Public health level recommendations on the use of pneumococcal vaccines in adults, including the use of 15-valent and 20-valent conjugate vaccines
Download in PDF format
(1.3 MB, 88 pages)
Organization: Public Health Agency of Canada
Date published: 2023-02-24
Cat.: HP5-153/1-2023E-PDF
ISBN: 978-0-660-47229-4
Pub.: 220712
An Advisory Committee Statement (ACS)
National Advisory Committee on Immunization (NACI)
Table of Contents
- Summary of information contained in this NACI Statement
- I. Introduction
- II. Methods
- III. Epidemiology
- IV. Vaccine
- IV.1 Preparations authorized for use in Canada
- IV.2 Efficacy and effectiveness
- IV.3 Immunogenicity
- IV.4 Persistence of Immune Response
- IV.5 Vaccine Administration and Schedule
- IV.6 Serological Testing
- IV.7 Storage Requirements
- IV.8 Concurrent Administration with Other Vaccines
- IV.9 Vaccine Safety
- IV.10 Contraindications and Precautions
- V. Vaccination of Specific Populations
- VI. Ethics, Equity, Feasibility and Acceptability Considerations
- VII. Economics
- VIII. Recommendations
- IX. Research priorities
- X. Surveillance issues
- XI. Characteristics of included studies
- List of Abbreviations
- Acknowledgments
- Appendix A: Tables
- References
Preamble
The National Advisory Committee on Immunization (NACI) is an External Advisory Body that provides the Public Health Agency of Canada (PHAC) with independent, ongoing, and timely medical, scientific, and public health advice in response to questions from PHAC relating to immunization.
In addition to burden of disease and vaccine characteristics, PHAC has expanded the mandate of NACI to include the systematic consideration of programmatic factors in developing evidence-based recommendations to facilitate timely decision-making for publicly funded vaccine programs at provincial and territorial levels.
The additional factors to be systematically considered by NACI include: economics, ethics, equity, feasibility, and acceptability. Not all NACI Statements will require in-depth analyses of all programmatic factors. While systematic consideration of programmatic factors will be conducted using evidence-informed tools to identify distinct issues that could impact decision-making for recommendation development, only distinct issues identified as being specific to the vaccine or vaccine-preventable disease will be included.
This statement contains NACI’s independent advice and recommendations, which are based upon the best current available scientific knowledge and is disseminating this document for information purposes. People administering the vaccine should also be aware of the contents of the relevant product monograph(s). Recommendations for use and other information set out herein may differ from that set out in the product monograph(s) of the Canadian manufacturer(s) of the vaccine(s). Manufacturer(s) have sought approval of the vaccine(s) and provided evidence as to its safety and efficacy only when it is used in accordance with the product monographs. NACI members and liaison members conduct themselves within the context of PHAC’s Policy on Conflict of Interest, including yearly declaration of potential conflict of interest.
Summary of information contained in this NACI Statement
The following highlights key information for immunization providers. Please refer to the remainder of the Statement for details.
1. What
Pneumococcal disease in adults includes invasive pneumococcal disease (IPD), an acute and serious communicable disease with manifestations such as meningitis, bacteremia and bacteremic pneumonia and empyema, as well as non-invasive pneumococcal disease such as community acquired pneumonia and acute otitis media in children. It is caused by the Streptococcus pneumoniae bacterium. Of the more than 100 serotypes of this bacterium, a small number cause the majority of disease. Bacteremic pneumococcal pneumonia is the most common presentation of IPD among adults.
Based on immunogenicity data relative to previously authorized pneumococcal conjugate vaccines (PNEU-C) and pneumococcal polysaccharide vaccines (PNEU-P), Health Canada has recently authorized two new PNEU-C vaccines:
- PNEU-C-15 (15-valent) is authorised for infants, children, and adolescents from 6 weeks through 17 years of age and adults 18 years of age and older with an indication for prevention of IPD caused by 15 serotypes of S. pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F, and 33F).
- PNEU-C-20 (20-valent) is authorized for adults 18 years of age and older with an indication for prevention of pneumonia and IPD caused by 20 serotypes of S. pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F).
No efficacy data are currently available for either PNEU-C-15 or PNEU-C-20.
2. Who
IPD is most common in the very young, the elderly, and groups with medical conditions and/or other risk factors that place them at high risk of IPD (see Table 1).
NACI recommends the use of PNEU-C-20, or PNEU-C-15 followed by pneumococcal polysaccharide vaccine, 23-valent pneumococcal polysaccharide vaccine (PNEU-P-23), in adults at a higher risk of invasive pneumococcal disease.
- All adults 65 years of age and older should receive a single dose of PNEU-C-20.
- Adults who are 50 to 64 years of age and living with underlying medical conditions and/or other risk factors that place them at high risk of IPD should receive a single dose of PNEU-C-20.
- Adults who are 18 years of age and older living with immunocompromising conditions (IC) should also receive a single dose of PNEU-C-20.
- PNEU-C-15 followed by PNEU-P-23 may be offered as an alternative if PNEU-C-20 is not available.
Additional details including immunization of adults who received a hematopoietic stem cell transplant, as well as intervals between previous pneumococcal vaccines and PNEU-C-15/PNEU-C-20 are discussed in Section VII.
| Non-immunocompromising conditions | Immunocompromising conditions Table 1 Footnote a | Other risk factors |
|---|---|---|
|
|
Individuals
|
|
||
3. How
PNEU-C-15 and PNEU-C-20 are supplied in a single-dose, prefilled syringe. Both PNEU-C-15 and PNEU-C-20 are to be administered intramuscularly. A standard schedule for immunization is one 0.5ml dose. Contraindications to administration of either PNEU-C-15 or PNEU-C-20 include hypersensitivity (e.g., anaphylaxis) to the vaccine or any of its components. Pneumococcal vaccines may be administered concurrently with other vaccines, except for a different formulation of pneumococcal vaccine (e.g., concurrent use of conjugate and polysaccharide).
