boosters and/or infections. A pre-fall vaccine booster may decrease incidence and/or hospitalizations. Vaccine effectiveness against circulating strain will influence. |
In Appendix 2: Epidemiological Drivers, the epidemiological drivers that influence: 1) the number and timing of new cases and, 2) health related impacts of cases, is presented for reference. (Note: this content has been retained from the 2nd edition of this Plan)
Observed severity
The number of hospitalized cases is one of the key variables used to represent observed severity in the population over time. This will be driven by the level of ongoing transmission in the population and the intrinsic transmissibility of the circulating variant(s). The observed severity of a new variant in the Canadian population will be a function of:
- the intrinsic virulence of the variant;
- who is getting infected (i.e., individuals with high-risk medical conditions, the elderly or low-risk, younger individuals) and who is not (i.e., due to residual protection from prior vaccination and/or infection); and
- the effectiveness of measures aimed at reducing severity and infection particularly amongst high-risk groups (e.g., evasion of therapeutics).
There is a role for the effective use of therapeutics, especially those that can be accessed and taken in the community early in an individual’s course of infection, which subsequently will impact the amplitude of the wave of COVID-19 related hospitalizations (see Figure 3). Pre-exposure prophylaxis with monoclonal antibodies for very high risk group who may not make good responses to vaccinations will also be available in the near future. Figure 4 identifies the 3 main drivers of observed severity in a population and highlights where public health action has the most influence.
Figure 4: Drivers of observed severity in a population
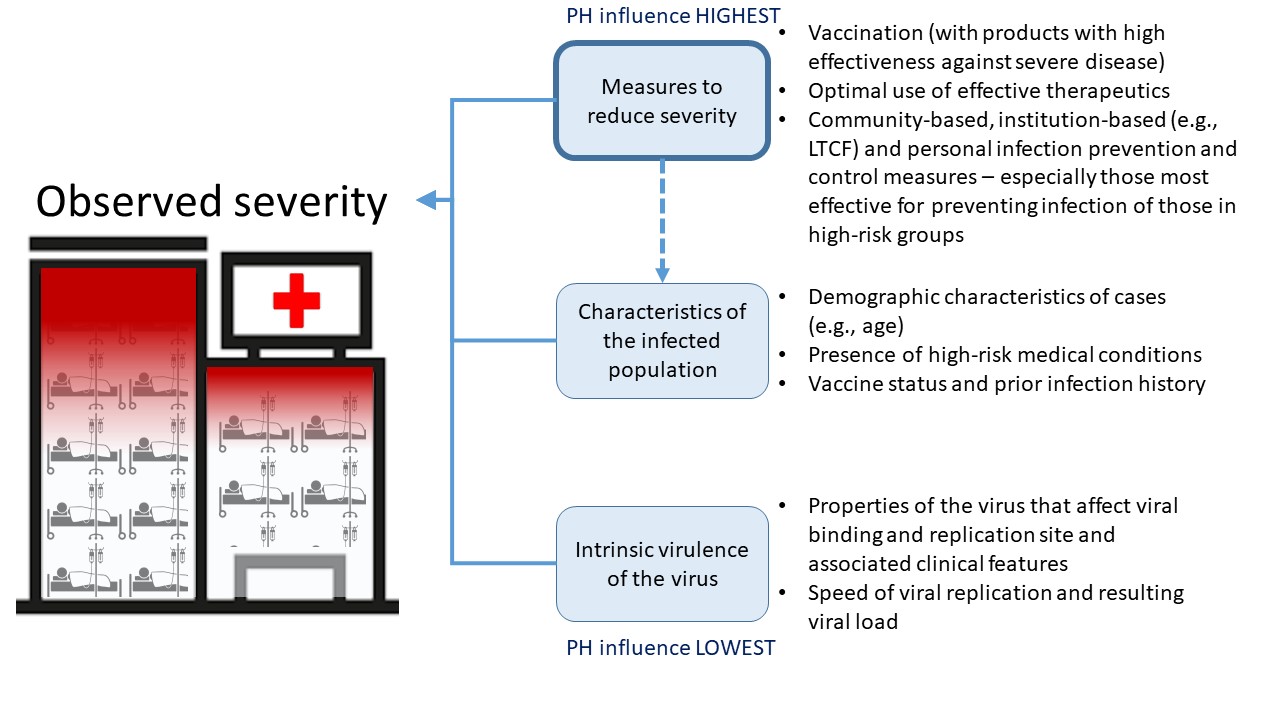
Figure 4: Text description
Observed severity is influenced by 3 factors in descending order of public health influence.
Measures to reduce severity:
- Vaccination (with products with high effectiveness against severe disease)
- Optimal use of effective therapeutics
- Community-based, institution-based (e.g., LCTF) and personal infection prevention and control measures – especially those most effective for preventing infection of those in high-risk groups
Characteristics of the infected population:
- Demographic characteristics of cases (e.g., age)
- Presence of high-risk medical conditions
- Vaccine status and prior infection history
Intrinsic virulence of the virus:
- Properties of the virus that effect viral binding and replication sites and associated clinical features
- Speed of viral replication and resulting viral load
Public health authorities have the greatest influence on the measures to reduce severity.
Serious outcomes of SARS-CoV-2 infection beyond the acute hospitalization period, specifically the Post-COVID Condition, also known as “Long-COVID”, also requires attention in forward plans. Public health authorities (PHAs) could play a leadership role in highlighting the need for, and facilitating funding of, research aimed at increasing the understanding of the epidemiology, including risk factors, for this syndrome. As more people experience this post-virus syndrome, necessary physical/rehabilitative and mental supports must be identified, quantified and used to plan for resources required for new programs and long-term management strategies. Collaboration across the health sector would facilitate a coordinated approach.
Risk management
Planning for the Transition phase, requires a risk management approach. As the epidemiology of COVID-19 in Canada becomes more stable and predictable, COVID-19 specific actions need to be transitioned into sustainable public health activities. Critical to this transition is ensuring that public health has the capacity to: provide informed, timely risk assessments on an ongoing basis that include but are not limited to COVID-19, and to response rapidly to signals of increased risk (e.g., severe VOCs). This risk management approach will help determine where to allocate and prioritize public health resources. It will also inform the need for system wide enhancements that will increase readiness and resilience for future pandemics.
While supporting and recognizing the interrelatedness of public health and health care delivery within our health care systems, the optimal public health response will be contingent on the ability to:
- rapidly assess new risks (e.g., new variants) - which includes monitoring the level of susceptibility and vulnerability in the population,
- mitigate the risk – by prioritizing and appropriately timing the use of highly effective, lower consequence measures, and implementing measures that are commensurate to the risk,
- minimize residual risk and response-associated consequences – which includes considering additional tools and measures that can lower residual risk as well as minimizing foreseeable, unintended, societal consequences of our responses
- evaluate impact of measures – to inform what worked well and what could be improved upon,
- scale up and down the response - based on the epidemiology of COVID-19 and related risks, with consideration of timing, triggers, effectiveness and risk tolerance
- increase the resilience in population and our health care systems – through addressing inequities in the social determinants of health, encouraging investment to improve surge capacity in both human resources and infrastructure, bolstering positive individual health behaviours and facilitating incorporation of individual, business and institutional changes into everyday practices.
Ongoing management of COVID-19 during the Transition phase includes ensuring the capacity to detect signals of resurgence, and the readiness to ramp up a response that is proportionate to the risk. Risk assessment is an important first step but the data needed to confidently inform the risk level is usually inadequate at the time the new signal is detected, especially if the signal is the emergence of a new variant. If the signal arises in another country, even if data is available on observed severity, the generalizability to the Canadian population and challenges with inferring intrinsic virulence from early population-level impact will remain Footnote 30. Genetic analysis of the variant may be helpful if there are mutations that are common to previously circulated variants but the ability to extrapolate population impact from these data will also be highly uncertain.
To facilitate readiness to respond in a manner proportionate to the risk, consideration of the viral characteristics and observed severity together with risk factors, can help inform which tools or measures to employ in the response. Content regarding planning for a reasonable worst case scenario has been retained from the second edition of this plan in Appendix 3: Planning for the reasonable worst case scenario, as it is still relevant and potentially applicable during the Transition phase.
Table 3 links these considerations with potential measures. Most non-restrictive measures will likely become recommended as opposed to mandated during the Transition phase. Therefore the role of public health will focus on empowering individuals to increase their resiliency by adopting individual health behaviours and make well-informed, risk-based decisions regarding what measures and protections to use and when, based on up-to-date evidence. This will involve doing: 1) a risk analysis as soon as possible after detection of a signal of concern, and 2) ongoing assessment of the risk factors identified in Table 3 in order to track the level of vulnerability in the Canadian population (e.g., due to waning immunity) over time, and 3) then providing credible advice to the public through risk communication activities. The list of tools/measures to mitigate the risks in Table 3 is intended to be illustrative not exhaustive.
Essential roles of public health and other government officials beyond encouraging individuals to conduct risk assessments and improve their protective behaviours is to strengthen societal structures through legislation and regulation so that there can be adequate testing, data collection, analysis and reporting, as well as enforcement of comprehensive border and travel health measures and opportunities for children, students, workers and other populations to have access to proper protective equipment and avoid exposure to coronaviruses.
| Viral Characteristic and Impact | Risk factors (level/degree of each affects risk level) |
Tools/Measures to mitigate |
|---|---|---|
Transmissibility - how much it will spread in Canada |
|
|
Immune escape - who will be vulnerable to infection |
|
|
Virulence - potential for severe disease due to viral properties and host response |
|
|
Observed severity - how much severe disease is experienced or could be expected (Note: this is influenced by the viral characteristics previously listed in this table) |
|
|
The risks of a variant with high intrinsic virulence, health care systems becoming overwhelmed, and the need to implement restrictive measures (which have known negative societal consequences and increase the risk of public backlash and lack of adherence to public health recommendations), are all connected. Forward planning needs to focus on the timing of, triggers for, and effectiveness of tools/measures implemented to reduce transmission of variants expected to have high observed severity in the Canadian population.
Timing
The timing of when to implement a measure, is usually based on an imminent risk or observed impact and the level of risk tolerance amongst decision makers and the public. In response to Omicron, measures were initiated before the impact of Omicron in our population was well understood. During the Transition phase we are now seeing pandemic fatigue, public risk perception and risk tolerance playing a greater role in the expeditious lifting of response measures.
Since most public health measures are preventive in nature, the effectiveness is usually affected by the timing of implementation. In short, the earlier after detection of a risk, the better. However, given the duration of the pandemic and the now known societal consequences of restrictive measures, there may be more reluctance to implement these types of measures early and broadly without strong evidence of observed severity in the Canadian, or a comparable, population. Individuals, equipped with public health recommendations, will likely take precautions when the risk is real to them or their friends and family. This will be too late for optimal population-based effectiveness.
Assuming there is no significant change in the population sub-groups at highest risk for severe outcome, it is likely that early implementation of restrictive measures will only be widely acceptable if they are targeted at, and known to be effective in, those at highest risk of severe disease and death. For example, targeting measures at settings where risk is likely to be greatest (e.g., long term care homes and other congregate living for older adults, as well as other high risk congregate living settings).
Triggers
The triggers for risk mitigation tools and measures will require consideration of how likely it is that the risk will be realized, what the potential severity of impact will be and the expected effectiveness of risk mitigation measures. Moving forward into the Transition phase it can be expected that decisions regarding the timing and triggers for action will include an element of risk tolerance, especially if expected severity is uncertain.
Triggers for public health action during the Transition phase will be based on the current epidemiology and subsequently, the demand on response resources and objectives of the response. Any significant change in response needs and requirements, which may or may not be able to be met with the existing capacity, may require adjustments in the public health response. Changes on demands for laboratory diagnosis, hospital treatment, or vaccines, could trigger an increase or decrease in response activity. For example, availability of vaccine for children triggered an increase in the number of clinics occurring in the community settings; whereas a decrease in laboratory capacity triggered a need for an increase in rapid test use and recommendations for self-care.
Similarly a change in emphasis of the response, for example to focus less on reducing transmission in the general population and more on protecting those at risk of severe disease, will also trigger a change in public health approach.
From an advanced planning perspective, the triggers for use of tools and measures should be based on a risk analysis that includes a focus on the risk of observed short-term and long-term severity, the risk of health care systems becoming overwhelmed, and the risk of societal disruption due to both disease and response measures implemented to reduce transmission.
Effectiveness
The effectiveness of any measure is highly variable and depends on the intrinsic properties (e.g., filtration capacity in a mask), whether it is consistently used properly (e.g., fit of mask) and at the population level, the uptake/adherence amongst the at risk proportion of the population (e.g., consistent mask use whenever in a public indoor setting). The relative effectiveness will vary between populations and over time, which is why timing and triggers are linked to effectiveness.
Recognizing that there are consequences of every measure both at an individual and population level, our experience to date has highlighted the need to balance the expected effectiveness of the measure against the possible negative consequences. Ideally, we all want highly effective measures with low negative consequences. Vaccination is one of the few measures that might be considered in this category. Therefore, forward planning for the public health response need to include:
- vaccine research and domestic production of vaccines,
- ongoing monitoring of the evidence base for the effectiveness of tools and measures,
- conducting research in the Canadian context to contribute to the evidence base,
- survey of knowledge, attitudes and behavior regarding measures to inform potential acceptance/uptake/adherence of recommended and mandated measures,
- evaluation the effectiveness of measures used during the pandemic, and
- examination of how to best to support adoption of effective behaviours at a population level.
Planning for recovery
In addition to ongoing response activities, the implementation of recovery-oriented activities is essential during the Transition phase. Planning for recovery in society includes addressing the broad consequences, backlogs within health care systems and the impact of interrupted public health program delivery, that have occurred over the course of the pandemic response. From a risk perspective, this involves examining COVID-19 related risks in the context of other public health risks, and re-balancing resources as needed to identify and address priorities. Recovery activities should include dedicating public health resources to address the broad, unintended mental and physical health consequences and risks that have occurred over the course of the pandemic response (See section 8).
Societal recovery
Given the uncertainties imbedded in the Transition phase, this will be an important time to foster public understanding of the ongoing risk environment while managing expectations for the recovery period (e.g., duration and potential need to re-implement pandemic response measures) and changes to improve resilience and mental wellbeing as COVID-19 becomes a persistent infectious disease in Canada. A part of this involves recognizing varying levels of risk tolerance in our population and the impact the information public health officials have provided to the public has had on how individuals accept and manage risk.
Many people have become more risk averse over the course of the pandemic and recovery for them may involve “normalizing” risk by providing reminders of what was tolerated previously and putting COVID-19 in the context of other daily risks. For those at higher-risk of severe disease (e.g., immunocompromised) the addition of SARS-CoV-2 as another pathogen that they need to beware of can be fear-provoking and overwhelming and therefore is likely best managed on an individual basis. At the other end of the spectrum, we now have people who feel confident in their understanding of COVID-19 risks to undertake, and make behavioral decisions, based on their own personal risk assessments. This type of empowerment is positive and public health facilitation of well-informed individual decision-making will be needed throughout the Transition phase.
Part of this transition back to more individual health decision-making and self-care, involves recognizing and respecting that people may make decisions that deviate from public health recommendations and that are not foremost in the interest of public health. Therefore, fostering recovery will include contextualizing risk and risk reduction measures for the population, while respecting individual differences.
Effective risk communication, in addition to ongoing knowledge translation and transparency, will be important to managing public expectations, facilitating evidence-based individual decision-making and maintaining public trust. Replenishing and supporting equitable access to effective vaccines, personal protective equipment and COVID-19 therapeutics as needed during this phase, will also mitigate the risk of future shortfalls and loss of public trust in our health care systems.
Societal recovery will require broad consideration and implementation of recovery activities adapted for population sub-groups and settings, for example: public health systems, health care systems, racialized communities, critical infrastructure, workplaces, schools, and congregate living settings.
Responder recovery
Planning activities are also needed to address the fact that the COVID-19 pandemic response has had a deleterious impact on the mental health of many responders (which include but is not limited to: public health workers, health care workers and social service providers). How this might impact recovery efforts and future response capacity is a major concern. Decreases in the available workforce have occurred due to burnout, early retirement, extended health/stress leaves and use of short-term solutions to supplement the workforce. There is also a need for the remaining responders to take time off work to recover, decompress and regain the energy required to continue to work in a stressful, often challenging, environment. Recovery efforts need to start with measures to improve the physical and mental health of pandemic responders, recognizing that this may be a prolonged need. This is necessary as some mental health conditions, such as post-traumatic stress disorder, may take months or even years to develop. Consideration should be given to increasing access to employee assistance programs (e.g., to all, not just full-time employees), and expanding the coverage available for counselling and other mental health services.