4. Why
Pneumococcal infection can cause severe infections and can lead to significant mortality and morbidity with lifelong complications. The most effective way to prevent these infections is through immunization.
I. Introduction
I.1 Guidance objective
The need for this National Advisory Committee on Immunization (NACI) Statement on the use of pneumococcal vaccines was triggered by the approvals of two additional pneumococcal conjugate vaccines for adults 18 years of age and older, a 15-valent vaccine, PNEU-C-15 (VaxneuvanceTM) on November 16, 2021, and a 20-valent vaccine, PNEU-C-20 (Prevnar 20TM) on May 9, 2022. The primary objective of this statement is to review the evidence on the efficacy, effectiveness, immunogenicity, safety, and cost-effectiveness of PNEU-C-15 and PNEU-C-20 vaccines and provide recommendations for their use in consideration of the disease burden in Canada among adults for whom pneumococcal vaccination is currently recommended:
- immunocompetent adults aged 65 and older
- immunocompetent adults at higher risk of pneumococcal disease (PD) (Table 1)
- immunocompetent adults residing in long term care facilities (LTCF)
- immunocompromised adults, including hematopoietic stem cell transplant recipients
I.2 Background on pneumococcal vaccines, immunization programs and recommendations for adults in Canada
For prevention of IPD in adults, two vaccines are currently available in routine, publicly funded programs: PNEU-P-23 and PNEU-C-13. Conjugate vaccines induce formation of long-term memory cells, provide longer duration of protection, and provide ability for boosting by involving T cells in the immune response to the vaccine, in a way that polysaccharide vaccines do not.
PNEU-P-23 was previously recommended by NACI for the routine immunization against IPD of all adults 65 years of age and older. PNEU-P-23 was also recommended for adults 18 to 64 years old who are residents of LTCF, smokers or persons with an alcohol use disorder, and persons experiencing homelessness as well for those living with both immunocompromising and non-immunocompromising underlying medical conditions that put them at higher risk of IPD. A complete list of underlying medical conditions that increase the risk of IPD along with dose and schedule is available in the Pneumococcal Vaccine Chapter of the Canadian Immunization Guide.
PNEU-C-13 in series with PNEU-P-23 was recommended by NACI in 2013 Footnote 1 for adults 18 years of age and older with immunocompromising conditions resulting in high risk of IPD. For a complete list of immunosuppressing conditions that increase the risk of IPD, please refer to Table 1 in the Pneumococcal Vaccine Chapter of the Canadian Immunization Guide.
PNEU-C-13 was also recommended by NACI in 2016 Footnote 2 and 2018 Footnote 3 on an individual basis for immunocompetent adults aged 65 years and older who wish to protect themselves against the 13 serotypes included in the vaccine for prevention of community-acquired pneumonia (CAP) and IPD. PNEU-C-13 was not recommended for publicly funded routine immunization programs due to cost-effectiveness.
II. Methods
In brief, the stages in the preparation of a NACI advisory committee statement are:
- Knowledge synthesis: retrieval and summary of individual studies, assessment of the risk of bias (RoB) of included studies (summarized in the Summary of evidence tables in Appendix A).
- Summary of evidence: benefits (immunogenicity) and potential harms (safety), considering the certainty of the synthesized evidence and, where applicable, the magnitude of effects observed across the studies.
- Use of the evidence to inform recommendations.
NACI also uses a published, peer-reviewed framework and evidence-informed tools to ensure that issues related to ethics, equity, feasibility, and acceptability (EEFA) are systematically assessed and integrated into its guidance. NACI evaluated the following ethical considerations when making its recommendations: promoting well-being and minimizing risk of harm, maintaining trust, respect for persons and fostering autonomy, and promoting justice and equity.
Further information on NACI’s process and procedures is available elsewhere.
For this statement, NACI reviewed evidence pertaining to the burden of IPD in the target population(s), the safety, immunogenicity, efficacy, and effectiveness of the vaccine(s), vaccine schedules, and other aspects of the overall adult pneumococcal vaccine immunization strategy. The knowledge synthesis was performed by NACI Secretariat and reviewed by the Pneumococcal Working Group. Following critical appraisal of individual studies, summary tables with ratings of the certainty of the evidence using GRADE methodology were prepared Footnote 4 Footnote 5 Footnote 6. An assessment using the Evidence to Decision (EtD) framework was prepared for each question, and proposed recommendations for vaccine use were developed Footnote 7. NACI reviewed the available evidence on May 19, 2022, July 4, 2022, and Sept 12, 2022. The description of relevant considerations, rationale for specific decisions, and knowledge gaps are described.
II.1 Burden of IPD
IPD has been nationally notifiable in Canada to the Canadian Notifiable Disease Surveillance System (CNDSS) since 2000, with all provincial and territorial jurisdictions reporting cases meeting the national case definition. Cases not captured by CNDSS may include those that do not get medical attention, those where clinical measures were applied with no specimen being taken. Information such as serotype, antimicrobial susceptibility, vaccine coverage as well as other enhanced epidemiological patient information are not reported through the CNDSS.
The national surveillance line list data used to assess the burden of IPD among different age groups were available from the CNDSS for six provinces (BC, AB, SK, ON, QC, and PEI) and from the International Circumpolar Surveillance (ICS) program for the three territories (YK, NU, and NT). Some provinces (MB, NS, NL, NB) were not included in the national surveillance line list as they provided aggregate data with broad age group intervals which could not be broken down to compare the IPD burden in different age groups among older adults in Canada. All cases were presumed to meet the national case definition of IPD. More information about the CNDSS data is provided on the Notifiable Diseases Online website.
Northern regions of Canada captured in the ICS system include Nunavut, Northwest Territories, Yukon, Northern Labrador, and Northern Quebec. The incidence of IPD in these regions was compared to IPD incidence from all other PTs using aggregate CNDSS data.