The period following an acute response often includes a series of inquiries, external evaluations and even legal challenges that require the same exhausted responders, expecting a reprieve, to continue work under potentially stressful conditions. It is important to recognize and prepare responders for this disheartening and challenging reality as this is difficult to avoid. Strategic planning for how to lessen the load on any one individual or team and be more efficient in terms of meeting these ongoing demands is needed.
This is also a time where changes to the workplace would be beneficial to ensure access to proper ventilation and protective equipment in the event of continued transmission of variants. Many workers, who were working virtually/remotely, may be anxious about returning to their designated office in person while those who routinely work virtually from a remote location may feel more disconnected and less well supported than they did when the majority were working virtually.
Planning with Indigenous communities
In response to the COVID-19 pandemic, Indigenous Services Canada (ISC) has provided or supported primary health care and public health services in First Nations and Inuit communities (see Appendix 4). For example, ISC provided access to personal protective equipment (PPE), supported communities in acquiring temporary assessment, screening, and isolation structures, assessed and supported re-opening of schools and other public facilities, provided surge capacity to address additional mental wellness needs, testing and contact tracing, and worked alongside provinces and territories, and Indigenous organizations, to prioritize access to vaccines for Indigenous people across Canada.
While First Nations living on reserve and Inuit living in land claim regions originally experienced lower rates of COVID-19 than the general Canadian population, First Nations, Inuit, and Métis had higher infection rates during the latest wave dominated by the Omicron variant. Urban First Nations, Inuit, and Métis have also been overrepresented in COVID-19 case counts throughout the pandemic.
Currently the most recent wave dominated by the Omicron variant is subsiding across the Indigenous population. Decisions made by Indigenous communities, regarding the lifting of health restrictions at the same time as many of their provincial and territorial counterparts, vary according to the local context and case rates. The vaccine rollout across Canada continues to prioritize access and allocation for Indigenous Peoples, and the uptake of vaccines has been largely successful, especially in light of vaccine hesitancy as a result of mistrust in the government due to colonial practices. As of February 15, 2022, 87.6% of First Nations living on reserve aged 12 years and older have received at least two doses of the vaccine.
While a full evaluation of the pandemic and response is a vital task to be undertaken during or following the Transition phase of the pandemic, some lessons learned have already become apparent. These include:
- the need to continue to work with Indigenous partners to prioritize Indigenous knowledge, lived experiences, priorities, and concerns around health and healthcare;
- the need to continue to work to gain trust from Indigenous Peoples and communities in order to effectively provide both primary and public health care services;
- significant discrepancies in social determinants of health is an increased risk for Indigenous Peoples with respect to both incidence and severity of communicable disease, particularly for respiratory illnesses; and,
- preparedness for health emergencies and pandemics and the ability to move quickly and flexibly allows a response to meet the distinct needs of First Nations, Inuit and Métis. This preparedness includes funding flexibility, access to PPE and medical supplies, timely knowledge translation, timely Indigenous (and non-Indigenous) language translation services, and health care personnel surge capacity.
Focus for transition phase
As Canada moves into the Transition phase of the COVID-19 pandemic, First Nations, Inuit, and Métis will have specific needs and considerations to be addressed in addition to those of the general Canadian population. Health equity gaps for First Nations, Inuit, and Métis populations are the result of colonial, historical, political, societal, and economic factors that have long influenced Indigenous health and Indigenous social determinants of health. Vaccination in the context of COVID-19 has shown, in several communities, the positive spin-offs of P/T collaboration with health and social services institutions as well as the added value of the cultural safety approach adopted by these institutions as part of their public health responsibilities towards communities and Indigenous Peoples. However, inequalities persist in part due to systemic racism experienced in the healthcare system and increased access to culturally safe services, as defined by Indigenous Peoples themselves, are required to support these populations. Important risk factors, such as higher rates of overcrowding and major repairs in homes, and inadequate resources to improve built environments, have the potential to contribute to transmission. Additionally, the waves of increased cases across Canada have not necessarily occurred in the Indigenous population at the same time as the general population; this has increased the comparative difference in risk between Indigenous Peoples and the general Canadian population. The impacts of the pandemic were exacerbated by overcrowded housing and other deficiencies in their built environment. As a result, it is important to recognize that First Nations, Inuit, and Métis, may have distinct needs and objectives that could differ from the general Canadian population, and from each other. Nonetheless, key priorities are expected to include:
- continuing to prioritize access to vaccines and therapeutics (particularly those designed to mitigate severe disease and hospitalization) in order to reduce the greater burden of risk experienced by Indigenous Peoples;
- taking public health action to reduce the incidence, morbidity, and mortality of COVID-19 among First Nations, Inuit, and Métis populations to low levels, as determined by each community, in a way that minimizes the negative physical health and well-being impacts and impediments to each community’s ways of life;
- assessing and addressing the impacts of the redirection of resources (financial, personnel, and expertise) toward COVID-19 to the possible detriment of other public health services and primary health care delivery;
- addressing and catching up with the back-log of public health activities, particularly TB screening and testing, childhood immunizations, and STBBI screening that have been delayed during the pandemic;
- dedicating public health resources and providing community support to address the unintended physical health and well-being impacts of the pandemic and consequences of pandemic response that have in particular impacted First Nations, Inuit, and Métis given their historical and colonial experiences;
- remaining in a state of readiness in order to swiftly address the potential threat that possible new variants may pose to Indigenous communities;
- Providing access to trauma-informed and cultural competency training to public health surge staff and responders to ensure culturally safe and appropriate care is provided to First Nations, Inuit, and Métis;
- Supporting the assessment, investigation and identification of risks and hazards in the built environment (e.g. restaurants, schools, and long-term care facilities) so as to reduce transmission and supporting communities in mitigating and preventing those risks;
- ensuring ongoing surveillance to facilitate early detection of resurgence signals and to inform risk assessments;
- provide access to First Nations, Inuit, and Métis to COVID-10 surveillance data that is distinctions-based for decision-making by Indigenous leadership;
- supporting the recovery and well-being of Indigenous pandemic responders and pandemic responders supporting Indigenous people and communities;
- in partnership with Indigenous communities and organizations, developing future strategy and approaches for managing and responding to COVID-19 in the long-term, as it becomes a more predictable ongoing infectious disease in Canada;
- support the education of clinicians to be able to respond adeptly to future variants of COVID-19, and other novel pathogens as they arise;
- assessing and articulating the additional burden of risk placed on First Nations, Inuit, and Métis by ongoing COVID-19 as a result of colonial, historic, political, societal, and economic factors that impact social determinants of health;
- reflecting, analyzing, learning, and documenting lessons learned and developing a plan aimed at improving future response capacity and efficiency; it will also address response elements identified as gaps or weaknesses in evaluation reports/activities in partnership with Indigenous communities and organizations;
- fostering understanding of the ongoing risk environment while managing expectations for the recovery period (e.g., duration and potential need to re-implement pandemic response measures) and changes to improve resilience as COVID-19 becomes an ongoing, predictable infectious disease, in a sustainable way; and,
- evaluating community based testing capacity that has been established over the pandemic and plan for transition to testing for other pathogens and maintain readiness for future emerging diseases concern.
Planning variables and signals
There are several unknown variables as well as currently held assumptions that will change the course of actions that will be taken during the Transition phase. The assumptions are:
- COVID-19 will become an ongoing, predictable infectious disease in Canada; and,
- the ongoing evolution of the virus is assumed, and therefore additional variants of concern are considered likely, including those which may prove to be more transmissible or virulent.
Unknown variables include:
- The degree to which the relaxation of restrictive public health measures will increase the risk for resurgent secondary wave of Omicron cases or other variants of concern, and the degree to which that risk may be disproportionally borne by Indigenous communities.
- It is unknown if COVID-19 will eventually become seasonal in nature, as with other respiratory viral illnesses.
- The scale of the “backlog” of primary care and public health services that were not available to First Nations, Inuit and Métis individuals and communities during the height of the pandemic, and the resources required to address it is unknown, but can be assumed to be quite significant based on information from regions, communities, and care providers.
- The scale of the additional physical and well-being impacts caused by the pandemic and the pandemic response for First Nations, Inuit, and Métis and the resources required to address it is unknown but should be assumed to be quite high.
- The waning protection of vaccines over time, and their efficacy when novel variants of concern may arise.
- The Indigenous community self-determined acceptable level of COVID-19 incidence, morbidity, and mortality among First Nations, Inuit, and Métis, and the degree to which that tolerance may differ from the general Canadian population.
- The future response capacity available to support future needs during resurgences of COVID-19, and other illnesses to the trauma, moral injury, fatigue, and burnout faced by healthcare providers and other responders.
- The future response capacity of Indigenous communities given the collective trauma caused by COVID-19, “COVID-19 fatigue”, and the impact on physical health and well-being.
- The degree of trust First Nations, Inuit, and Métis may have in the federal government, provincial and territorial governments, and local public health providers, as well as public health, in general, has been improved or damaged during the ongoing response to COVID-19.
Transition planning and recovery
While it is understandable that the during the transition phase significant resources are directed towards planning, learning, and reassessing best practises for managing COVID-19 on an ongoing basis, as well as planning for potential other novel pathogens, it is critical to ensure that these important exercises do not draw resources away from the recovery period required within First Nations, Inuit, and Métis communities. Indigenous communities will face considerable challenges in addressing the backlog of primary care and public health services and will require additional resources in order to do so. There is a risk that inadequate support for Indigenous communities in addressing this backlog will further widen the gap of health inequities between First Nations, Inuit, and Métis and non-Indigenous Canadians. There is, however, an opportunity that appropriate support in addressing this backlog will both serve to decrease those inequities, and act to make steps toward decolonizing health services, as Indigenous leaders and organizations are invited to partner in this work.
Addressing the consequences of pandemic response
The response to COVID-19 over the last 2 years has yielded multiple diverse impacts aside from the successful reduction in serious illness and deaths experienced in Canada due to COVID-19. On the positive side, the need for strong public health capacity as part of the health care continuum is now more fully recognized and decision-makers, the media, and the public are now highly aware of the role and responsibilities of public health in pandemic response. Connectivity across the health system has also improved, but still requires more work in particular to support timely, evidence-based decision making for the Canadian context. There has also been an increase in public understanding of scientific concepts, particularly regarding immunology and epidemiology, and the use and trust in science as a basis for decision making. Similarly, public health literacy and understanding, as evidenced by widespread uptake of recommended public health measures, has increased in the population.
Furthermore, changes in workforce surge capacity (e.g., employment of foreign-trained health professionals), domestic manufacturing and infrastructure, and increased capacity and flexibility to work virtually from home, may prove to be positive long-term consequences of the pandemic response. Strengthened stakeholder collaboration and relationships were also noted across multiple levels. The accelerated development of online technology, tools and platforms such as schedulers for public to self schedule lab testing, vaccine scheduling, public access to lab results and apps which can be used for other health care needs in the future were also positive outcomes.
Some of the positive consequences, however, were also temporary or diminished over time. For example, initially there was an increased public trust in governmental decision-making and sense of unity as evidenced by large turnouts to mass testing, support for health care workers, and high adherence to recommended measures. However, as the pandemic progressed this seemed to decline as public trust began to erode and community divisiveness increased especially in certain populations whose employment and economic prospects were diminished. Footnote 34
Unfortunately, there are also many negative consequences, many of which affected specific segments of the Canadian population. These groups include but are not limited to: older adults, essential workers, children and youth, racialized populations, Indigenous populations, people living with disabilities, women, 2SLGBTQI+ communities, people who use drugs, people living on low incomes, newcomers to Canada and people who are experiencing homelessness and/or under-housed. These consequences of the response include impacts on childhood development, access to health services, mental health, family and gender-based violence, and social isolation and exclusion. Footnote 35 Footnote 36
Many of the negative unintended consequences of the pandemic response were the result of existing baseline inequities in Canadian society. Table 4 provides examples of some of the negative consequences, contributing factors and potential sources of data or evidence that could help inform the magnitude of the impact.
| Negative consequence | Contributing factors | Data/evidence sources (examples) |
|---|---|---|
Delayed diagnosis of treatable medical conditions |
|
|
Delayed surgical and medical treatment |
|
|
Domestic abuse, child safety |
|
|
Delayed child development/education |
|
|
Increased substance use and related harms, such as overdoses |
|
|
Increased levels of anxiety and depression |
|
|
Increased personal and societal economic burden |
|
|
Interruption of routine preventative health and public health services |
|
|
Health authorities and health care institutions need to identify priorities for immediate action – like the resumption of elective surgeries, non-COVID public health programs and full capacity operation of diagnostic services and community services and clinics, and allocate resources accordingly.
Public health planning going forward needs to ensure capacity to detect, assess and mitigate negative impacts that arose during the Pandemic phase; in particular, the consequences of the response that may be ongoing but not currently substantiated by robust data. The prerequisites for this capacity need to be identified (e.g., increase access and timeliness of data/evidence, cross-sector collaboration) and tangible deliverables need to be incorporated into work plans that extend well beyond the Transition phase. PTs have identified this as a priority; for immediate public health attention, for after action reviews, and for incorporation in future pandemic plans. Specific public reports on the various pandemic response consequences are now being produced in some jurisdictions. Footnote 37
The pandemic response goal to “minimize serious illness and overall deaths…as a result of the pandemic”, was intentionally phrased to recognize that a certain degree of non-COVID-19 serious illness and deaths, due in part to the consequences of the response itself, was unavoidable. The onus is now on PHAs to incorporate measures to address these consequences as a response component in pandemic preparedness guidance and response plans. PHAs also have a role in communicating to decision-makers, stakeholders and the public, the impact the social determinants of health have on population health and resilience. With the pandemic in the forefront of the public consciousness, now is the time to connect these dots using the measurable disproportionate impacts of the COVID-19 pandemic on the Canadian population to prevent increasing health inequities for higher risk populations.
The diversity and magnitude of the consequences observed over the course of the acute pandemic response phase requires a “call to action,” since addressing these challenges will require a cross-sector, all of society approach. Furthermore, it is important that the multi-sectoral, multi-departmental response to COVID-19 continues during the Transition phase in order to address these broad societal consequences effectively.
COVID-19 FPT response components
Forward plans and current actions will also be informed by ongoing reflection regarding what has worked well, what we have learned and what can be adjusted based on evidence and experience. The response components identified in the CPIP have been used in the COVID-19 response structure. In this edition of the plan each of the following components are addressed in dedicated appendices, to facilitate rapid access to the specific content.
- Surveillance (Appendix 5)
- Laboratory Response Activities (Appendix 6)
- Public Health Measures (Appendix 7)
- Infection Prevention and Control and Clinical Care Guidance (Appendix 8)
- Vaccination (Appendix 9)
- International Border and Travel Health Measures (Appendix 10)
- Health Care Systems Infrastructure (Appendix 11)
- Risk Communications and Outreach (Appendix 12)
- Research (Appendix 13)
With a focus on those actions requiring FPT public health leadership and consultation, these appendices provide details on the current status of FPT activities that are planned or already underway that will assist and expedite complementary planning in each federal government department, province and territory.
Assessment and evaluation
One of the objectives of the Transition phase is to document lessons learned and start forward planning aimed at improving future response capacity, efficiency and addressing response elements identified as gaps or weaknesses in after action evaluative reports/activities. How lessons learned will be addressed by current responders and effectively “passed on” to decision-makers, the next cohort of responders (e.g., students in health disciplines) and society at large, needs to be a part of this multi-faceted process.
Assessing and evaluating pandemic response efforts during the Transition phase, while recent and outstanding challenges are still front of mind, will help identify areas of improvement and prioritize future planning efforts. It is also vital, on an ongoing basis, to determine whether response activities have been effective and implemented efficiently and balanced appropriately to minimize societal disruption and negative consequences in addition to minimizing serious illness and overall deaths.
The FPT COVID-19 response governance structure, which includes the SAC, TAC and LAC, provides multiple fora for these discussions and opportunities for sharing of experience, lessons learned and identified best practices. More structured processes for assessment and evaluation, including in-action and after-action reviews should be considered at all levels of government and diverse sectors to inform forward planning and future pandemic preparations. Findings from formal audits undertaken by FPT governments will also be taken into consideration in future planning processes.
Appendix 1: Modelling support for forward planning
Modelling facilitates planning and informs ongoing readiness needs by exploring how possible ranges of parameters relevant to these issues affect the extent and impact of the pandemic in Canada. Modelling inputs require epidemiological data from surveillance and other sources, while outputs largely depend on the underlying assumptions. Forecasting models are best suited to inform what may occur in the coming 2-3 months, while modelling of scenarios provides additional information to decision makers for long-term planning regarding the potential impact of control measures.
Modelling recreates the essential components of pathogen transmission cycles from our understanding of the biology of the pathogens and their interactions with their hosts. Models help to predict where and when infectious diseases may emerge or re-emerge, and they can be used to explore the best methods or combinations of methods to control disease outbreaks or epidemics and protect the health of Canadians. Models can take into account new events during the course of the pandemic such as vaccination or emergence of new variants of concern.