The National Microbiology Laboratory (NML) collaborates with provincial and territorial public health laboratories to conduct passive, laboratory-based surveillance of IPD in Canada Footnote 8. All IPD isolates from the provincial/territorial public health laboratories are serotyped by the NML, although specimen collection may be limited by variable regional standards, the preliminary nature of some data and the availability of bacterial isolates for testing. Serotype data may also be biased toward over representing more virulent serotypes for which medical treatment is sought and clinical specimens taken. Despite these limitations, the passive national surveillance program from 2015 – 2019, including additional data submitted by the provincial reference laboratories of Alberta and Quebec, provided timely reporting of serotype distributions, and accounted for 80 to 98% of all IPD cases reported to CNDSS. In 2020 Footnote 9, a total of 2,067 isolates were reported to the NML, representing 94.3% of the 2,193 reported by all PTs to the CNDSS (preliminary 2020 data).
For vaccine serotype groupings, serotype 6C was included with PNEU-C-13 serotypes due to cross protection with 6A Footnote 10. Serotypes 15B and 15C were grouped together as 15B/C because of reported reversible switching between them in vivo during infection, making it difficult to precisely differentiate between the two types Footnote 11 Footnote 12.
II.2 Literature Review of PNEU-C-15 and PNEU-C-20 studies
The policy question addressed in this statement is: What is the efficacy, effectiveness, and safety of PNEU-C-15 and PNEU-C-20, administered in series with or without PNEU-P-23, when used with the objective to reduce the risk of IPD in adults.
Population: Adults 50 years of age or older without IPD risk factors; adults 18 years or older with IPD risk factors (Table 1).
Intervention: PNEU-C-15 or PNEU-C-20, alone and in series with PNEU-P-23 (depending on the population group of interest).
Comparator: Currently recommended age and risk factor-appropriate pneumococcal vaccine schedule.
Outcomes: Death due to vaccine preventable serotype S. pneumoniae, IPD due to vaccine preventable pneumococcal serotype, IPD due to any pneumococcal serotype (vaccine preventable and not vaccine preventable), pneumococcal community-acquired pneumonia (pCAP) due to a vaccine preventable serotype, serious adverse events (SAEs), severe systemic adverse events (AEs), and mild/moderate systemic AEs following vaccination. Outcomes were accompanied by definitions and are summarized in the appendix (see Appendix A, Table 6).
In the absence of disease endpoint and mortality data, immunogenicity (opsonophagocytic [OPA] geometric mean titer [GMT] ratios and percentage of seroresponders defined as greater or equal to a 4-fold increase in OPA GMT ratio from before vaccination to after vaccination) was evaluated.
Safety and immunogenicity data for PNEU-C-15 and PNEU-C-20 in adults from key clinical trials, published studies, and supplementary data obtained from manufacturers were reviewed. Data were extracted from eligible studies related to the study design, population, intervention, comparator, and outcomes of interest. The RoB (Appendix A, Table 8) for each study was assessed using the Cochrane Risk of Bias Tool Footnote 13. The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework (Appendix A, Table 5) was used to assess the certainty in evidence.
Meta-analytic techniques were used to synthesize adverse event data; statistical heterogeneity was considered using a combination of factors (direction of estimates, overlapping confidence intervals, and the Cochran Q [p<0.10] and I-squared statistics). For I-squared statistics, a rough guide of low (0-25%), moderate (25-50%), substantial (50-75%), and considerable (75-100%) was used. For binary outcomes and where event rates were low (using 1% as a rough guide), the Peto Odds Ratio was used; otherwise, the Risk Ratio was used. Where possible to do so, relative effect measures were used to calculate risk differences, aligning with the GRADE approach. For immunogenicity, narrative syntheses were used, and heterogeneity was determined according to the direction of effect, using the magnitude of the estimates. The focus for GMT ratios was the study investigators’ demonstration of non-inferiority for shared serotypes between vaccines. For the percentage of seroresponders, point estimates were used to gauge the direction of effect based on those magnitudes. It is important to note, however, that no immunologic correlates of protection have been established for PD.
For the GRADE certainty of evidence assessments (Appendix A, Table 5), control group data from studies were used to estimate baseline risk. The use of surrogate measures was the main consideration for indirectness. The review information sizes of 400 people with events for binary data, at least 4,000 people analyzed for small event rates, and 800 people for continuous data were used to inform imprecision when confidence intervals were not importantly wide. Planned subgroup analyses was not undertaken for the age-based recommendation owing to the nature of the data and insufficient number of studies. Sensitivity analyses were undertaken to restrict analyses to studies at a low RoB, where applicable, to see if the results changed appreciably. Too few studies were located to perform a test for small study effects.
Modifications to scope and process during conduct of the review: (a) an evaluation for the 75 years and older age group was added for the age-based recommendation; (b) expansion of eligibility to include additional vaccines administered concurrently with pneumococcal vaccines; and (c) full verification of data extraction, RoB assessments, and GRADE assessments were reduced to partial verification or single person review to facilitate a rapid review of the evidence.
II.3 Literature review of PNEU-C-15 and PNEU-C-20 cost-effectiveness
A systematic review of the cost-effectiveness of PNEU-C-15 and PNEU-C-20 vaccines for preventing IPD was conducted. The search included economic evaluations conducted in adults aged 18 years or older, comparing currently used vaccines to prevent IPD to PNEU-C-15 or PNEU-C-20. The components of the research question are summarized as:
- Population: Adults aged 18 years or older
- Intervention: PNEU-C-15 or PNEU-C-20 (alone or in series with other pneumococcal vaccines)
- Comparator: Current pneumococcal vaccines (PNEU-C-7, PNEU-C-10, PNEU-C-13, PNEU-P-23)
- Outcomes: Measures of cost-effectiveness (incremental cost per quality-adjusted life year [QALY], incremental cost per disability-adjusted life year [DALY], and cost per life year, etc.)
Additional details of the economic literature review are provided in a supplementary economic evidence appendix.
II.4 NACI Cost-utility analysis and multi-model comparison
A model-based cost-utility analysis was conducted from health system and societal perspectives. A Markov cohort model was developed to compare the benefits (in QALYs) and costs (in 2022 Canadian dollars) associated with using PNEU-C-15 or PNEU-C-20, either alone or in series with PNEU-P-23, compared to PNEU-P-23 alone. Vaccination was evaluated at ages 50, 65, or 75. The Northern Canadian Territories were assessed separately from the rest of Canada to account for higher PD incidence in the north. The primary outcome was the incremental cost-effectiveness ratio (ICER). The analysis used a lifetime time horizon and 1.5% discount rate. Scenario and sensitivity analyses were conducted to examine the impact of uncertainties in model parameters and assumptions.
To evaluate the robustness of the cost-utility model, a multi-model comparison was conducted using two additional cost-utility models developed by the manufacturers of PNEU-C-15 and PNEU-C-20 with different structures and assumptions. Wherever possible, all models were modified to use the same input parameters. ICERs for a single base case were compared across models.
Additional details of the cost-utility analysis and multi-model comparison are provided in a supplementary economic evidence appendix.
III. Epidemiology
III.1 IPD burden in Canada
Based on the data from CNDSS, the incidence rate of IPD in children under 5 years of age decreased from 41.8 cases to 15.7 cases per 100,000 population between 2003 and 2006. Following a few years of increasing incidence, IPD incidence rates in children under 5 years have remained relatively steady at around 12 cases per 100,000 population since 2012 (Figure 1). Children aged 5 to17 years consistently had the lowest IPD incidence rate, remaining below 5 cases per 100,000 population during the 2001-2019 study period. Canadians aged 18 to 49, 50 to 64 and 65 years and older showed similar trends with increased IPD incidence from 2001 to 2004, probably due to improvements in diagnosis and reporting, followed by relatively stable incidence rates in the subsequent 15 years. The incidence rate in adults 65 year of age and older was reported to be consistently higher by approximately 10 to 15 cases per 100,000 population than in adults aged 50 to 64 years old (e.g., in 2019, it was reported at 25 cases and 14 cases per 100,000 population, respectively). Adults aged 18 to 49 years consistently had the second lowest IPD incidence rates compared to other age groups, maintaining an incidence around 5 cases per 100,000 population from 2001-2019.
Figure 1: Annual incidence rate of IPD by age group reported to Canadian Notifiable Disease Surveillance System, 2001-2019
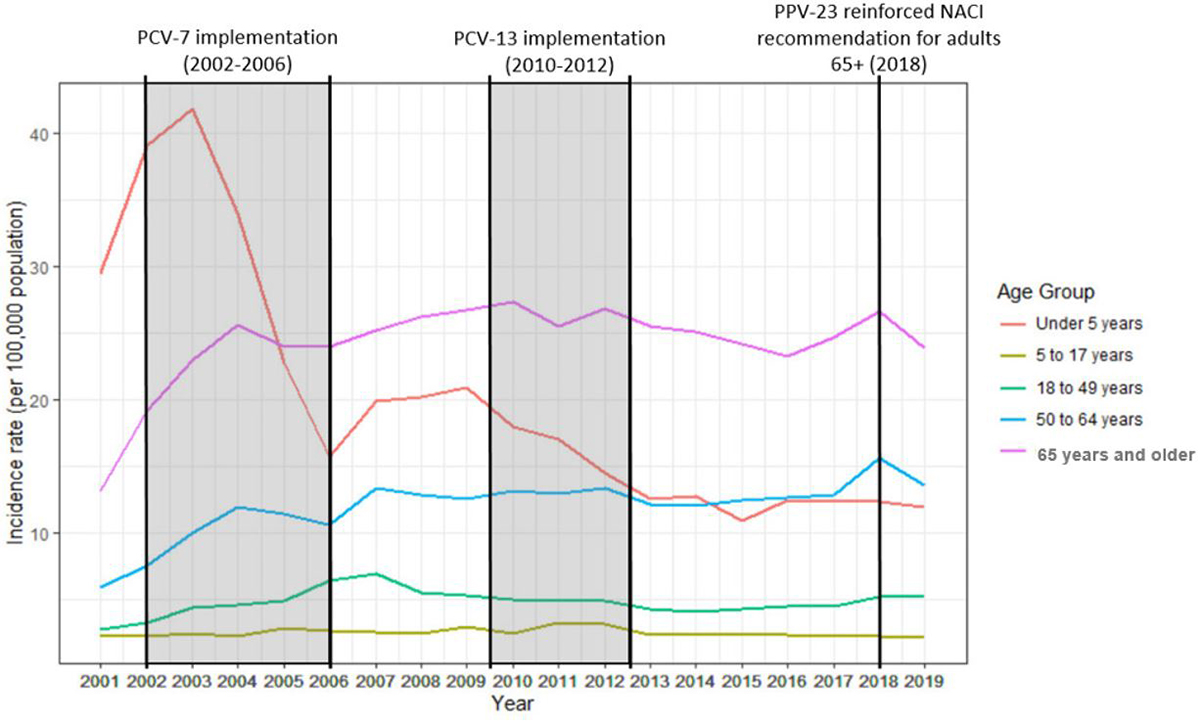
Text Description
Figure 1 shows the incidence rate of invasive pneumococcal disease (IPD) (vertical axis) per 100,000 population with respect to year in one-year increments (horizontal axis) from 2001 to 2019 in Canada, grouped by age category. The shaded boxes provide additional context concerning Canada's PNEU-C-7 implementation for the pediatric population (2002-2006), PNEU-C-13 implementation for the pediatric population (2010-2012). PNEU-P-23 recommendation for all Canadians 65 years and older (2018) is shown with a line. The incidence rates were calculated using data from the ICS program for Canada's three territories, and data from CNDSS for six provinces that had line list data available (AB, BC, ON, QC, SK, and PEI).