For response to COVID-19, there are three broad types of model being used:
- Deterministic compartment models. These are Susceptible-Exposed-Infectious-Recovered (SEIR) type dynamic models in which the population is divided into “susceptible”, “exposed”, “infectious” and “recovered” classes. After encountering infection, individuals in a population move from one state to the next. This basic structure includes elements to model SARS-CoV-2 and impacts of public health measures, with more realism. These elements include compartments for isolated cases and quarantined “exposed” contacts from which onward transmission to susceptible people is limited or absent, compartments for asymptomatic cases that may or may not be detected by surveillance, as well as flows to “isolation” and “quarantine” compartments that allow variation according to different levels of public health effort. These models are used to inform broad policies at FPT tables, including i) estimating numbers of cases, hospitalisations and deaths; ii) estimating the effects of non-pharmaceutical interventions (NPIs), (physical distancing, case detection and isolation, and contact tracing and quarantine), iii) design of vaccination programs; iv) the design of programs to enhance “herd immunity” via use of antivirals/therapies in combination of vaccination; and v) estimating the effect of the emergence of new variants of concern on the disease transmission.
- Agent-based models. These are also SEIR models, and they can also be used to inform development of Pan-Canadian strategies. However, because they can simulate disease transmission with some detail in and amongst homes, work places leisure spaces etc., they are particularly useful for decision-making at an individual community level regarding effects of vaccination, needs for NPIs, and strategies for relaxing restrictive closures.
- Branching models. These simply assess what factors cause single chains of transmission to expand or become extinct. They are often used to assess the needs for controlling transmission in work places or importation of cases.
The PHAC has developed models that can be shared, and are constantly undertaking modelling to support decisions. The PHAC External COVID-19 Modelling Expert Group was formed in February 2020, and currently comprises 37 members from 21 universities across Canada, as well as 74 members from other Federal departments/organisations provincial/territorial public health organisations. The group comprises the majority of infectious disease modelling group leads in Canadian universities, and is capable of supporting modelling needs for decision-making.
Appendix 2: Epidemiological drivers
This content has been retained from the 2nd edition of this plan as it may serve as a good reference, particularly for new responders.
An epidemic curve pattern is one part of a planning scenario as it reflects the potential changes in the number of new cases occurring over a period of time (see Figure A2-1). To ensure optimal planning, it is important to consider not only the number of cases but variables that may shift the health and societal impacts of those new cases and subsequently possible surges that exceed current health care and public health capacity thresholds.
Figure A2-1: Epidemiological drivers: Incidence
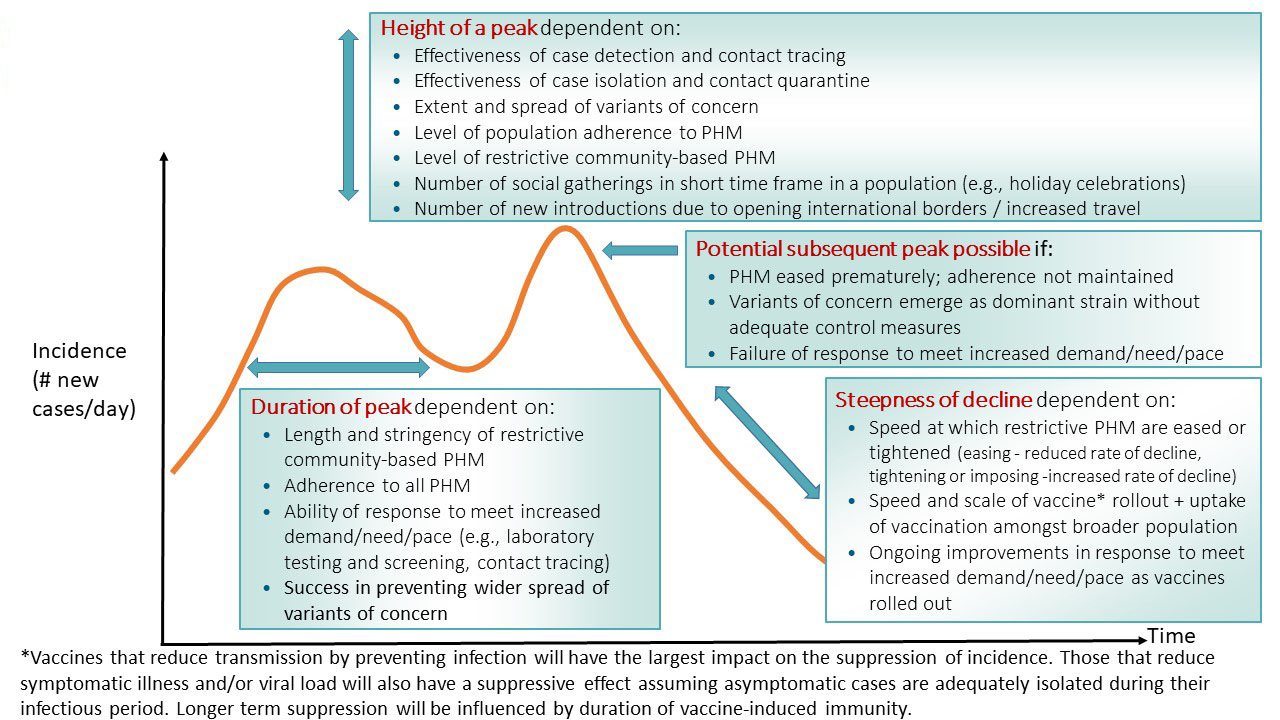
Figure A2-1: Text description
Incidence (the number of cases per day) depends on several factors.
Duration of peak incidence is dependent on:
- Length and stringency of restrictive community-based PHM
- Adherence to all PHM
- Ability of response to meet increased demand/need/page (e.g. laboratory testing and screening, contact tracing)
- Success in preventing wider spread of variants of concern
Height of a peak of incidence is dependent on:
- Effectiveness of case detection and contact tracing
- Effectiveness of case isolation and contact quarantine
- Extent and spread of variants of concern
- Level of population adherence to PHM
- Level of restrictive community-based PHM
- Number of social gatherings in short time in a population (e.g. holiday celebrations)
- Number of new introductions due to opening international borders/increased travel
A potential subsequent peak of incidence is possible if:
- PHM erased prematurely; adherence not maintained
- Variants of concern emerge as dominant strain without adequate control measures
- Failure of response to meet increased demand/need/pace
Steepness of a decline in incidence is dependent on:
- Speed at which restrictive PHM are eased or tightened
- Easing: reduced rate of decline
- Tightening or imposing: increased rate of decline
- Speed and scale of vaccine rollout and uptake of vaccination amongst broader population
- Ongoing improvements in response to meet increased demands/need/pace as vaccines rolled out
Vaccines that reduce transmission by preventing infection will have the largest impact on the suppression of incidence. Those that reduce symptomatic illness and/or viral load will also have a suppressive effect assuming asymptomatic cases are adequately isolated during their infectious period. Longer term suppression will be influenced by duration of vaccine-induced immunity.
Figure A2-2 describes epidemiological drivers of health impact in terms of variables that may increase or decrease the occurrence of severe illness and deaths due to COVID-19. These variables include but are not limited to: changes in severity of illness experienced by the majority of cases due to increased virulence, changes in high-risk groups (i.e., both the demographic characteristics of who is getting severely ill and identification of new risk factors for severe illness), the impact of variants of concern, availability of effective therapeutics and hospital care, and vaccine coverage. The manifestation of these variables will also influence public risk perception and therefore, in a somewhat circular manner, epidemiological drivers like adherence to recommended PHMs.
Figure A2-2: Epidemiologic drivers: COVID-19 related health impact
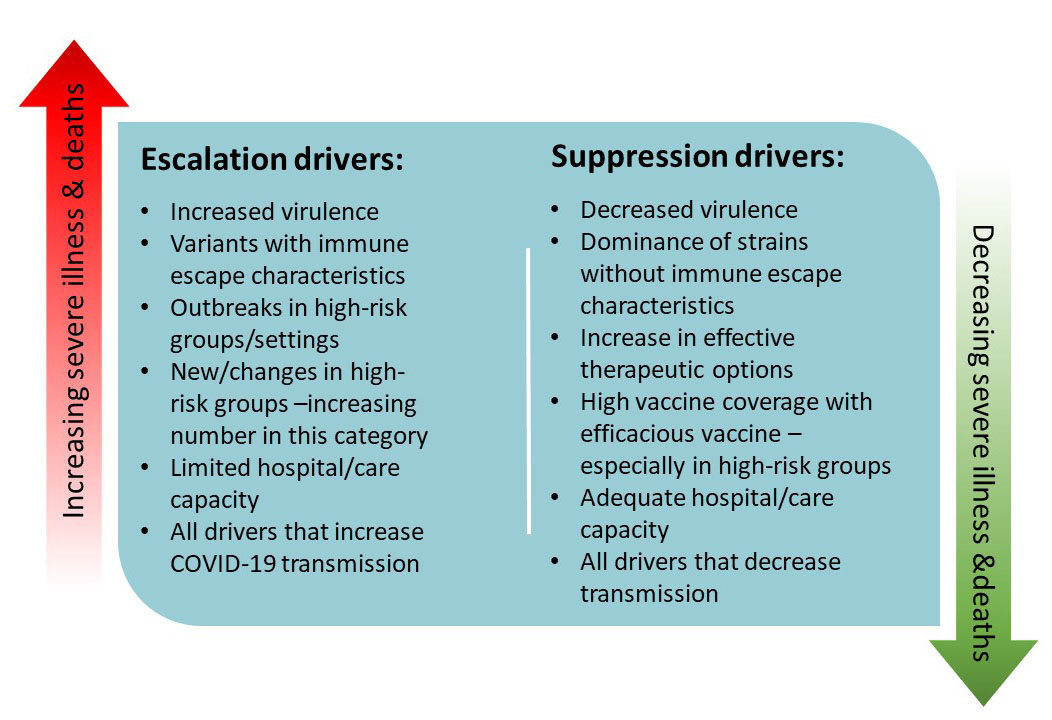
Figure A2-2: Text description
Escalation drivers that would lead to more severe health impacts:
- increased virulence
- variants with immune escape characteristics
- outbreaks in high-risk groups/settings
- new/changes in high-risk groups – increasing number in this category
- limited hospital/care capacity
- all drivers that increase COVID-19 transmission
Suppression drivers that would lead to less severe health impacts:
- decreased virulence
- dominance of strains without immune escape characteristics
- increase in effective therapeutic options
- high vaccine coverage with efficacious vaccine – especially in high-risk groups
- adequate hospital/care capacity
- all drivers that decrease transmission
Appendix 3: Planning for the reasonable worst case scenario
This content has been retained from the 2nd edition of this plan. Minor edits (e.g., removal of dates) have been made to make this a more generic reasonable worst-case scenario.
Reasonable worst-case scenario characteristics
- A large wave with a peak of prolonged duration followed by ongoing peaks of decreasing amplitude but several exceeding health care delivery, laboratory and public health capacity thresholds.
- Peak is similar or higher than the incidence experienced at the peak of the Omicron wave.
- Relatively high seasonal peak in winter occurs concurrently with severe influenza/other respiratory pathogens season.
- Similar timing of peaks across the country (each jurisdiction experiences peaks at same time).
- New VOC with high transmissibility, increased severity and immune escape properties becomes the dominant strain.
- VOC with immune escape properties reduce vaccine effectiveness.
- There is reluctance to take the licensed vaccines (or specific vaccines) or vaccine supply is insufficient or delayed, reducing vaccine coverage.
- Available vaccines do not significantly reduce transmission and do not confer long-term immunity.
- Available treatment/therapeutics are less effective against dominant variant.
- Weak/non-sustained post-infection immunity (recovered cases become susceptible again).
- Demand for health care resources (hospitalizations, ICU beds, ventilators, personal protective equipment (PPE), Long-term care spaces, etc.) exceeds system capacity (during wave peaks).
- Shortage of health care providers (e.g., due to illness, burnout, work refusal, international competition).
- Demands on both laboratory and public health resources exceed capacity (during all wave peaks).
- Low level of compliance with public health measures.
- Permeation of mis /disinformation in Canadian society and/or loss of public trust/confidence.
The generic reasonable worst-case scenario can be used to identify any new or outstanding preparedness and response needs or issues that would require, or benefit from, a coordinated FPT effort should Canada be faced with this scenario. It is provided as a “stress-test” not a prediction and is intended to stimulate thinking concerning our current response efforts, capacity thresholds and resiliency.
More specifically, the scenario presents a set of potential risks, each requiring mitigation strategies based on an assessment of capacity requirements and our capability to manage the risks. Figure A3-1 identifies high-level capabilities that need to be in place for this scenario and Table A3-1 identifies associated requirements that should be considered at all levels of government.
Figure A3-1: Capabilities for management of the reasonable worst-case scenario
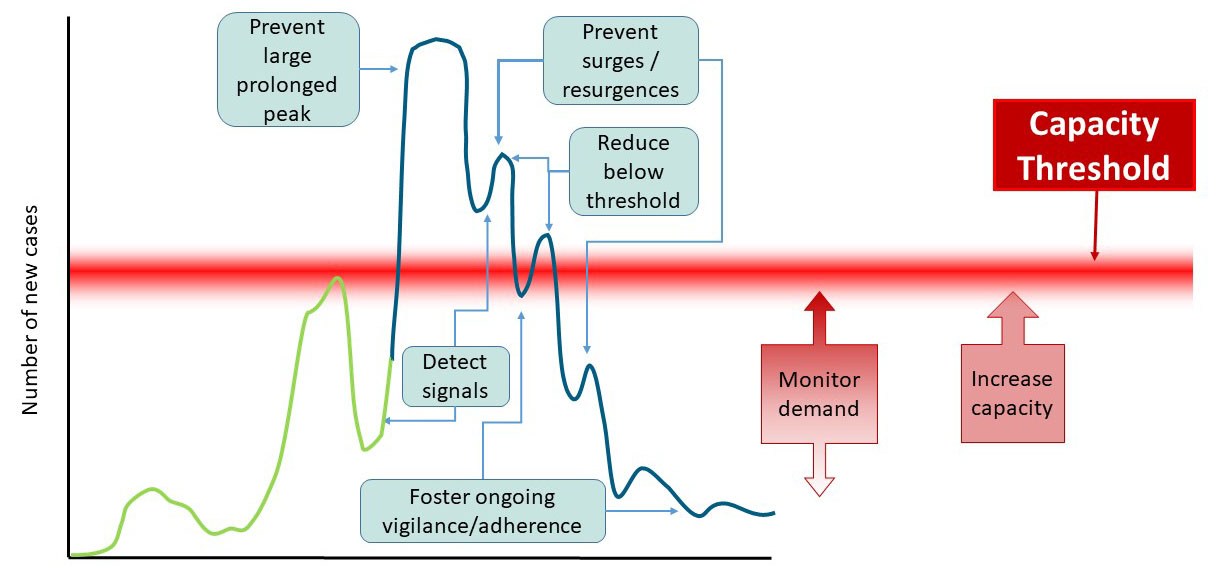
Figure A3-1: Text description
There is an ongoing need to monitor the demand on public health and health care resources. Increasing capacity to prevent breech of the capacity threshold is needed particularly when there is a signal that case incidence may rise to very high levels and/or a new variant may be highly virulent.
Managing the reasonable worst case scenario requires the ongoing capability to:
- Foster ongoing vigilance/adherence
- Monitor resource demand
- Detect signals
- Prevent surges/resurgences
- Prevent large prolonged peak
- Increase resource capacity
Table A3-1: Reasonable worst-case scenario risk management requirements
| Capability | Risk management requirements |
|---|---|
Detect: signals indicating a significant surge in cases may occur |
|
Prevent: large prolonged peak and surges, especially those that exceed capacity to respond |
|
Reduce: surges in incidence and hospitalizations |
|
Increase: health care and public health capacity |
|
Monitor: demand for health care resources |
|
Foster: ongoing public vigilance and adherence to measures and recommendations |
|
Appendix 4: COVID-19 response planning with Indigenous communities
Indigenous Services Canada (ISC), the Public Health Agency of Canada (PHAC) and the FPT response partners have been involved in various activities to support the COVID-19 response in First Nations, Inuit and Métis communities and partners, including the work of the SAC. These supportive activities are summarized below.
- Preparedness: Resources to support pandemic planning updates/activation; access to vaccines, medical supplies and PPE; training; and, guidelines. In the context of transitioning from the Pandemic phase of COVID-19 (to managing it as another infectious disease in Canada), all partners will continue to work to provide Indigenous communities the tools and resources needed in order to respond to ongoing clusters of outbreaks within communities.
- Health human resources: Resources to support community hired nurses and other health workers as well as to support surge capacity for health human resources, including nursing, medical and paramedical supports; as well as, charter services to get health human resources into communities. Indigenous Services Canada is currently working with its regional offices, FPT response partners and Indigenous partners and communities on a project to develop a surge response team of logisticians, epidemiologists, public health nurses and social workers. The surge team members’ primary focus would be deployments out to regions and communities that identify needs and capacity for public health response, surveillance, and mental health crisis support and response. Additional resources are also needed to provide for the logistical needs of these teams or community-hired personnel including infrastructure and housing.
- Infrastructure: Resources to procure temporary shelter solutions and to support communities in efforts to re-tool existing spaces to offer safe assessment and overflow space; and, additional surge supports for food, water and other supply chain components; coordination of chartered flights to ensure availability of critical infrastructure supplies and professionals.
- Infection prevention and control (IPC): Ongoing sharing of information (i.e., guidance on public health measures and promoting personal health measures for individuals and health providers), training and increasing capacity to support community response, including public service announcements in Indigenous languages. Provision of training of community workers and health providers on IPC. Ongoing funding for communities and service providers to increase their capacity for infection prevention and control, including First Nations-run schools, boarding homes, family violence shelters and friendship centres.
- Testing: Resources to develop capability and capacity to conduct COVID-19 testing including the provision of testing swabs, and rapid molecular and antigen point-of-care tests. In March 2020, the NML initiated the Northern, Remote and Isolated (NRI) initiative in collaboration with Indigenous Services Canada to build community-based testing (CBT) capacity in Indigenous and remote communities across Canada. This includes First Nation, Inuit, and Metis communities, organizations and service centres that are located in community or nearby communities that provide health services. This initiative was aimed at addressing the unacceptable turnaround time for diagnostic results experienced by people living in NRI communities, during the early phase of the pandemic. The NRI initiative is community-led, and enabled by the NML with the goal of ensuring that Indigenous communities have access to testing equivalent or better services found in major urban centres, with turnaround times to results available in under 1 hour. As of March 7, 2022, this initiative has seen diagnostic testing implemented in or near more than 300 Indigenous communities across Canada, with more than 2 million tests and devices for COVID19 distributed through the NRI initiative. The NRI will serve as a foundation for CBT for other infectious diseases (Tuberculosis, Hepatitis C, and others) beyond the current pandemic. This resource serves as a critical infrastructure for pandemic preparedness and outbreak response for Indigenous Peoples and hard to reach populations living in NRI sites.
- Public health advice and guidance: Have developed and are continuing to keep up to date advice and guidance to health professionals and communities that take into consideration the unique context of communities.
- Public facility control and prevention : Supporting high risk public facilities such as schools, day care centres, restaurants and long-term care facilities, in implementing of COVID-19 prevention measures. This included targeted inspections and assessments, and the provision of guidance, advice and training to community leadership, facility operators, and staff. Participation in technical networks to develop and apply building related interventions, such as ventilation, and to guide policy, program and funding opportunities. Indigenous Services Canada is continuing to seek resources to address the pre-pandemic service delivery gap and resulting backlog created from diverting resources.
- Governance: Continue to work with First Nations, Inuit, and Métis partners, the Public Health Agency of Canada (PHAC), Health Canada, Public Safety’s Government Operations Centre, and other departments, as well as their provincial and territorial counterparts for a coordinated and consistent Canadian approach to COVID-19 to protect the health and safety of all First Nations, Inuit and Métis, regardless of where they live in Canada.
- Communications: Continue to develop and broadly disseminate communication messaging through Indigenous Service Canada’s COVID-19 Single Window to networks with public service announcements in multiple Indigenous languages. Using digital media to further reach stakeholders with communications such as public health measures and maintaining an online, publicly available repository of COVID-19 resources relevant for Indigenous Peoples in multiple languages and formats. Multilateral calls with partners at the national and regional levels continue.
- Surveillance: Adaptation of the Department’s flu surveillance tool to track COVID-19 across First Nations communities; and development of a tracking tool to inform dashboards on key indicators of COVID-19. COVID-19 epidemiological and vaccination data is updated regularly on the ISC COVID-19 webpage. ISC continues to fund and facilitate partnerships with Indigenous-led, distinctions-based data initiatives. PHAC is working with provinces and territories to support collection of COVID-19 case and vaccination information, including race/ethnicity and Indigeneity to support understanding of the impacts of COVID-19 and inform response planning and actions.
- Vaccine response planning: Collaborating with federal departments, provinces and territories, and First Nations, Inuit and Métis partners to ensure that health facilities in Indigenous communities have the necessary immunization supplies, PPE, testing kits, and health human resources to deliver vaccines as needed. Facilitating a COVID-19 Vaccine Planning working group with representation from federal, provincial and territorial, and First Nations, Inuit and Métis partners to co-develop approaches to support the ongoing access to COVID-19 vaccines for Indigenous Peoples, including those living in urban settings. The work on vaccine access and response planning for Indigenous Peoples will continue from the Pandemic phase and into the Transition and Interpandemic phases, as needs arise for further doses in underserved populations due to variants of concern, and waning immunity, etc.
Based on knowledge and feedback learned to date, ongoing collaboration and funding is needed to support First Nations, Inuit, and Métis partners and their communities to respond to any future surges/resurgences. This includes continued access to timely testing supplies, P/T labs for processing, and results, including point of care testing for northern, remote and isolated communities and capacity to detect VOCs.
Access to care to treat more severe symptoms of COVID-19 in remote and isolated communities also requires that ongoing arrangements, or new ones, are in place to ensure an adequate number of beds in hospitals south of 60, to support the treatment of Indigenous Peoples living in northern, remote and/or isolated communities without this type of service. In communities where there are long-term care facilities, or Elders residences, it is important to have access to adequate resources to support their planning in keeping Elders safe and healthy, including funding for basic infection prevention control measures (i.e., PPE, high dose flu vaccine, cleaning supplies, etc.), as well as, developed public health measures.
Learning from H1N1 and now COVID-19, we know that long standing public health gaps and health inequities between First Nations Inuit and Métis, and non-Indigenous Canadians increase the likelihood and potential severity of a COVID-19 outbreak in Indigenous communities, and we have seen this throughout the pandemic, as well as in many cases, urban Indigenous populations. These inequities are exacerbated in remote or fly-in communities, where access to necessary supplies and health care services is limited as compared to non-Indigenous communities. We also know that during H1N1, data for First Nations, Inuit, and Métis were not captured in a consistent way, or a way that supported communities in their preparedness and response efforts. A distinctions-based approach has been adopted by the federal government to ensure that the unique rights, interests and circumstances of the First Nations, Inuit, and Métis are acknowledged, affirmed, and implemented. In this context, it takes into account the cultural and socio-economic realities of First Nations, Inuit, and Métis communities involved. Distinctions-based, Indigenous-led analysis of COVID-19 data is necessary to advancing culturally appropriate and evidence-based approaches, for First Nations, Inuit and Métis communities.
The strategy/approach, actions and deliverables for these preparations for the short, medium and long-term are presented below.
Short term: In the short term, ongoing work to continue to ensure First Nations, Inuit, and Métis communities and organizations have access to necessary supplies (e.g., PPE, vaccines and related administration supplies), human resources, and funding to support the COVID-19 response and planning for future waves. Vaccine planning is a priority in the short term and is being conducted through collaborative efforts in working groups to facilitate culturally safe and equitable access to the COVID-19 vaccine for all Indigenous Peoples, regardless of where they live in Canada. Communications regarding the vaccine are being developed and distributed in multiple Indigenous languages, in partnership with Indigenous leaders and organizations, to build vaccine confidence. ISC and PHAC continue to work with partners to advocate for the prioritization of Indigenous Peoples for access to the COVID-19 vaccine.
There is a need for continued work on COVID-19 surveillance and tracking of the COVID-19 vaccine administration, which is underway in collaboration with federal departments, provinces and territories, and Indigenous partners. Resources to support Indigenous-led data collection/governance/infrastructure to support data optimization for the longer term in Canada are essential. Resources to bolster community-led public health supports, culturally appropriate communication and information, and work are required, as well as training and capacity building to support these functions.
Medium term: As COVID-19 vaccine programs continue and the supply of the vaccine increases, the tracking and reporting of vaccine uptake and effectiveness will be critical. ISC will also continue to work with Indigenous partners to increase vaccine confidence, building on lessons learned from the vaccine rollout. Continued work is required to support access to patient care, as well as the work of community based workers and nurses in northern, remote and/or isolated communities, and increased funding for telemedicine and virtual health care providers is necessary. This work aims to reduce the anticipated backlog of medical or specialist appointments after the acute COVID-19 response phase, and support access to timely care supporting better health outcomes. Ongoing monitoring of forest fires and flood for possible evacuations and planning in light of COVID-19 will be maintained over the summer and fall months.
Longer term : During the Transition phase, ISC will work with partners to facilitate after action reviews that will inform emergency management funding and planning for future pandemics. ISC will be supporting health emergency management capacity in First Nations and Inuit communities through sustained funding for community-driven and designed health emergency management preparedness and mitigation activities. The department will also prioritize culturally-informed health emergency management capacity development and training opportunities with First Nations and Inuit partners.
ISC will also address the ongoing management of COVID-19 as an ongoing infectious disease with a possible seasonal pattern of increased incidence. Part of this management plan will include monitoring the high level signals that would necessitate a change in timelines or strategies and approaches and subsequent actions and deliverables. These include:
- community spread of new VOCs;
- ongoing and prolonged community outbreak scenario;
- signals and risks of community spread, where communities may be at a higher risk due to geographic location;
- access to health care to treat more severe symptoms;
- strain on system for medevacs;
- shifts in hospitalization rate, ICU admission rate, case fatality rate;
- post-COVID condition/long COVID;
- reproductive rate;
- outbreaks in long-term care facilities or Elder lodges; and,
- shift in age/sex distribution of cases.
This new continuum approach could cover the full spectrum of services from supports for people living with disabilities, to aging in place approaches, improvements to facility-based care, and services like those required by young adults that were previously served under the Jordan’s Principle. This continuum must address anti-Indigenous racism within health service systems and seek, as a matter of core principle, to eliminate health inequities for all Indigenous Peoples.
Finally, ISC will undertake a review, in collaboration with Indigenous communities, partners and organizations. The review will cover actions taken during the pandemic to learn about the challenges, , successes, weaknesses, strengths and opportunities in the approach taken, as well as to learn about the distinct ways in which pandemics may impact Indigenous communities differently than non-Indigenous communities. It will be important to work with Indigenous communities, partners, and organizations from the conception of this undertaking all the way through to the course of the review; this is critical in creating an opportunity to continue the effort to decolonize health care, and promote Indigenous self-determination within the field of public health.
Appendix 5: Surveillance
The purpose of surveillance is to provide decision makers with the timely epidemiological and risk information they need to inform action. Similar to national influenza surveillance (FluWatch), COVID-19 surveillance is a pan-Canadian initiative that integrates numerous data streams including existing surveillance systems with novel, non-traditional data sources. Ongoing COVID-related surveillance, is expected throughout the Transition phase with connectivity across health sectors to foster real-time data analysis to facilitate early detection of resurgence signals and examine COVID-19 related risks in the context of other public health risks.
Current status/focus
Currently, the following data sources enable monitoring of COVID-19 epidemiology:
- Case-level data reported by PTs: A national dataset including demographic, race/ethnicity, occupation, symptoms, clinical course and outcomes, exposures, vaccine history and variant lineage information for all confirmed and probable COVID-19 cases in Canada. This information used to monitor and describe the distribution of COVID-19 across priority epidemiologic factors.
- Aggregate laboratory result data reported by Provincial public health laboratories: numbers of positive tests and the number of tests performed to detect SARS-CoV-2. This information is used to measure the level of SARS-CoV-2 transmission in the community and to monitor the need for changes in community testing practices.
- Whole genome sequencing data reported by PTs: national genomic sequencing data detects SARS-CoV-2 variants, including VOCs.
- Aggregate sampling: Wastewater surveillance is underway and showing some promise as a surveillance and alert component at the regional level.
- Data on travellers and border testing: Used to identify new genomic variants and monitor trends at the border; thus facilitating early detection, situational awareness, and together with isolation and quarantine measures, the reduction of travel associated transmission in Canada.
- Special surveys: Impact of COVID- 19 on specific populations (e.g., health care worker).
- Sentinel Surveillance Networks:
- Hospital networks - Several hospital-based data streams measure the impact of COVID-19 in Canadian hospitals and collect detailed case information on most severe cases.
- Canadian Pediatric Surveillance Program - occurrence of Multi Inflammatory System in Children (MIS-C).
- Community-based systems/ networks - Assess the level of transmission in the community and the epidemiologic characteristics of outpatient cases.
- Publicly available data: supplementary data source to add situational awareness on COVID-19 transmission in jurisdictions and internationally.
- The federal, provincial and territorial public health partners are leveraging existing mechanisms and operating procedures to collaborate on multijurisdictional and complex COVID-19 outbreak investigations. This allows sharing of capacity and resources toward the goal of better understanding COVID-19 in our communities.
- Outbreak surveillance: systematically collates COVID-19 outbreak events in Canada through partnership with federal, provincial and territorial health authorities.
Preparations/forward planning
Forward planning will ensure that Canada’s surveillance strategy aligns with the public health management goals as they evolve through the next phases of the pandemic. Key changes to the public health management strategy with impacts on surveillance include: the withdrawal of population-level PCR testing and the reduction or elimination of public health follow-up of cases, which impacts data availability; and the relaxation of restrictive public health measures, which may have impacts on the epidemiology of COVID-19. As a result of these changes, alternative surveillance approaches are required to accurately inform timely public health policy and intervention decisions.
The surveillance strategy will focus on a multi-component/multi-pathogen surveillance model where applicable, with improved linkages and efficiency of data management. The focus will be on: i) monitoring, detecting and assessing signals of COVID-19, including the detection of variants of interest /VOCs; ii) monitoring and describing the clinical and epidemiologic features of severe COVID-19 infection (hospitalizations and deaths); iii) gaining a greater understanding of impacts of COVID and long COVID and populations at high risk for poor health outcomes; and iv) understanding waning of vaccine immunity. Multiple data streams are required to address these areas of focus: some existing; some requiring modification; and some new initiatives requiring implementation.
The preparations and ongoing activities based on the anticipated short, mid or long-term timeframe are identified below.
Short term:
- Establish Pan-Canadian surveillance goals and objectives, updated surveillance system framework (i.e., identification of data streams to retain, modify and develop), and revised surveillance guidance for the transition period
- Explore options for implementation or enhancement of sentinel or other community-based surveillance data stream(s) (e.g., cohorts) to compensate for reductions in public health follow-up of non-severe cases
- Monitor vaccine performance, including coverage, safety and effectiveness, waning immunity and vaccine escape.
- Transition from Genome Canada/CanCOGeN support to sequencing laboratories, to PHAC delivered support to integrated genomic surveillance and analysis
- Support operationalization of genomic capacity and screening strategies and continue to support mechanisms to facilitate linkages between epidemiological and laboratory data to monitor on-going viral evolution including VOCs.
- Further validation and integration, and use of wastewater testing as an early detection mechanism.
- Initiate planning for surveillance to identify broader impacts of COVID-19 and associated control measures on health of Canadians.
- Conduct scenario-based planning to identify signals that may arise, the surveillance information required to detect and characterize the signals, and the associated public health actions required to respond.
- Support rapid epidemiologic investigations to characterise the transmission and impacts of new variants and impact of vaccination in the context of outbreaks.
- Provide federal surge capacity support.
- Share timely information effectively with partners and publicly with Canadians.
Medium to long term:
- Support rapid epidemiologic investigations if there is a concern that a new variant is driving transmission (immune escape) and/or impacting severity outcomes.
- Monitor vaccine performance, including coverage, safety and effectiveness, including issues such as waning immunity and vaccine escape.
- Conduct targeted surveillance on broader consequences of the response to inform public health action.
- Enhance data integration to evaluate evolving epidemiology in the context of increased vaccination and immunity to support recovery.
- Continue to build and maintain data and analytics capacity and knowledge transfer networks to support on-going development and sharing of intelligence.
- Consideration of surveillance strategies for Post-COVID Condition/Long COVID.
- Integrate and operationalize wastewater genomic surveillance as a routine element of pathogen detection and tracking.
- Establish national reference center to enable monitoring for drug resistance for approved COVID anti-virals.
- Support the expansion of the current VirusSeq Data Portal for genomic data to support controlled access for collaborative FPT and Academic investigation to lab data and associated case data (pilot under Pan-Canadian Health Data Strategy).
- Consideration of strategies that could detect zoonotic and reverse zoonotic (zooanthroponosis) transmission. This could involve leveraging some of what has been established for human testing/response and human genomic surveillance and new mechanisms beyond referrals from wildlife agencies to the Canadian Food Inspection Agency’s National Centre for Foreign Animal Disease (CFIA-NCFAD).