| Year | Age group | Incidence rate (per 100,000 population) |
|---|---|---|
| 2001 | Under 5 years | 29.5 |
| 5 to 17 years | 2.2 | |
| 18 to 49 years | 2.7 | |
| 50 to 64 years | 5.9 | |
| 65 years and older | 13.2 | |
| 2002 | Under 5 years | 39.1 |
| 5 to 17 years | 2.2 | |
| 18 to 49 years | 3.2 | |
| 50 to 64 years | 7.5 | |
| 65 years and older | 19.2 | |
| 2003 | Under 5 years | 41.8 |
| 5 to 17 years | 2.4 | |
| 18 to 49 years | 4.4 | |
| 50 to 64 years | 10.0 | |
| 65 years and older | 22.9 | |
| 2004 | Under 5 years | 34.0 |
| 5 to 17 years | 2.2 | |
| 18 to 49 years | 4.6 | |
| 50 to 64 years | 11.9 | |
| 65 years and older | 25.5 | |
| 2005 | Under 5 years | 22.7 |
| 5 to 17 years | 2.9 | |
| 18 to 49 years | 4.9 | |
| 50 to 64 years | 11.4 | |
| 65 years and older | 23.9 | |
| 2006 | Under 5 years | 15.7 |
| 5 to 17 years | 2.6 | |
| 18 to 49 years | 6.4 | |
| 50 to 64 years | 10.5 | |
| 65 years and older | 24.0 | |
| 2007 | Under 5 years | 19.8 |
| 5 to 17 years | 2.5 | |
| 18 to 49 years | 6.9 | |
| 50 to 64 years | 13.3 | |
| 65 years and older | 25.1 | |
| 2008 | Under 5 years | 20.2 |
| 5 to 17 years | 2.4 | |
| 18 to 49 years | 5.5 | |
| 50 to 64 years | 12.8 | |
| 65 years and older | 26.2 | |
| 2009 | Under 5 years | 20.9 |
| 5 to 17 years | 2.9 | |
| 18 to 49 years | 5.3 | |
| 50 to 64 years | 12.5 | |
| 65 years and older | 26.7 | |
| 2010 | Under 5 years | 17.9 |
| 5 to 17 years | 2.5 | |
| 18 to 49 years | 4.9 | |
| 50 to 64 years | 13.1 | |
| 65 years and older | 27.3 | |
| 2011 | Under 5 years | 17.0 |
| 5 to 17 years | 3.2 | |
| 18 to 49 years | 4.8 | |
| 50 to 64 years | 12.9 | |
| 65 years and older | 25.5 | |
| 2012 | Under 5 years | 14.4 |
| 5 to 17 years | 3.1 | |
| 18 to 49 years | 4.9 | |
| 50 to 64 years | 13.4 | |
| 65 years and older | 26.8 | |
| 2013 | Under 5 years | 12.5 |
| 5 to 17 years | 2.3 | |
| 18 to 49 years | 4.3 | |
| 50 to 64 years | 12.1 | |
| 65 years and older | 25.4 | |
| 2014 | Under 5 years | 12.7 |
| 5 to 17 years | 2.3 | |
| 18 to 49 years | 4.1 | |
| 50 to 64 years | 12.0 | |
| 65 years and older | 25.1 | |
| 2015 | Under 5 years | 10.9 |
| 5 to 17 years | 2.4 | |
| 18 to 49 years | 4.2 | |
| 50 to 64 years | 12.4 | |
| 65 years and older | 24.2 | |
| 2016 | Under 5 years | 12.4 |
| 5 to 17 years | 2.3 | |
| 18 to 49 years | 4.5 | |
| 50 to 64 years | 12.6 | |
| 65 years and older | 23.3 | |
| 2017 | Under 5 years | 12.3 |
| 5 to 17 years | 2.2 | |
| 18 to 49 years | 4.4 | |
| 50 to 64 years | 12.8 | |
| 65 years and older | 24.7 | |
| 2018 | Under 5 years | 12.3 |
| 5 to 17 years | 2.2 | |
| 18 to 49 years | 5.2 | |
| 50 to 64 years | 15.6 | |
| 65 years and older | 26.6 | |
| 2019 | Under 5 years | 11.9 |
| 5 to 17 years | 2.1 | |
| 18 to 49 years | 5.2 | |
| 50 to 64 years | 13.6 | |
| 65 years and older | 23.8 |
IPD incidence is directly proportional to age in persons 50 years of age and older (Figure 2). From 2011-2019, IPD incidence rates were highest in the oldest age group (85 years and older). In the other age groups, the incidence rates fluctuated slightly but remained relatively steady from 2011-2019. In Canadians aged 85 years and over, however, the incidence decreased from 50 to 40 cases per 100,000 population between 2011 and 2016. After 2016, incidence rates fluctuated ranging from 39 to 46 cases per 100,000 population, with a mean of 42 cases per 100,000 population. Incidence rates in the other age groups were approximately: 12 to 13 cases per 100,000 population in the 50 to 64 year-old age group; 19-20 cases per 100,000 population in the 65 to 74 year-old age group; and 26-28 cases per 100,000 population in the 75-84 year-old age group.