Planning variables or signals
It is possible that a new syndrome or rare event would require the development of a new, or adjustments to, the surveillance strategy as has occurred for Multisystem Inflammatory Syndrome in Children (MIS-C).
New settings or populations affected by outbreaks could emerge in outbreak surveillance (or via outbreak intelligence gathering) which could precipitate new data needs, additional surveillance activities or new variables to be collected to inform actions. For example, outbreaks among temporary foreign workers have highlighted the need to be prepared to rapidly implement specific surveillance and coordination mechanisms, as well as drawn attention to how social determinants of health (e.g., crowded housing, precarious work, access to medical services) can impact transmission and control of COVID-19.
Surveillance strategy, capabilities and capacity, will focus on a multi-component/multi-pathogen surveillance model as Canada transitions to the next phase of the COVID-19 pandemic. With the expected withdrawal of population-level testing via PCR tests, alternative surveillance approaches are needed to accurately inform timely public health policy and intervention decisions.
Appendix 6: Laboratory response activities
Laboratory-based surveillance is an integral part of monitoring respiratory virus activity. Since the start of the COVID-19 outbreak, Canada’s National Microbiology Laboratory (NML) has been providing leadership in regard to testing for COVID-19 and surge capacity for provincial and territorial public health laboratories. The NML has also contributed to domestic and international efforts to better understand COVID-19 virus characteristics that can inform the development of medical countermeasures.
The NML, Indigenous Services Canada and CPHLN have worked closely and successfully with northern, remote, and Indigenous communities to enable those communities to have greater access to laboratory diagnostic tools (e.g., point-of-care, diagnostic platforms, reagents, training). Through collaboration with the NML, the territories have been able to set up COVID-19 testing within each territory.
Canada’s genomic surveillance capacity has increased exponentially in response to the COVID-19 outbreak. Provincial and territorial involvement in the sequencing efforts across Canada through the Canadian COVID-19 Genomics Network (CanCOGeN) has greatly enhanced genomic sequencing throughput. Ongoing communications with partners within industry, academia, and various government levels have fostered a collaborative approach to sequencing and monitoring novel virus variants. The National Microbiology Lab (NML) plays a lead role in supporting and guiding these efforts at all levels, including through laboratory and bioinformatic analyses.
Wastewater-based surveillance of SARS-CoV-2 has emerged as an innovative tool to complement clinical epidemiology and testing data and is a rapid and cost-effective approach for early detection of outbreaks and surges as it monitors the circulation of variants of concern. The Public Health Agency of Canada (PHAC), through the National Microbiology Laboratory (NML), developed a Pan-Canadian Wastewater Surveillance Network with key partners and programs across different government levels (federal, provincial, territorial, municipal) and academia to sample and test wastewater for COVID-19 from a large number of municipalities across Canada.
Current status/focus
The Omicron-driven wave of the pandemic caused cases to surge, with testing demand exceeding available laboratory capacity in most jurisdictions. In response, most P/T jurisdictions limited the use of PCR testing to diagnose COVID-19 to specific target groups, including the unvaccinated, immunocompromised, or those working or living in high-risk settings, with public health testing guidance varying between jurisdictions.
Rapid antigen detection tests (RADT) are increasingly being used to support self-testing and case detection. RADTs are comparatively less sensitive than RT-PCR-based testing, but may be appropriate for screening purposes in higher prevalence settings where timely access to RT-PCR testing is limited. The positive predictive value of RADTs will decrease as the true prevalence of infection in the target population decreases.
The evolution of novel virus variants with altered characteristics has been observed, including increased transmissibility and partial immune escape, posing new challenges to Canadians. Canada’s public health laboratories, working through the CPHLN, are meeting this new challenge while continuing to address other key COVID-19 and non-COVID-19 pressures through the following activities:
- development and validation of diagnostic VOC screening assays;
- updating of FPT screening and sequencing guidance for SARS-CoV-2 variants;
- continued support for acceleration of whole genome sequencing and improvement of timeliness of analysis and communication of variant information;
- transition of support to PT sequencing laboratories from initial capacity building through CanCOGeN to sustainable operation through NML support undertaking genomic surveillance efforts to monitor the emergence and prevalence of VOCs within Canada, including through border surveillance initiatives;
- acquiring VOC samples to support Canadian diagnostic initiatives and research, including the assessment of vaccine efficacy in the face of evolving variants;
- continued work to evaluate serological testing kits as well as developing in-house serological tools such as ELISA, neutralization assays and point of care tests (serological work is in support of the broader Canadian Immunology Task Force), incorporating the ability to distinguish natural infection from vaccine-derived antibodies;
- collaboration with other partners, such as CIHR and academic, to undertake studies that help us understand pathogen characteristics, including the differences brought on by virus variants;
- continued readiness to tackle multiple respiratory virus outbreaks as needed, recognizing that the PHMs in place have largely suppressed influenza and RSV activity but a resurgence might be observed with the relaxation of PHMs;
- continued growth of the Pan-Canadian Wastewater Surveillance network through various federal, provincial, territorial and academic collaborations (currently almost 60% Canadian population on sewage treatment systems is covered).
Preparations/forward planning
During the Omicron wave, access to molecular testing in most provinces and territories was constrained due to very high case numbers. Many provinces and territories are continuing a shift to rapid testing and individual responsibility for limiting the spread of COVID-19. This means reduced availability of population-level surveillance testing with PCR tests that can then be used for genomic surveillance. Efforts will be needed to transition to targeted surveillance (e.g., hospitals, primary care, and borders) while also ensuring a minimum level of testing of a random selection of samples from communities.
The NML together with the CPHLN, is undertaking the following activities in order to continue to prepare for potential surges/resurgences based on the reasonable worst-case scenario but also as part of the laboratory preparedness long-term vision.
The Pan-Canadian Wastewater Surveillance network needs to be expanded further to cover more Canadian population especially those in Northern, remote and isolated areas.
Short term:
- Continuing strong communication among Canada’s public health partners through CPHLN to ensure laboratory response strategies are aligned and appropriate.
- Continuing a strong collaborative approach toward developing and validating diagnostic testing.
- Provide support for point of care testing.
- Work together to develop a robust collaborative research agenda into SARS-CoV-2 variants of concern, their detection and public health impacts as vaccines are administered.
Mid term:
- Continue optimizing various testing platforms and their uses to determine whether individuals have been previously infected, especially for healthcare and other service providers such as police, fire fighters, employees in long-term care facilities, etc.
- Continue streamlining molecular and serological testing as well as variant screens and whole genome sequencing, including stewardship of reagents so they are conserved as testing demands increase.
- Continue developing, validating, and enabling greater access to faster diagnostic tools such as Point of Care tests and self tests (prioritizing northern, remote, isolated and Indigenous communities).
- Continue working with PTs and other stakeholders to inform the use of testing in specialized settings (such as borders).
- Create a sustainable wastewater-based epidemiology program.
- Ongoing assessment of RADT performance characteristics and sample approaches; address gaps in PH reporting of positive cases identified via RADTs; provide updated guidance regarding the use of RADTs for the identification of SARS-CoV-2 infection.
Planning variables or signals
Epidemiological data from January 2022 are beginning to demonstrate declines in case counts in most Canadian jurisdictions, but with the combination of relaxation of public health measures, the very high transmissibility of Omicron, and the expectation that additional high-transmissibility and immune escape variants, effective genomic surveillance will be required. Early identification, detection and tracking of additional variants will continue to be a priority as we move into the inter-pandemic phase.
Appendix 7: Public health measures
PHMs are the range of non-pharmaceutical interventions implemented by individuals and PHAs at the FPT and local level to reduce the risk of infectious disease transmission. PHM range from those applied at the individual-level to community-based measures implemented in non-health care community settings (e.g., schools, workplaces/businesses, gatherings and events).
Individual-level PHMs include actions that individuals can take to protect themselves and others, including wearing masks, physical distancing, improving indoor ventilation, practising hand hygiene and respiratory etiquette, self-monitoring for symptoms and staying home when sick.
Community-based measures range from public education campaigns, case and contact management activities, and mask mandates; to restrictive measures to reduce interactions and prevent transmission in population groups, settings and the community at large. “Restrictive” community-based measures aim to reduce contacts by limiting movement, activities, or access to resources and public spaces. Examples of such measures include: school closures, restrictions on gatherings, workplaces/businesses restrictions or closures, inter- or intra-provincial or territorial travel restrictions, and curfews).
PHMs have been shown to be effective in controlling transmission of COVID-19 even where VOCs with increased transmission are dominant. 9,10 However, many of these measures have important consequences that must be considered in public health decision-making. These consequences require careful consideration and prioritization in relation to other determinants of health, such as impacts on childhood development, access to health services, mental health, family and gender-based violence, social isolation and exclusion, and at-risk communities. PHM effectiveness depends on the level of adherence by the public, which is influenced by pandemic fatigue and factors such as living, working, community conditions, and financial and social circumstances.
Since the start of the COVID-19 pandemic the FPT public health response has involved working closely with multilateral partners, other government departments, and First Nations, Inuit and Métis partners to develop, update and disseminate appropriate public health guidance for a range of target audiences on how to detect, report, prevent and manage COVID-19 infection. One example of this is the formation of the Public Health Working Group on Remote and Isolated Communities that adapts public health measures guidance to the unique needs, context and considerations of these communities in the response.
Currently, PHAs continue to adjust (re-instate, maintain, ease) PHMs in response to local circumstances as the pandemic evolves, including the emergence of new COVID-19 variants that have the potential to be more transmissible, cause more severe disease, or have known or potential for vaccine immune escape. During the Transition phase it will be important to maintain readiness for new VOCs, seasonal resurgence, decreased protection against infection over time, and community outbreaks among populations at high risk of poor health outcomes. As part of readiness activities, effective public risk communication regarding these possibilities will be needed in order to prepare the public for any corresponding adjustments in the use of PHMs.
Focus for transition phase
The focus during the Transition phase includes:
- ongoing updates to existing or development of new FPT and/or PHAC guidance as evidence evolves;
- continuing to provide advice to the public on how to assess and mitigate COVID-19 risks, and fostering public understanding of the on-going risk environment;
- collaborating with FPT stakeholders on pandemic recovery and adjusting PHMs as required;
- highlighting current guidance for adjusting PHMs
- normalizing individual-level PHMs so that they may become a part of everyday practices to help reduce the risk of transmission of COVID-19 and other respiratory viruses (e.g., staying at home when sick, improving indoor ventilation, hand hygiene, respiratory etiquette, cleaning and disinfecting);
- continuing to promote the use of additional layers of protection (e.g., wearing well-constructed and well-fitted masks or respirators, physical distancing, avoiding or limiting time spent in closed spaces and crowded places) across jurisdictions and normalize their use, particularly among higher risk populations/settings. Individual use of these measures should be based on a personal risk assessment which considers local COVID-19 activity and individual risk factors;
- continuing to monitor the situation to identify triggers for reinstatement of certain PHMs (e.g., based on VOCs that are more transmissible, cause more severe disease, or have immune escape properties);
- identifying current gaps in knowledge and facilitating research activities to inform current and future advice surrounding PHMs;
- in alignment with scoping exercises and stakeholder consultations, as well as lessons learned activities from the COVID-19 pandemic, evaluating the PHMs component of the COVID-19 pandemic response to incorporate outputs into PHMs planning for future pandemics; and
- developing proactive, seasonal infectious illnesses prevention strategies/messaging for COVID-19, similar to other respiratory illnesses (e.g., influenza, RSV).
Planning variables or signals
Going forward, it will be important to consider uncertainties and challenges around:
- the emergence of VOCs domestically and globally, particularly those associated with increased transmissibility, more severe disease or immune escape;
- decreased protection from vaccines over time;
- community outbreaks in populations at high risk of poor health outcomes;
- pandemic fatigue, as well as challenges related to public adherence and trust; and
- managing risk for segments of the population that remain unvaccinated because they are either not eligible (e.g., medical contraindications) or they choose not to be vaccinated.
Indicators such as COVID-19 epidemiology, health care and public health capacity, as well as risk reduction measures in place for high-risk populations and settings should be considered when determining if/when additional PHMs need to be implemented. If PHMs need to be re-instated, they should be proportionate with the risk in the local community, balanced against the risk of unintended consequences of the intervention, and responsive to the local circumstance (e.g., taking into consideration key indicators and factors such as transmissibility and severity of a VOC.
Appendix 8: Infection prevention and control
While impacting the FPT public health response, the provision of infection prevention and control (IPC) and expert advice has predominantly been aimed at informing healthcare setting and infection prevention and control professionals. Guidance for infection prevention and control will focus on ongoing measures based on emerging IPC science for managing COVID-19 as an ongoing, predictable infectious disease in Canada.
Current status/focus
The current focus of response activities pertaining to IPC include:
- ensuring that previously published COVID-19 Infection Prevention and Control documents continue to provide up-to-date relevant and evidence-informed guidance; and,
- preparing guidance for an ongoing COVID-19 activity in Canada particularly related to routine practices, additional precautions, and other IPC guidance.
Preparations/forward planning
All COVID-19 Infection Prevention and Control guidance documents should be reviewed on an ongoing basis to ensure they reflect the most up to date emerging science in IPC. This includes key infection prevention and control findings in the literature, responding to new and/or changing science.
Planning variables or signals
If additional infection prevention and control information emerges, (e.g., a change in mode of transmission, dominance of VOCs with immune escape characteristics, or additional risk groups), there may be a need to revise or develop additional IPC guidance documents.
Appendix 9: Vaccination
In December 2020, Canada received its first shipments of COVID-19 vaccines and proceeded to administer more than one million doses in the first two months of the national vaccination campaign. Since then, the Government of Canada has been able to offer all people residing in Canada 5 years of age and older a primary vaccine series, as well as booster doses to all those who are eligible.
To support the ongoing COVID-19 vaccination campaign, Canada has secured sufficient vaccine supply to meet current and future needs including possible new vaccine formulations that may be variant specific.
The Government of Canada signed advance purchase agreements to secure access to several COVID-19 vaccine candidates, including Moderna, Pfizer-BioNTech, AstraZeneca, Janssen (Johnson & Johnson), Novavax, Medicago, and Sanofi/GlaxoSmithKline. P/T governments, together with federal and Indigenous partners, developed plans for the efficient, equitable and effective distribution and administration of COVID-19 vaccines across Canada, including prioritizing key populations for early vaccination based on risk of severe outcomes and risk of COVID-19 exposure, particularly in the context of limited vaccine supply.
Much of this work was done in collaboration with the SAC and the Canadian Immunization Committee (CIC), which have both played integral roles in Canada’s COVID-19 pandemic response by fostering FPT collaboration and vaccine rollout coordination. Most P/T immunization plans are informed by guidance from Canada’s National Advisory Committee on Immunization (NACI), an advisory body of experts external to government who provide independent advice to the Public Health Agency of Canada and PTs on the use of authorized vaccines in Canada. NACI continues to develop guidance on the optimal use of COVID-19 vaccines, as new COVID-19 vaccines continue to be authorized and as new real world data and evidence on COVID-19 and COVID-19 vaccines continue to emerge.
In addition to collaborative work with jurisdictions and Indigenous partners to purchase, allocate, distribute and administer vaccines as efficiently, equitably and effectively as possible, work has also been undertaken across Canada to monitor the safety, coverage and effectiveness of COVID-19 vaccines.
Vaccination will continue to be an important tool to prevent severe outcomes from COVID-19 and to prevent healthcare system capacity from being overwhelmed, supporting continued access to health care for both COVID-19 and non-COVID needs.
Current status/focus
As of February 24, 2022 a total of six COVID-19 vaccines are authorized by Health Canada for use in Canada including:
- two mRNA vaccines (e.g. Pfizer-BioNTech Comirnaty, Moderna Spikevax),
- two viral vector vaccines (e.g. AstraZeneca Vaxzevria and Janssen),
- a protein subunit vaccine (e.g. Novavax Nuvaxovid), and
- a virus like-particle-based vaccine (Medicago Covifenz).
Canada continues to be a world leader in COVID-19 vaccination coverage. With its robust vaccine supply Canada is now focusing on providing booster and pediatric doses to all eligible people in Canada, guided by scientific data and advice.
FPT governments, First Nations, Inuit and Métis leadership and public health authorities continue to collaborateFootnote 38 to ensure that vaccination programs and vaccine delivery models are designed and implemented in a manner that is equitable, accessible and sensitive to individual and community needs, including robust, culturally appropriate communication and delivery plans. PHAC’s Vaccine Rollout Task Force has hosted over 50 bilateral and multilateral engagements with PTs, 1 Rehearsal of Concept, and 5 Federal, Provincial, Territorial and Indigenous summits (4 of which had international presenters) to discuss various aspects of vaccine rollout and facilitate the sharing of best practices and lessons learned.
Implementation as documented in the Comprehensive Distribution Plan, and guided by the Vaccine Annex of the CPIP is continuing. Canada’s COVID-19 immunization plan includes enhanced tracking systems for monitoring adverse events following immunization (AEFI), the Vaccine Injury Support Program, vaccine effectiveness, as well as assessment of vaccine uptake/coverage; allocation, storage and handling; and vaccine delivery strategies. Instrumental to the FPT vaccine rollout is VaccineConnect, a digital vaccine management platform, which has been designed to augment existing provincial and territorial public health information technology systems to facilitate end-to-end vaccine and therapeutics management. These enhanced tracking and monitoring systems have been critical for alerting and signaling safety concerns, identifying supply challenges and for informing overall immunization programming.
The National Operations Centre for COVID-19, is the federal logistical coordination entity and focal point for managing vaccine delivery and collaboration with provinces and territories for distribution. The NOC supports partners involved in Canada’s COVID-19 immunization roll out and continues to lead the tracking of vaccine delivery and distribution across Canada.
PHAC has contracted logistics service providers who are supporting importation, storage and distribution for several vaccine candidates. The logistic service providers complement provincial and territorial supply chains, and align with the activities that provinces and territories and Indigenous, remote and isolated communities have undertaken to strengthen supply chains within their jurisdiction. Building upon the collaborative work to date to strengthen cold chains, continued FPT engagement will facilitate advancement of this initiative throughout the supply chain.
A key component to the COVID-19 immunization roll out has been to ensure that health care providers have the training, tools and resources they need to support public health practice for primary series, booster and pediatric vaccination. The federal government continues to collaborate with PTs, Indigenous partners, and other health system stakeholders and partners to facilitate the timely sharing of scientific advice, provide educational webinars, immunization clinic guidance and evidence-based information on vaccination decision supports to healthcare providers.
Efforts to support COVID-19 immunization roll out also include emphasis on promoting vaccine confidence and uptake. Through engagement with key partners, stakeholders and experts the Government of Canada has taken a collaborative approach to better understand public opinion and behaviour. This enhanced understanding informs the development of partnerships, educational tools, vaccination projects, and communication strategies to further educate and build trust in COVID-19 vaccines, while addressing mis- and dis-information about vaccine safety and effectiveness. The Immunization Partnership Fund (IPF) is a key funding tool in the federal toolbox to support public health and non-traditional partners at community, regional and national levels to combat vaccine mis- and dis-information, address access barriers, and support culturally appropriate strategies to increase vaccine confidence and uptake, and to reduce the incidence of vaccine preventable diseases including COVID-19.
Further, the Government of Canada has worked closely with P/ T governments and Indigenous partners to develop a standardized Canadian COVID-19 proof of vaccination credential. This collaboration has ensured Canadian citizens and residents had access to a trusted and secure way to demonstrate their vaccination status internationally and domestically. The Government of Canada also engaged with Indigenous communities and organizations to understand and respond to concerns associated with proof of vaccination credentials, including gaps in reporting Indigenous vaccination data into P/T systems.
The Government of Canada’s COVID-19 Vaccine Task Force, as well as the COVID-19 Joint Biomanufacturing Subcommittee, helped identify areas for strategic investments in vaccine research, development, and domestic bio-manufacturing. This has helped guide ongoing work by the Health Portfolio, in partnership with Innovation, Science and Economic Development Canada, to facilitate longer-term domestic production capacity and support future pandemic preparedness; In addition, a COVID-19 Vaccine Clinical Trial Discussion Forum is convening academic, government, and industry partners to discuss vaccine clinical trial challenges and optimal designs.
The Government of Canada continues to implement the Biomanufacturing and Life Sciences Strategy, which was released in July 2021 and presents a long-term vision for strengthening Canada’s biomanufacturing sector and protecting individuals in Canada against pandemics and other health emergencies in the future. Through strategic investments and partnerships, the Government of Canada is working to grow Canada’s capacity to rapidly develop and produce vaccines, therapeutics and other life saving medicines. This includes an agreement with leading COVID-19 vaccine developer Moderna to build a state-of-the art mRNA vaccine production facility in Canada.
Preparations/forward planning
Through a variety of bilateral and multilateral mechanisms the Government of Canada will continue to collaborate with provinces, territories, municipalities, Indigenous partners and other partners to facilitate the rollout of COVID-19 vaccines. Guidance and tracking systems will continue to be updated as vaccine supply changes. The National Emergency Strategic Stockpile procured sufficient supplies to support FPT vaccine administration.
Timelines for activities that support Canada’s COVID-19 Immunization Plan are:
Short term
Immunization readiness and vaccine rollout:
- Ensure vaccines are deployed to all populations, as the result of detailed demand planning with provinces and territories, to support subsequent doses as recommended, and for all eligible age cohorts.
- Developing a Vaccine Confidence Plan as Canada transitions to managing COVID-19 as an ongoing infectious disease including: continue to integrate vaccine confidence messaging and tactics into communications strategies for campaigns (e.g., COVID-19 boosters and pediatric immunization).
- Continue providing appropriate ancillary supplies to PTs for vaccine administration and explore alternative technologies to optimize use.
- Work with provincial and territorial governments and Indigenous partners to ensure that COVID-19 proof of vaccination credentials continue to be issued in a consistent and trusted manner, and remain available to individuals in Canada for use internationally and domestically as needed.
- Work with partners to (1) harmonize eligibility, accessibility, security, and service support for proof of vaccination credentials across the country; and (2) update the credential in response to evolving needs both internationally and domestically.
Vaccine surveillance:
- Continue to collaborate with PTs to monitor vaccine safety and coverage and make information available to Canadians to support vaccine confidence.
- Monitor vaccine effectiveness to inform policy decisions, including the need for additional booster doses.
- Identification of vaccine strategies and vaccine-related research priorities to address changing epidemiological context and emerging evidence (e.g., evidence on the duration of vaccine protection).
- Build additional functionality of VaccineConnect, the digital vaccine management system to support jurisdiction vaccine program management and pan-Canadian reporting.
Vaccine acquisition:
- Manage existing and future supply arrangements, guided by scientific data and advice, to support PT’s COVID-19 vaccination campaigns; considerations include ensuring appropriate mix of mRNA and non-mRNA options as well as balancing current versus future supply needs in light of new product vaccine technologies and formulations.
- Continue to collaborate with manufacturers to obtain sufficient supportive guidance and training to build the capacity and capability of provinces, territories, First Nations, Inuit and Métis partners and federal department to manage anticipated supply and distribution of vaccines.
- Continue to work with FPT and international partners on the management of doses that are surplus to domestic requirements to support Canada’s commitment to global vaccine equity.
Engagement:
- Continue FPT and Indigenous collaboration to promote vaccines, confidence and uptake, including booster and pediatric doses by reducing barriers to vaccination, including access to convenient community vaccination sites and pop-up/mobile options.
- Continue to foster FPT collaboration on Canada’s COVID-19 pandemic response via the FPT Special Advisory Committee, Canadian Immunization Committee, and bilateral and multilateral engagements.
- In conjunction with Indigenous Services Canada and First Nations Inuit Health Branch, continue to engage with Indigenous partners to support collaboration on vaccination programs and vaccine delivery models that are equitable, accessible, and sensitive to needs and conditions of communities
- Ongoing FPT/I dialogues for sharing challenges and lessons learned, including strategies to bolster vaccine roll-out capacity, target uptake in hard-to-reach populations and communities, and to prepare for rapid roll-out of campaigns for new vaccine formulations for eligible age cohorts and additional booster doses as needed.
- Provide continuing support through the Immunization Partnership Fund regarding efforts by partners at the community, regional and national levels to reach at-risk and underserved populations, reduce access barriers and increase vaccine confidence and uptake through evidence-based and culturally appropriate approaches.
- Continue bilateral and multilateral engagement with international partners to ensure Canada’s proof of vaccination credential is accepted internationally, and to seek mutual verification/interoperability of credentials with other countries where possible and appropriate.
Mid term:
Immunization readiness and vaccine rollout:
- Work on vaccine confidence including public education and communication campaigns, partnership project investments and tailored efforts targeted to the population as a whole and priority subgroup in Canada as vaccine options, eligibility and COVID-19 epidemiology evolves and to catch-up on uptake of routine immunization programs.
- Prepare to address new challenges and the future vaccination needs of individuals in Canada by building on best practices and lessons learned during COVID-19 through the renewal of the National Immunization Strategy
Vaccine surveillance:
- Conduct/support data analysis to inform the need for new vaccine formulations to ensure protection against emerging VOCs, booster doses, and/or seasonal vaccination programs.
- Undertake causality assessments and support research to better understand specific safety signals.
- Explore new data collection methodologies, and partnerships to understand barriers to vaccination.
Vaccine acquisition:
- Manage vaccine supply arrangements, considering the possible recommendation for seasonal booster campaigns, and the need to secure doses past 2023.
- Continue to work with suppliers on availability of new product presentations, including single-dose formats, in order to meet the evolving vaccine administration needs in Canada.
Engagement:
- Build and maintain relationships, support community engagement and equip trusted community leaders (e.g., faith-based leaders, newcomer support organizations, family/youth organizations) with evidence-based information, resources and tools to support informed vaccination choices and address mis- and dis-information.
Longer term:
Immunization readiness and vaccine rollout:
- Explore innovations/strategies to enhance the speed and scale of distribution and uptake of vaccines and other medical counter measures to support planning for efficient and effective response to pandemics and other infectious disease outbreaks.
- Ongoing vaccine confidence, promotion and uptake support programming for COVID-19 vaccines, and to protect against other vaccine preventable diseases.
- Adaptation of the contents of the CPIP Vaccine Annex for the COVID-19 context as necessary.
- Explore options for leveraging VaccineConnect to support pan-Canadian medical counter measure initiatives beyond COVID-19.
Vaccine surveillance:
- Ongoing monitoring of vaccine safety, coverage, and effectiveness in collaboration with partners.
- Evaluate current vaccine surveillance efforts to inform signal detection and the surveillance of population risk or protection from vaccine preventable diseases.
- Capitalise on ongoing vaccine coverage surveillance to ensure necessary evidence is available to assess the level of protection among different population.
Vaccine acquisition:
- Strategic planning for ongoing COVID-19 vaccine supply, including domestic bio-manufacturing capacity, allocation and distribution models and logistics as needed.
Engagement:
- Maintain and enhance robust collaborative infrastructures with provincial, territorial and Indigenous partners to support the evolution of COVID-19 vaccination campaigns and inform the integration of lessons learned into routine immunization programming.
- Work with key partners and stakeholders to explore how greater vaccine acceptance can be fostered across Canada, taking into consideration lessons learned and best practice from COVID-19, to allow for effective response to possible future pandemics and other infectious disease outbreaks.
- Application of lessons learned on COVID-19 vaccine confidence, promotion and uptake to support and maintain partnerships and community outreach efforts for engagement and equipping trusted community leaders with evidence-based information, resources and tools to address mis-information and build long term vaccine confidence and support informed vaccination choices to protect against vaccine preventable diseases.
In addition to COVID-19 vaccine planning, reducing hospitalizations due to seasonal influenza and invasive pneumococcal disease through increased vaccine coverage can preserve both public health resources (e.g., diagnostic/testing, outbreak response) and health care capacity (i.e., outpatient visits and inpatient stays).
Routine immunization programs and influenza vaccines
COVID-19 has required significant public health resources and has inadvertently led to temporary pauses or disruption of routine immunization programs to prioritize pandemic response efforts. As provinces and territories lift public health measures and as travel increases, the risk of vaccine preventable diseases (VPDs) may also increase. Monitoring routine vaccination coverage and identifying and addressing gaps in routine vaccinations will be important in preventing further spread of VPDs and outbreaks, and in ensuring that the pandemic does not leave a long-lasting immunization gap in any Canadian communities.
NACI will gradually resume activities to provide guidance on other VPDs as new vaccine products emerge, and also to consider strategic use of existing products to prevent VPD resurgence and promote health equity. Guidance from PHAC on managing VPD outbreaks (e.g., measles) will need to be updated in order to prepare for a possible resurgence of VPDs in light of immunization gaps that have resulted from the pandemic. CIC will also resume activity related to routine immunization to ensure that any gaps in routine vaccinations as a result of the pandemic are addressed as well as any other issues regarding immunization programs.
Planning variables or signals
The evolving evidence on vaccine effectiveness and levels of vaccine confidence will be monitored to support continued planning for education, outreach, and uptake supports for routine vaccination programs and campaigns, including response to AEFI reports or signals. This requires continued AEFI surveillance, health promotion and education, vaccine confidence monitoring, health care provider supports, project partnerships, behavioural science and risk communication expertise.
Appendix 10: International border and travel health measures
Since the onset of the pandemic, the Public Health Agency of Canada (PHAC) has significantly shifted and expanded its border and travel health programs to focus primarily on mitigating the risk of COVID-19 importation. These measures, together with other FPT responses, help to protect the capacity of provinces and territories to provide health services to Canadians. Prior to COVID-19, it was not envisioned that Canada would implement extensive border closures as a pandemic response measure. Successful implementation of border and travel health measures has required intensive and ongoing multilateral engagement and cooperation with government and non-government stakeholders (e.g., the air travel industry).
Focus for transition phase
Throughout the past two years, several border and travel health measures critical to the COVID-19 response have been developed and implemented. The following measures remain important during the Transition phase, as FPT partners work to reduce COVID-19 incidence and associated serious illness to a locally manageable level and kick starting recovery activities, while maintaining surveillance, risk assessment capacity and readiness for any resurgence:
- leveraging the provisions of the Quarantine Act and introducing 74 Emergency Orders as of January 31, 2022;
- originally prohibiting entry of foreign nationals (unless exempt), followed by a limitation on entry based on vaccination status;
- restricting direct flights from countries of concern via a Notice to Airmen (NOTAM);
- requiring that travellers obtain a negative pre-departure test from a third country when there are issues with the quality of testing in a country of concern;
- testing and quarantine/isolation requirements for incoming travellers to Canada, including a shift from increased testing and quarantine in light of Omicron back to a surveillance testing model;
- increasing the public health presence at the border (i.e., public health officers being assigned to 36 high volume points of entry) as well as enhanced PHAC capacity to conduct virtual health assessments for COVID-19 via access to a 24/7 Central Notification System;
- updated messaging and communication tools for the travelling public, including through travel advisories, web presence, and travellers handouts;
- linkages between federal and P/T guidance and oversight for the management of international and domestic travellers;
- ongoing cooperation and work with provincial and/or local law enforcement-related partners to support compliance verification and enforcement activities, including ticketing travellers not complying with federal quarantine and/or testing requirements; and,
- enhanced partnerships with provincial and territorial health authorities and other key players to support data-sharing, and compliance and enforcement of quarantine.
Planning variables or signals
The emergence of the Omicron variant underscored the need for ongoing surveillance and operational readiness for resurgence. Moving forward, PHAC will continue to maintain a high level of readiness to respond to COVID-19 through a combination of border and travel measures that are intended to:
- monitor the COVID-19 situation, most notably with the aim of quickly detecting VOCs at points of entry (POEs) and limiting their importation;
- consider domestic epidemiological factors, including regionally-specific factors and provincial and territorial public health measures;
- track the progress of COVID-19 vaccine coverage both domestically and internationally and ongoing scientific evidence on vaccine effectiveness;
- monitor the availability and quality of COVID-19 testing both in Canada and abroad;
- update modelling and risk analysis of other countries and international experiences to capture lessons learned;
- maintain operational capacity pre-, at- and post-border to handle anticipated incoming and outbound travel volumes along with additional measures;
- identify scalable border measure options in case of resurgence;
- evaluate border measures including enhancing or easing measures in coordination and alignment with FPT requirements (while factoring in whole of health system capacity);
- consider the public health/health system capacity to manage potential increase in imported cases (testing, provincial and territorial health care capacities, etc.); and,
- monitor volumes into Canada by cohort (e.g., immigration status, purpose of travel, etc.) and arrival mode.
As international and domestic contexts shift, border and travel measures need to be adapted accordingly. PHAC is working towards a sustainable and adaptive border framework that mitigates serious illness and severe outcomes while enabling economic recovery, enhances the surveillance approach that is ready to respond if new threats are detected, and applies lessons learned from Omicron in Canada and abroad. There is a variety of possible approaches that could be explored and implemented in any combination, as the current Omicron-driven wave subsides.
- Global restrictions: Reduce restrictions for travellers from all destinations, provide relevant travel advice to Canadians, and continue surveillance at the borders.
- Country-specific restrictions: Remove prohibition of entry for all foreign nationals, but maintain/impose restrictions for high-risk countries by exception, based on risk of importation as determined by surveillance testing data from Canada’s Border Testing Program.