Figure 2. Annual incidence rate of IPD in Canadian adults 50 years of age and older, reported to Canadian Notifiable Disease Surveillance System, 2001-2019
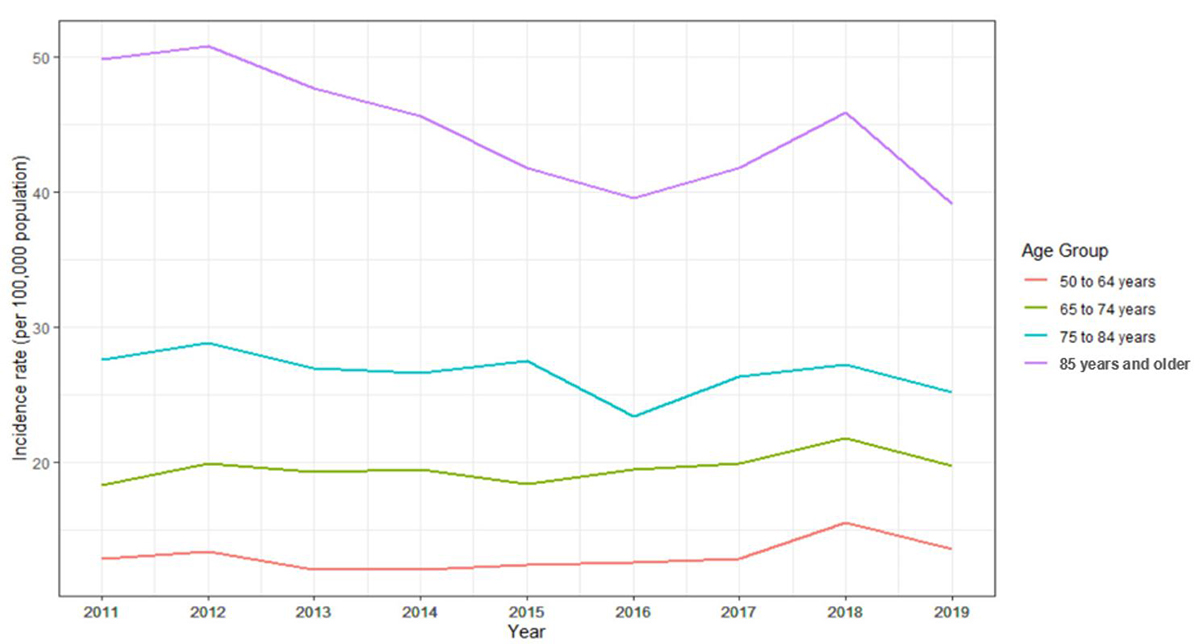
Text Description
Figure 2 shows the incidence rate of IPD in Canadians over the age of 50 per 100,000 population (vertical axis) from 2011-2019 with one-year increments (horizontal axis), grouped by age category. The age categories used compare the incidence of IPD in the Canadian adult population and are plotted in distinct colors (50-64 in red, 65 to 74 in green, 75 to 84 in turquoise, and over 85 in purple). The incidence rates were calculated using data from the ICS program for Canada's three territories, and data from CNDSS for six provinces that had line list data available (AB, BC, ON, QC, SK, and PEI).
| Year | Age group | Incidence rate (per 100,000 population) |
|---|---|---|
| 2011 | 50 to 64 years | 12.9 |
| 65 to 74 years | 18.3 | |
| 75 to 84 years | 27.6 | |
| 85 years and older | 49.8 | |
| 2012 | 50 to 64 years | 13.4 |
| 65 to 74 years | 19.9 | |
| 75 to 84 years | 28.8 | |
| 85 years and older | 50.8 | |
| 2013 | 50 to 64 years | 12.1 |
| 65 to 74 years | 19.3 | |
| 75 to 84 years | 26.9 | |
| 85 years and older | 47.6 | |
| 2014 | 50 to 64 years | 12.0 |
| 65 to 74 years | 19.5 | |
| 75 to 84 years | 26.6 | |
| 85 years and older | 45.7 | |
| 2015 | 50 to 64 years | 12.4 |
| 65 to 74 years | 18.3 | |
| 75 to 84 years | 27.5 | |
| 85 years and older | 41.8 | |
| 2016 | 50 to 64 years | 12.6 |
| 65 to 74 years | 19.5 | |
| 75 to 84 years | 23.4 | |
| 85 years and older | 39.5 | |
| 2017 | 50 to 64 years | 12.8 |
| 65 to 74 years | 19.9 | |
| 75 to 84 years | 26.3 | |
| 85 years and older | 41.8 | |
| 2018 | 50 to 64 years | 15.6 |
| 65 to 74 years | 21.8 | |
| 75 to 84 years | 27.2 | |
| 85 years and older | 45.8 | |
| 2019 | 50 to 64 years | 13.6 |
| 65 to 74 years | 19.7 | |
| 75 to 84 years | 25.2 | |
| 85 years and older | 39.1 |
The Toronto Invasive Bacterial Diseases Network (TIBDN) Footnote 14, an active surveillance program in Metropolitan Toronto and the Peel region, found that between 2012/2013 and 2018/2019, the incidence of IPD in adults aged 15 to 64 years increased significantly from 3.7 to 5.4 cases/100,000/year. During this same period, the incidence of IPD in adults aged 65 years and older decreased from 22.8 to 18.7 cases/100,000/year; however, this change was not significant. TIBDN also found that from 2018/2019 to 2020, IPD incidence in adults aged 15 to 64 years decreased from 5.4 to 2.6 cases/100,00/year, and IPD incidence in adults 65 years and older decreased from 18.7 to 8.7 cases/100,000/year.
III.1.2 IPD incidence in Northern Canada
The age-standardized incidence rate in Northern Canada, based on the data submitted to ICS, was significantly higher (25.8 cases per 100,000 population, 95% CI: 23.5 to 28.1%) than the rest of Canada (9.1 cases per 100,000 population, 95% CI: 9.1 to 9.2%) between 2001 and 2019 (Figure 3) Footnote 15.
In northern Canada, the IPD incidence rate in Indigenous Canadians was significantly higher at 31.3 cases per 100,000 population per year compared with non-Indigenous Canadians at 7.0 cases per 100,000 population per year (p<0.0001) for the same time period Footnote 15.