- Cohort restrictions: Modify exemptions to entry prohibitions and/or border measures based on a sectoral analysis.
- Testing and/or vaccination certification: Continue to ease or impose measures according to travellers’ test results and/or Proof of Vaccination, in a way that is justified by available scientific evidence and is sensitive to legal and ethical issues, including around equity and accessibility.
The objective of this border framework will be to move towards an empowerment and surveillance approach that is ready to respond if new threats are detected. Surveillance will continue to be the primary goal and a readiness “playbook” will be prepared, as the Government of Canada and FPT partners will need to maintain the ability to ramp up measures in case of a resurgence of COVID-19 or the emergence of new VOCs.
Appendix 11: Health care systems infrastructure
A significant resurgence of COVID-19 in any jurisdiction can have a substantial impact on health care service capacity and the ability of health care organizations to provide optimum care to all patients.
Canadian businesses have stepped up to offer their solutions and expertise, or pivoted their manufacturing facilities. Canada is now successfully producing: therapeutics (e.g., Molnupiravir) Made-in-Canada PPE, medical equipment and supplies to address the urgent needs of frontline workers, and the safety of Canadians at large. In addition, Innovation, Science and Economic Development Canada, Health Canada, PHAC and PSPC Canada continue to work closely together to assess and monitor Canada’s domestic manufacturing of medical equipment and supplies.
With respect to therapeutics, the Interim Order Respecting the Prevention and Alleviation of Shortages of Drugs in Relation to COVID-19, made by the federal Minister of Health on October 16, 2020 introduced tools for the Minister to address drug shortages, or the risk of drug shortages, that may be caused or exacerbated, directly or indirectly, by COVID-19.
Current status/focus
The FPT public health response in terms of health care system infrastructure has involved linking with those partners responsible for monitoring, anticipating and planning for surges in capacity within health care systems in order to increase mutual knowledge and situational awareness, and support response activities regarding the delivery of health care to COVID-19 cases in Canada. To support this work:
- PTs have taken steps to support hospital surge capacity and ensure timely access to critical equipment and supplies;
- the Government of Canada continues to work with provinces and territories: to help ensure health care systems are ready for future waves of the virus, to support populations in situations of vulnerability and high-risk Canadians, including those in long-term care, home care, acute care and palliative care, and to support people experiencing challenges related to mental health, substance use, or housing;
- PTs are working to develop, expand and launch virtual care and mental health tools, including through the use of federal funding to support P/T services;
- The federal government is also committed to sustaining the Wellness Together Canada portal, which is a free 24/7 bilingual online resource that all Canadians can access. The portal serves to supplement any online mental health tools provided by PTs.
- through the federal Safe Long-Term Care Fund, governments will work together to protect people living and working in long-term care, including carrying out infection prevention and control readiness assessments, making improvements to ventilation and hiring and training additional staff or topping up wages to support workforce stability;
- the federal government is supporting infection prevention and control measures in long-term care, including funding for Healthcare Excellence Canada (formerly the Canadian Foundation for Healthcare Improvement) to expand its LTC+ initiative and funding to engage with third parties to help identify resources to conduct readiness assessments in long-term care facilities and support training on infection prevention and control;
- the federal government is also supporting PT testing programs in workplace and high risk congregate settings through the procurement and distribution of free rapid tests;
- the Canadian Red Cross and other non-governmental organizations are being supported by the federal government to build and maintain a humanitarian workforce to provide surge capacity in response to COVID-19 outbreaks and other large-scale emergencies;
- modelling has been used to project anticipated demands;
- sharing of hospital-based data (on rates of admission, current capacity and equipment/supplies/resources usage) has been included in surveillance products; and
- the Logistics Advisory Committee (LAC) was convened in February 2020 to provide an FPT forum for collaboration including identification of FPT PPE, equipment and supply needs, informing procurement and facilitating allocation.
Preparations/forward planning
In terms of forward planning, the Government of Canada will continue to:
- collaborate and work with PTs to better understand the rapid tests and PPE needs across the Pan Canadian landscape;
- explore opportunities to consider sustainable domestic production capacity for medical equipment and supplies such as vaccines, therapeutics, rapid tests and PPE;
- monitor for potential COVID-related drug shortages and work with PTs and stakeholders to proactively develop and implement strategies to manage these risks;
- through the Indigenous Services Canada (ISC) Stockpile and PHAC’s National Emergency Strategic Stockpile (NESS), provide medical equipment and supplies to First Nations, Inuit and Métis communities to support the delivery of health care services;
- consult regularly with PTs to identify need for federal COVID-19 surge capacity supports to jurisdictions, including health human resources and mobile hospital units, as well as identify initiatives over the medium-term to help address gaps in Canada’s health human resources, and encourage PTs to bolster their existing health human resources through the use of other sources such as international medical graduates and foreign-credentialed health professionals;
- facilitate sharing of best practices on alternate care facilities, triage and management of delivery of non-COVID-19 health care services review the latest available scientific evidence to inform guidance for health settings and develop tailored approaches for communities with specific health care needs, such as remote, northern and isolated communities as well as Indigenous Peoples in urban settings;
- work with PTs to support safe resumption of in-person primary care and mental health services (where this were suspended/delayed or shifted to virtual care platforms);
- work through the Health Standards Organization and the Canadian Standards Association (CSA) group to set new national standards for long-term care so that older adults get the best support possible, and work with PTs to use the standards to drive lasting change;
- take more action to help people live longer at home;
- work with PTs as well as other partners and stakeholders to develop national mental health and substance use standards. (These standards will help ensure that Canadians receive high-quality mental health and substance use services, no matter where they live or seek to access services); and
- work with PTs to make sure that the entire Canadian population has access to high-quality care, including ensuring access to a family doctor or primary care team, expanding capacity to deliver virtual care, and increasing access to mental health services.
Provincial and territorial governments, along with health care facilities, many of which are already working close to full capacity, continue to do further planning for how they have in some regions (and could in the future) accommodate potentially large influxes of patients, including establishing triage protocols for the allocation of scarce resources such as ICU beds and specialized health human resources. In remote, northern and isolated communities it is also critical to plan for further potential supply-chain and medical evacuation interruptions due to weather.
The level and type of health care system resources needed to manage the Post-COVID Condition/Long-COVID also requires coordinated planning, especially since its full impact remains to be determined. Forward planning must also consider the broad health care system impacts and changes that have occurred as a result of the COVID-19 pandemic in Canada; for example, the unanticipated reduction in emergency room visits for serious conditions, the shift of primary care to virtual care, the unintended but severe health and safety impacts of removing family caregivers from long-term care facilities, increased incidence of opioid overdose, delayed/decreases in routine immunization, and the backlog of elective procedures.
The implications of these impacts and changes include the need to plan for: more and different supportive care for older adults, “catch-up” of delayed medical tests, treatments and procedures and the need to plan for future waves in a way that doesn’t impede health care systems more than is necessary. In addition, understanding gaps that appeared, and lessons to be learned from how they were addressed, in the intersection between PHMs, health care services and other social determinants of health will be important to consider in a holistic way for future planning. For example, how to make sure individuals experiencing homelessness receive adequate supports to be able to follow PHMs (e.g., isolation and quarantine protocols).
Planning variables or signals
In the event health care institutions start to see an increase in the number or change in the characteristics (e.g., demographics, underlying medical conditions) of patients being treated for COVID-19, the Government of Canada will continue to work with PTs to monitor capacity and facilitate timely access to medical equipment and supplies such as PPE, vaccine ancillary supplies, biomedical equipment and intensive care unit (ICU) beds. The federal government continues to be ready to respond to PT requests for assistance and surge support, (e.g., limited health human resource support, facilitation of mobile health services capacity, safe voluntary isolation sites).
Appendix 12: Communications and outreach
Communication of information and advice in a public health emergency is a critical public health intervention that helps to protect public health, save lives, and minimize the overall social and economic impacts. To ensure this, information must be available in plain language and multiple formats and languages so that it is accessible to all people in Canada, including those with low literacy. Using a risk communications approach, the Public Health Agency of Canada, together with other government departments and P/T counterparts and Indigenous partners, have worked hard to provide health care providers, Canadians and key stakeholders with the timely, trusted, accessible, evidence-informed and complete information they require to protect themselves, their families, their communities and businesses. As Canada transitions to a more sustainable, long-term management of COVID-19, ongoing proactive and targeted communications from trusted sources will continue to be important.
Focus for transition phase
The focus remains on communicating clear, concise and timely information, within a constantly evolving public environment, that will cut through mounting COVID-19 fatigue and mis- and dis-information. The goal is to ensure people in Canada have the information they need to make informed decisions to help protect themselves, their families and their communities from COVID-19.
As Canadians emerge from the latest wave, it is an opportune time to recognize all that we have collectively accomplished, take a broad perspective and map out the path forward. While transitioning out of the acute response phase, it is important to remain nimble and ready to respond to new risks in an appropriate and proportionate manner. All levels of government need to communicate to Canadians that progress may not be linear and continue to promote the various tools, including vaccines, therapeutics, robust surveillance and individual public health measures, to avoid resurgences.
Communications, public education and advertising activities will:
- encourage continued use of individual public health measures, including staying home when sick, washing hands, wearing a mask, ventilation and rapid testing;
- promote COVID-19 booster doses and pediatric vaccination, and possible seasonal immunization programs, such as seasonal flu;
- raise awareness of evolving border measures;
- use credible/trusted sources to counter misinformation and address vaccine hesitancy;
- communicate transitions to management of COVID-19 as an ongoing infectious disease in Canada when prudent; and
- communicate with empathy and honesty to recognize the efforts and sacrifices of Canadians have saved lives; that we are now in a stronger position than ever before; and encourage everyone to continue to use the various tools available.
These activities will be supported by FPT strategies, content and implementation plans that include:
- sufficient public opinion research (POR) and behavioural insights (re. behaviours, vaccine, public health measures, back to school) to identify Canadians’ priorities, values and concerns, and capture regional variations;
- public education campaigns (COVID-19 vaccines, PHMs and mental health);
- campaigns to ensure Canadians are aware of COVID-related travel requirements; and,
- testing and contact tracing related communication activities.
Effective communications will be achieved through a coordinated, strategic and scalable approach to outreach and engagement. This includes communications by the Chief Public Health Officer (CPHO), Deputy Chief Public Health Officer (DCPHO), Chief Medical Officers of Health (CCMOHs) across the country and other P/T and local spokespersons, as appropriate; public education campaigns; traditional and digital media outreach, social media, and website updates.
Significant outreach and engagement with a range of health and non-health stakeholders has been an essential part of the national response to COVID-19. This outreach and engagement has evolved throughout the pandemic from a focus on proactively sharing the latest public health developments and resources to identifying stakeholder information needs and perspectives, to collaborating on guidance development and joint communication initiatives, to transitioning towards a more sustainable approach to long term management of COVID-19. A range of stakeholders have been engaged through regular COVID-19 briefings, teleconferences and webinars including the following: CPHO Health Professionals Forum (national health professional organizations), national allied health organizations, local public health medical officers of health, critical infrastructure stakeholders, agriculture and agri-food stakeholders, business groups, travel associations, airlines, and childcare and education stakeholders. A range of community-level leaders have also been engaged including faith-based organizations, organizations representing racialized communities, and engagement with national and community level First Nations, Inuit and Métis organizations.
It has been and continues to be especially important to engage community leaders from Indigenous communities, rural communities, racialized communities, groups representing newcomers to Canada, and faith-based organizations to help deliver critical informationFootnote 39.
Challenges and considerations
Messages in the earliest phase of the pandemic were clear – stay home; physical distance; wash your hands; wear a mask. Now the environment is much more complex.
- As populations and health care capacities differ across jurisdictions, there will be variability in how each province, territory and community assesses risk and responds to the needs of their respective jurisdictions. Messages and their delivery must be clear so as to avoid confusion and assure Canadians that public health officials are aligned in their approach.
- Canadians have gone through multiple waves across the country and there is a real balance that needs to continue to be communicated as we transition away from the crisis phase: keeping COVID-19 vaccinations up to date, being aware of personal and family risks, and maintaining individual public health measures. This messaging can support individuals to make the right choices for themselves and their family and can help mitigate the impact of pandemic fatigue.
- COVID-19 is here for the foreseeable future and there will continue to be new and important roles for public health to play. Messages must be designed to help manage expectations and emphasize a risk-based approach.
- The risk perception (and compliance) of Canadians will vary based on their individual experiences and their unique reality. Canadians need to assess their activity, their risk tolerance, their risk to others and the importance of their own behaviour in reducing risk. Our communications efforts must arm them with the information to do so easily and accurately.
- There is still much uncertainty that impacts how precise and definitive we can be in our messaging, especially with the new VOCs. As science evolves and we learn more, advice to Canadians may change. It will be important to continue to communicate what is known and what is not known.
- There will continue to be an overwhelming amount of information on COVID-19 and some Canadians may find it hard to distinguish misinformation or disinformation from information from Governments and other credible health sources. Communications efforts must address misinformation and provide everyone in Canada with evidence-based information to help them make the decision to keep their COVID-19 vaccinations up to date.
- Canadians expect timely and responsive communication using newer social media platforms (e.g., TikTok, Instagram) and from leaders and influencers that are meaningful and trustworthy within their communities and social media circles.
- The pandemic has revealed and amplified deeply entrenched health, social, and economic inequities that exist in Canada. The interaction of the social determinants of health in shaping negative health outcomes and driving health inequities is more evident than ever before. Communications efforts will need to acknowledge and address the broader health impacts of this pandemic and consequences of the pandemic response.
- Public opinion research has shown that public trust in messages from the medical and scientific community is declining. Collaborative or complementary communications approaches, and consistent messaging across jurisdictions can help to regain public trust.
- Throughout the pandemic response, there has been an increase in the public’s understanding of public health measures, which can be leveraged in the ongoing fight against COVID-19 as well as with other future public health events.
Planning variables or signals
Surges in cases requiring adjustments to or re-instatement of community-based measures or restrictions, along with any changes in science (e.g., new information about COVID-19 that requires a shift in Canada’s public health response or guidance to specific populations), changes to border measures, emergence of VOCs, availability of boosters or pediatric vaccines, will all necessitate updating of the current FPT communication strategy and products.
Appendix 13: Research
The Government of Canada quickly mobilized Canada’s research and scientific communities in response to the spread of the novel coronavirus (COVID-19). Early in the pandemic, research areas focused on medical countermeasures (vaccines, therapeutics, and diagnostics), clinical management research, predictive modelling, as well as social and policy research. Since then, the research focus has expanded to areas such as mental health and substance use during the pandemic, safety in long-term care homes, Indigenous communities’ experiences with COVID-19, and variants of concern. Community engagement is important to ensure culturally appropriate research approaches.
Current status/focus
- The Government of Canada established mechanisms for mobilizing rapid research responses for this type of emergency, which have been activated to accelerate development of medical countermeasures, to support priority research on the transmission and severity of COVID-19, and to understand the potential benefits and potential limitations of medical, social and policy countermeasures (e.g., the COVID Immunity Task Force).
- Within the Canadian Institutes of Health Research (CIHR), the recently created Centre for Research on Pandemic Preparedness and Health Emergencies, will build on Canada’s research strengths and continues to grow its capacity to be a leader in preventing, preparing for, responding to, and recovering from existing and future pandemics and public health emergencies.
- The funding for the Centre for Research on Pandemic Preparedness and Health Emergencies includes funds for studies on Post-COVID Condition/Long-COVID in Canada.
- Health Canada established and continues to apply a number of temporary innovative and flexible measures to help prioritize and expedite the regulatory review of COVID-19 health products without compromising Canada's high standards for safety, efficacy and quality (these measures have been put in place to facilitate safe and timely access to products Canadians and health care workers need).
- A wide array of Clinical Trials activities for therapeutics and vaccines are underway under the Canadian Treatments for COVID-19 (CATCO) trial.
- PHAC has established a pan-Canadian network for wastewater surveillance for SARS-CoV-2 in collaboration with other federal departments, provincial, territorial and municipal governments and academia across Canada that lays the foundation for timely detection and surveillance of COVID-19 across the country.
- Several federal programs available aimed at mobilizing industry, innovation and research continue to respond to COVID-19.
- Networks such as CanCOVID, COVID-END and National Collaborating Centres, have been launched to facilitate research effort and leverage transdisciplinary knowledge synthesis, translation and expertise among Canada's scientific, policy, and health communities.
- Capacity at federal research facilities is being leveraged, and federal granting agencies are strategically aligned to support Canadian research capacity.
- Knowledge on indoor air quality is being mobilized with federal, provincial, territorial and private sector partners.
- The Canadian private sector (R&D, manufacturing) is engaged in contributing to research and development solutions.
- The Government of Canada is also supporting various strategies to bring significant findings arising from these research efforts to decision-makers in a useful and timely way.