Figure 3. Annual incidence rate of IPD in northern Canada, ICS 2001-2021, and rest of Canada, 2001-2019, CNDSS
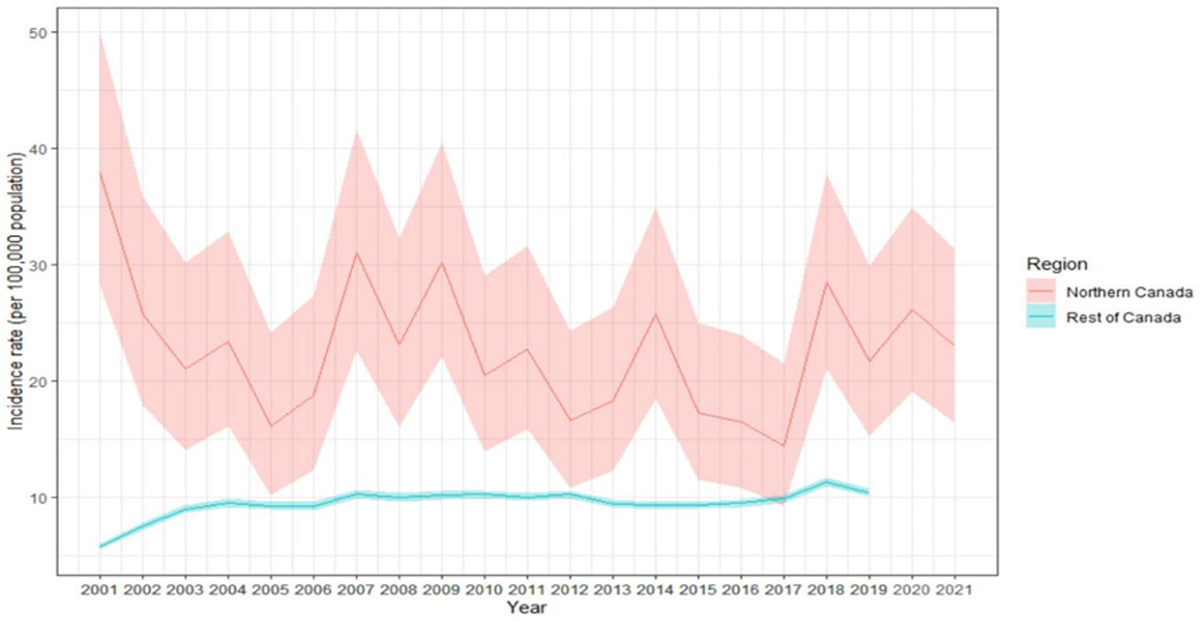
Text Description
Figure 3 shows the comparison of annual IPD incidence rates with 95% confidence intervals between Northern Canada (in red) and the rest of Canada (in blue) per 100,000 population (vertical axis) from 2001-2021 (horizontal axis). Data from Northern Canada was extracted from the ICS program and includes Canada’s three territories (Nunavut, Yukon, and Northwest territories), as well as Northern Labrador and Northern Quebec. Data for the rest of Canada came from CNDSS. IPD data for the rest of Canada for the years 2020-2021 were not yet available.
The incidence rate of IPD was consistently and significantly higher in Northern Canada when compared to the rest of Canada, with an exception of the year 2017, which was the minimum IPD incidence rate in Northern Canada at around 15 cases per 100,000 population. In this year, the incidence was still higher in Northern Canada but not significantly. The maximum overall IPD incidence rate Northern Canada occurred in 2001 with 38 cases per 100,000 population. The incidence rate subsequently decreased to 16 cases per 100,000 population in 2005 following the introduction of pediatric pneumococcal immunization in Canada. Since 2005, the IPD incidence rate fluctuated yet remained relatively stable, and was most recently calculated as 23 cases per 100,000 population in 2021. IPD cases have remained slightly elevated from 2018 to 2021 when compared to 2015 to 2017.
| Year | Northern Canada Crude incidence (per 100,000 population) | Rest of Canada Crude incidence (per 100,000 population) |
|---|---|---|
| 2001 | 37.95 | 5.58 |
| 2002 | 25.78 | 7.24 |
| 2003 | 21.02 | 8.66 |
| 2004 | 23.39 | 9.19 |
| 2005 | 16.12 | 8.94 |
| 2006 | 18.78 | 8.92 |
| 2007 | 31.07 | 9.94 |
| 2008 | 23.12 | 9.67 |
| 2009 | 30.23 | 9.83 |
| 2010 | 20.51 | 9.90 |
| 2011 | 22.74 | 9.69 |
| 2012 | 16.61 | 9.92 |
| 2013 | 18.32 | 9.14 |
| 2014 | 25.71 | 9.00 |
| 2015 | 17.30 | 9.04 |
| 2016 | 16.49 | 9.19 |
| 2017 | 14.46 | 9.59 |
| 2018 | 28.49 | 10.96 |
| 2019 | 21.72 | 10.08 |
III.2 Distribution of IPD Serotypes in Canada, 2016 – 2020
Distribution of IPD Serotypes in Canada, 2016 – 2020
From 2016 to 2020, a combined 15,234 isolates of S. pneumoniae causing invasive disease were characterized by the NML with 34% of these being identified from adults 65 years of age or older. The majority of IPD cases were caused by vaccine-contained serotypes (Figure 4). Serotypes 3 and 22F were identified as the most common causes of IPD overall and in older adults based on isolates submitted to NML (Figure 4).
Overall, the proportion of IPD isolates covered by each vaccine (PNEU-C-13, PNEU-C-15/non-PNEU-C-13, PNEU-C-20/non-PNEU-C-15 and PNEU-P-23/non-PNEU-C-20) have remained relatively stable since 2016 (Figure 5). In 2020, among adults 65 years old or older, 27.4% of circulating serotypes were covered by PNEU-C-13, 40.6% were covered by PNEU-C-15, 55.8% were covered by PNEU-C-20 and 66.9% were covered by PNEU-P-23. Circulating serotypes not covered by any pneumococcal vaccine amounted to 33.1%.
Serotype distribution for IPD among adults are summarized in Appendix A, Tables 21-23.
Figure 4. Proportion of isolates of invasive S. pneumoniae for all ages and adults 65 years and older in Canada, by serotype, 2016 to 2020, combined total

* Component of PNEU-C-13; ** Component of PNEU-C-15; ^ Component of PNEU-C-20; ~ Component of PNEU-P-23; ‡ Number of isolates for all ages and adults 65 years and older, respectively (2016-2020, combined total).