Preparations/forward planning
In an earlier version of this Plan, a number of needs had been identified in order to prepare against surges/resurgences based on the reasonable worst-case scenario. In addition to the activities described above, work has begun in earnest in several crucial areas.
- Strengthening our capacity to deliver on relevant COVID-19 modelling work.
- The COVID-19 pandemic has demonstrated the important role and need for greater and ongoing capacity to implement the full range of modelling tools required to support decision-making during a complex public heath crisis. Models help to predict where and when COVID-19 infections may emerge or re-emerge, emergence of new variants of concern, and they can be used to explore the best combinations of approaches to control disease progression and protect the health of Canadians, including vaccination. Expert groups continue their ongoing work on modelling the reproductive number (R t) over the course of the pandemic, and are working on modelling several scenarios for de-escalation strategies, including border reopening and lifting travel restrictions.
- Examining and addressing the need to pursue research and surveillance studies aiming at better understanding mechanisms of infections, transmission and immunity against the SARS-CoV-2 virus.
- FPT governments are currently focusing on the investigation and tracking of the genetic diversity of SARS-CoV-2, across Canada to better respond to its spread, particularly new variants of concern. However, research is needed to examine the full potential of these variants in their transmissibility, virulence and vaccine efficacy, and to monitor their emergence and presence over time. The Government of Canada launched the COVID-19 Immunity Task Force, which engages universities, hospitals and public health officials to use blood test (serologic) methods to track and study the immune status of various Canadian populations, and will be used to support vaccine surveillance, safety and efficacy. The need for research and research coordination with partners to understand transmission dynamics and impact of non-medical measures (e.g., ventilation, portable air cleaners, etc.) is beginning to take shape through early aerosol transmission studies in high-risk settings, such as hospitals, prisons, and long-term care homes. Discussions and work continues with domestic and international partners to develop COVID-19 animal models and medical countermeasures.
- Strengthening our capacity to coordinate, perform, mobilize and utilize rigorous and rapid evidence review.
- More experts within and outside of government are being leveraged to generate and disseminate evidence reviews and answer specific questions to provide the most up-to-date scientific evidence for optimal decision-making.
- Exploring the epidemiological value of new, innovative methods to track community spread, such as testing SARS-CoV-2 from sewage water.
- Testing wastewater is providing early warning ability at the community level (municipality, special settings such as Long-Term Care Facilities, prisons, hospitals and remote communities). With its FPT partners, the federal wastewater surveillance program is further strengthening the network throughout Canada for surveillance of public health outcomes such as COVID-19.
- NML is conducting wastewater based metagenomics sequencing of COVID-19 virus for early identification of VOCs/variants of interest.
- Examining and addressing the need to pursue research and surveillance studies on COVID-19 at the human-animal interface, and in particular to enhance our understanding of the possible impact of new variants, the range of species that can get infected, and how different species may be affected, carry and transmit the virus.
- While there is limited information on the susceptibility of wildlife to SARS-CoV-2, the virus has infected multiple animal species globally, including farmed mink, companion animals (e.g., cats, dogs, ferrets, hamsters), and zoo animals (e.g., tigers, lions, gorillas, cougars, otters, other).
- Transmission from animals-to-humans has been reported from mink, and recently from hamsters. Other instances of animal-to-human transmission have been suspected (e.g., big cat-to-human in a zoo in the US); however, it has been difficult to clearly demonstrate directionality, given the virus is transmitting so widely in people.
- A collaborative team of scientists, and wildlife and public health experts from across Canada has recently reported a unique lineage of SARS-CoV-2 in white-tailed deer that also includes a viral genome from a human case from southwestern Ontario. According to the paper, the human case had contact with deer prior to contracting COVID-19. This is the first report of this new SARS-CoV-2 lineage and possible deer-to-human transmission of the virus.
- There is currently no scientific evidence that animals play a large role in the current spread of COVID-19. However, as the virus continues to evolve and change, the role of animals as a source of new variants may also change.
- Deer and other cervid species (such as elk and moose) are abundant across the provinces and territories in Canada. More research is required to understand how widespread the new lineage is in deer populations, how and if the virus is transmitted between species, and how this virus differs from existing SARS-CoV-2 lineages in terms of transmission and potential to cause disease.
- Strengthening laboratory capacity in the area of genomic innovation and bioinformatics.
- The Government of Canada has begun to secure investments in this area.
- NML is participating in Genome Canada funded consortium – CanCOGen - for genomic studies, both host and virus.
- Mobilizing knowledge from the social sciences.
- There continues to be a need to invest in and mobilize knowledge relating to social sciences such as sociology, anthropology and psychology. Specifically behavioural science and ethnic research can guide future policy and regulatory actions.
Short to mid term:
In the short to mid term, the approach to these preparations continues to be to:
- work collaboratively with National partners, FPT, stakeholders groups, Indigenous partners (including National Indigenous Organizations; Indigenous researchers and scholars; the National Collaborating Centres for Public Health), and the Federal Science Community to support the work of key task groups mandated to support Canada’s COVID-19 response (Immunity Task Force, the Vaccine Task Force, the Therapeutic Task Group) and Indigenous-led culturally grounded research (with appropriate community engagement and cultural safety in approaches);
- work collaboratively with federal science based departments and agencies with specific targeted engagement with the CIHR and the Chief Science Advisor of Canada; and
- continue engagement with the COVID-19 Governance Structure (via the Technical Advisory Committee (TAC), LAC and SAC). Activities include sharing research, data and local experience that will inform further planning in alignment with our stated public health pandemic goal and objectives (e.g., quantifying the negative and positive consequences of the PHM that were uses in the initial response to be better able to address the inequities that have arisen, evidence generation in the effective and appropriate use of home rapid testing).
Planning variables or signals
Similar to the other COVID-19 response components above, there are several factors that could potentially impact preparations for the ongoing COVID-19 response, including: a significant shift in genomic pattern of SARS-CoV2 (leading to examination of possible shift in virulence or infectivity), significant increases in the mortality ratio, data from vaccine and therapeutic clinical trials, data on immunological protection of Canadians, new/rigorous knowledge on the impact of COVID-19 specific high-risk groups, and new/rigorous knowledge of the importance of a non-respiratory mode of transmission.
References
- Footnote 1
-
World Health Organization (WHO), "Pandemic fatigue: reinvigorating the public to prevent COVID-19: policy considerations for Member States in the WHO European Region," 2020. [Online]. Available: https://apps.who.int/iris/handle/10665/335820.
- Footnote 2
-
Alberta Health Services, "COVID-19 Scientific Advisory Group Rapid Evidence Report: Attitudes and Adherence to COVID-19 Guidelines," September 2020. [Online]. Available: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-sag-rapid-evidence-report-attitudes-and-adherence-to-covid-19-guidelines.pdf. [Accessed March 4 2021].
- Footnote 3
-
Benham, J. L., Lang, R., Kovacs Burns, K., MacKean, G., Léveillé, T., McCormack, B., & Marshall, D. A. (2021). Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: A qualitative study to inform public health messaging. PloS one, 16(2), e0246941. https://doi.org/10.1371/journal.pone.0246941
- Footnote 4
-
Seale H, Dyer CEF, Abdi I, Rahman KM, Sun Y, Qureshi MO, et al. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect Dis. 2020;20(1):607. https://doi.org/10.1186/s12879-020-05340-9.
- Footnote 5
-
Escandón K, Rasmussen AL, Bogoch II, Murray EJ, Escandón K, Popescu SV, Kindrachuk J. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infectious Diseases. 2021 July (1):1-47. https://doi.org/10.1186/s12879-021-06357-4
- Footnote 6
-
Public Health Ontario, "Negative Impacts of Community-based Public Health Measures on Children, Adolescents and Families Duriong the COVID-19 Pandemic: Update," 11 January 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/he/2021/01/rapid-review-neg-impacts-children-youth-families.pdf?la=en.
- Footnote 7
-
Chiesa, V., Antony, G., Wismar, M., & Rechel, B. (2021). COVID-19 pandemic: health impact of staying at home, social distancing and 'lockdown' measures-a systematic review of systematic reviews. Journal of public health (Oxford, England), 43(3), e462–e481. https://doi.org/10.1093/pubmed/fdab102
- Footnote 8
-
Fiorillo, A., Sampogna, G., Giallonardo, V., Del Vecchio, V., Luciano, M., Albert, U., Carmassi, C., Carrà, G., Cirulli, F., Dell'Osso, B., Nanni, M. G., Pompili, M., Sani, G., Tortorella, A., & Volpe, U. (2020). Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. European psychiatry: the journal of the Association of European Psychiatrists, 63(1), e87. https://doi.org/10.1192/j.eurpsy.2020.89
- Footnote 9
-
World Health Organization. (2017). Pandemic influenza risk management: a WHO guide to inform and harmonize national and international pandemic preparedness and response. World Health Organization. [Online] Available: https://apps.who.int/iris/handle/10665/259893 License: CC BY-NC-SA 3.0 IGO
- Footnote 10
-
Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2020. From risk to resilience: An equity approach to COVID-19. Public Health Agency of Canada. [Online]. Available: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html
- Footnote 11
-
E. M. Abrams and S. J. Szefler, "COVID-19 and the impact of social determinants of health," The Lancet Respiratory Medicine, vol 8, no. 8, p. 743, August 2020.
- Footnote 12
-
Public Health Ontario, "COVID-19 - What We Know So Far about... Social Determinants of Health," 24 May 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2020/05/what-we-know-social-determinants-health.pdf?la=en
- Footnote 13
-
Public Health Ontario, "Economic Impacts Related to Public Health Measures in Response and Recovery during the COVID-19 Pandemic," 11 March 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/phm/2021/03/eb-covid-19-economic-impacts.pdf?la=en
- Footnote 14
-
R. M. Siegel, P. J. Mallow. The Impact of COVID-19 on Vulnerable Populations and Implications for Children and Health Care Policy. Clin Pediatr (Phila). 2021 Feb;60(2):93-98. doi: 10.1177/0009922820973018. Epub 2020 Nov 26. PMID: 33243000.
- Footnote 15
-
E. M. Abrams and S. J. Szefler, "COVID-19 and the impact of social determinants of health," The Lancet Respiratory Medicine, vol 8, no. 8, p. 743, August 2020.
- Footnote 16
-
Public Health Ontario, "COVID-19 - What We Know So Far about... Social Determinants of Health," 24 May 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2020/05/what-we-know-social-determinants-health.pdf?la=en
- Footnote 17
-
Public Health Ontario, "Negative Impacts of Community-based Public Health Measures on Children, Adolescents and Families Duriong the COVID-19 Pandemic: Update," 11 January 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/he/2021/01/rapid-review-neg-impacts-children-youth-families.pdf?la=en.
- Footnote 18
-
Chiesa, V., Antony, G., Wismar, M., & Rechel, B. (2021). COVID-19 pandemic: health impact of staying at home, social distancing and 'lockdown' measures-a systematic review of systematic reviews. Journal of public health (Oxford, England), 43(3), e462–e481. https://doi.org/10.1093/pubmed/fdab102
- Footnote 19
-
Fiorillo, A., Sampogna, G., Giallonardo, V., Del Vecchio, V., Luciano, M., Albert, U., Carmassi, C., Carrà, G., Cirulli, F., Dell'Osso, B., Nanni, M. G., Pompili, M., Sani, G., Tortorella, A., & Volpe, U. (2020). Effects of the lockdown on the mental health of the general population during the COVID-19 pandemic in Italy: Results from the COMET collaborative network. European psychiatry: the journal of the Association of European Psychiatrists, 63(1), e87. https://doi.org/10.1192/j.eurpsy.2020.89
- Footnote 20
-
Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2020. From risk to resilience: An equity approach to COVID-19. Public Health Agency of Canada. [Online] Available: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html
- Footnote 21
-
E. M. Abrams and S. J. Szefler, "COVID-19 and the impact of social determinants of health," The Lancet Respiratory Medicine, vol 8, no. 8, p. 743, August 2020.
- Footnote 22
-
Public Health Ontario, "COVID-19 - What We Know So Far about... Social Determinants of Health," 24 May 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2020/05/what-we-know-social-determinants-health.pdf?la=en
- Footnote 23
-
Public Health Ontario, "Economic Impacts Related to Public Health Measures in Response and Recovery during the COVID-19 Pandemic," 11 March 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/phm/2021/03/eb-covid-19-economic-impacts.pdf?la=en.
- Footnote 24
-
R. M. Siegel, P. J. Mallow. The Impact of COVID-19 on Vulnerable Populations and Implications for Children and Health Care Policy. Clin Pediatr (Phila). 2021 Feb;60(2):93-98. doi: 10.1177/0009922820973018. Epub 2020 Nov 26. PMID: 33243000.
- Footnote 25
-
Public Health Ontario. (Nov 2021) Negative Impacts of Community-based Public Health Measures on Children, Adolescents and Families During the COVID-19 Pandemic: Update. https://www.publichealthontario.ca/-/media/documents/ncov/he/2021/01/rapid-review-neg-impacts-children-youth-families.pdf?la=en
- Footnote 26
-
World Health Organization. (2017). Pandemic influenza risk management: a WHO guide to inform and harmonize national and international pandemic preparedness and response. World Health Organization. [Online] Available: https://apps.who.int/iris/handle/10665/259893 License: CC BY-NC-SA 3.0 IGO
- Footnote 27
-
World Health Organization (WHO), "Pandemic fatigue: reinvigorating the public to prevent COVID-19: policy considerations for Member States in the WHO European Region," 2020. [Online]. Available: https://apps.who.int/iris/handle/10665/335820. [Accessed March 4 2021].
- Footnote 28
-
Escandón K, Rasmussen AL, Bogoch II, Murray EJ, Escandón K, Popescu SV, Kindrachuk J. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infectious Diseases. 2021 July (1):1-47. https://doi.org/10.1186/s12879-021-06357-4
- Footnote 29
-
Scientific Advisory Group for Emergencies (SAGE) Academics: Viral evolution scenarios, 10 February 2022 [Online] Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1054323/S1513_Viral_Evolution_Scenarios.pdf
- Footnote 30
-
Bhattacharyya RP, Hanage WP. Challenges in inferring intrinsic severity of SARS-CoV-2 Omicron
variant from early population-level impact. HCPDS Working Paper Volume 21, Number 10. December 15, 2021. [Online] Available: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2623/2021/12/21_Hanage_Bhattacharyya_Challenges-in-assessing-Omicron-severity_HCPDS-Working-Paper-Volume-21_No-10-1.pdf - Footnote 31
-
Emerg Microbes Infect. 2020; 9(1): 2222–2235.
Published online 2020 Oct 14. doi: 10.1080/22221751.2020.1827984
PMCID: PMC7594747
PMID: 32967592
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7594747/ - Footnote 32
-
Emerg Microbes Infect. 2020; 9(1): 2222–2235.
Published online 2020 Oct 14. doi: 10.1080/22221751.2020.1827984
PMCID: PMC7594747
PMID: 32967592
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7594747/ - Footnote 33
-
“The presence of genetic polymorphisms and pathogenic auto-autoantibodies in severe COVID-19 also suggests a significant contribution of immune dysregulation to poor outcomes.”
“Hyperinflammation is a key component of severe COVID-19,”
https://pubmed.ncbi.nlm.nih.gov/34264880/ - Footnote 34
-
Escandón K, Rasmussen AL, Bogoch II, Murray EJ, Escandón K, Popescu SV, Kindrachuk J. COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection. BMC Infectious Diseases. 2021 July (1):1-47. https://doi.org/10.1186/s12879-021-06357-4
- Footnote 35
-
Public Health Ontario, "COVID-19 - What We Know So Far about... Social Determinants of Health," 24 May 2021. [Online]. Available: https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/2020/05/what-we-know-social-determinants-health.pdf?la=en
- Footnote 36
-
R. M. Siegel, P. J. Mallow. The Impact of COVID-19 on Vulnerable Populations and Implications for Children and Health Care Policy. Clin Pediatr (Phila). 2021 Feb;60(2):93-98. doi: 10.1177/0009922820973018. Epub 2020 Nov 26. PMID: 33243000.
- Footnote 37
-
B.C. Centre for Disease Control. Societal Consequences of COVID-19. [Online] Available: http://www.bccdc.ca/health-professionals/data-reports/societal-consequences-covid-19
- Footnote 38
-
Canada’s COVID-19 Immunization Plan: Saving Lives and Livelihoods. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/canadas-reponse/canadas-covid-19-immunization-plan.html
- Footnote 39
-
Krishnan, L., Ogunwole, S. M., & Cooper, L. A. (2020). Historical Insights on Coronavirus Disease 2019 (COVID-19), the 1918 Influenza Pandemic, and Racial Disparities: Illuminating a Path Forward. Annals of Internal Medicine. https:// doi:10.7326/M20-2223