Text Description
Figure 4 shows a bar graph displaying the percentage of Streptococcus pneumoniae serotypes from 2016 to 2020 (combined total) based on the total number of isolates tested annually, for all ages and adults ≥65 years.
| Serotype (n by age group) | All ages (n=15234) | ≥65 years (n=5860) |
|---|---|---|
| 1* (5,1)‡ | 0.0% | 0.0% |
| 3* (1638,653) | 10.8% | 11.1% |
| 4* (1120,194) | 7.4% | 3.3% |
| 6A* (51,31) | 0.3% | 0.5% |
| 6B* (46,32) | 0.3% | 0.5% |
| 7F* (509,83) | 3.3% | 1.4% |
| 9V* (157,44) | 1.0% | 0.8% |
| 14* (75,32) | 0.5% | 0.5% |
| 18C* (45,13) | 0.3% | 0.2% |
| 19A* (767,275) | 5.0% | 4.7% |
| 19F* (333,125) | 2.2% | 2.1% |
| 23F* (12,2) | 0.1% | 0.0% |
| 22F** (1346,624) | 8.8% | 10.6% |
| 33F** (500,183) | 3.3% | 3.1% |
| 8^ (865,239) | 5.7% | 4.1% |
| 10A^ (304,117) | 2.0% | 2.0% |
| 11A^ (473,227) | 3.1% | 3.9% |
| 12F^ (654,129) | 4.3% | 2.2% |
| 15B/C^ (519,178) | 3.4% | 3.0% |
| 2~ (5,1) | 0.0% | 0.0% |
| 9N~ (933,361) | 6.1% | 6.2% |
| 17F~ (156,73) | 1.0% | 1.2% |
| 20~ (542,135) | 3.6% | 2.3% |
| 6C (298,172) | 2.0% | 2.9% |
| 7C (198,106) | 1.3% | 1.8% |
| 15A (641,381) | 4.2% | 6.5% |
| 16F (384,191) | 2.5% | 3.3% |
| 23A (574,301) | 3.8% | 5.1% |
| 23B (482,198) | 3.2% | 3.4% |
| 31 (235,124) | 1.5% | 2.1% |
| 34 (144,73) | 0.9% | 1.2% |
| 35B (348,194) | 2.3% | 3.3% |
| 35F (248,128) | 1.6% | 2.2% |
| 38 (192,92) | 1.3% | 1.6% |
| Other (435,148) | 2.9% | 2.5% |
Figure 5 shows the proportion of IPD isolates by year among all isolates tested and older adults. In 2020, the proportion of isolates with PNEU-C-20/non-PNEU-C-13 (i.e., serotypes 8, 10A, 11A, 12F, 15B/C, 22F and 33F) among all IPD cases accounted for 30.4% and among IPD cases in adults 65 years old or older, for 28.4%. The proportion of IPD isolated covered by each vaccine among younger adults 18 to 49 and 50 to 64 years of age is shown in Appendix A, Figure 6.
Figure 5. Proportion of IPD isolates from 2016 to 2020 by vaccine, for all ages and adults 65 years of age and older

*Vaccine serotypes include PNEU-C-13 (1, 3, 4, 5, 6A/C, 6B, 7F, 9V, 14, 19A, 19F, 18C, 23F); PNEU-C-15 (all PNEU-C-13 plus 22F and 33F); PNEU-C-20 (All PNEU-C-15 plus 8, 10A, 11A, 12F, 15B/C) and PNEU-P-23 (PNEU-C-20 serotype except 6A, plus 2, 9N, 17F, 20); NVT = all serotypes not included in PNEU-C-13, PNEU-C-15, PNEU-C-20 and PNEU-P-23. Serotype 6C included in PNEU-C-13 Serotypes due to cross protection with 6A. Serotypes 15B and 15C were grouped together as 15B/C because of reported reversible switching between them in vivo during infection, making it difficult to precisely differentiate between the two types.
Text Description
Figure 5 shows a stacked bar graph displaying the percentage of Streptococcus pneumoniae collected from each vaccine category (PNEU-C-13, PNEU-C-15/non-PNEU-C-13, PNEU-C-20/non-PNEU-C-15, PNEU-P-23/non-PNEU-C-20 and other non-vaccine serotypes), for all ages and adults ≥65 years, from 2016 to 2020.
| Age Group | Year | PNEU-C-13 (%, N) |
PNEU-C-15/ non-PNEU-C-13 (%, N) |
PNEU-C-20/ non-PNEU-C-15 (%, N) |
PNEU-P-23/ non-PNEU-C-20 (%, N) |
NVT (%, N) |
Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Ages | 2016 | 32.9% | (938) | 12.6% | (360) | 18.4% | (526) | 8.8% | (251) | 27.3% | (780) | (2855) |
| 2017 | 32.2% | (1054) | 11.9% | (390) | 17.7% | (578) | 11.3% | (371) | 26.8% | (877) | (3270) | |
| 2018 | 33.0% | (1099) | 11.7% | (388) | 19.1% | (634) | 10.7% | (357) | 25.5% | (850) | (3328) | |
| 2019 | 32.6% | (1198) | 13.8% | (507) | 17.3% | (637) | 11.5% | (423) | 24.7% | (908) | (3673) | |
| 2020 | 36.4% | (767) | 9.5% | (201) | 20.9% | (440) | 11.1% | (234) | 22.1% | (466) | (2108) | |
| ≥65 years | 2016 | 29.1% | (307) | 12.7% | (134) | 16.8% | (177) | 7.2% | (76) | 34.2% | (360) | (1054) |
| 2017 | 26.5% | (355) | 12.7% | (171) | 15.9% | (213) | 10.4% | (139) | 34.6% | (464) | (1342) | |
| 2018 | 28.8% | (367) | 14.2% | (181) | 15.1% | (192) | 9.9% | (126) | 32.0% | (408) | (1274) | |
| 2019 | 29.3% | (431) | 15.4% | (226) | 13.5% | (199) | 10.1% | (149) | 31.7% | (467) | (1472) | |
| 2020 | 27.4% | (197) | 13.2% | (95) | 15.2% | (109) | 11.1% | (80) | 33.0% | (237) | (718) | |
Distribution of IPD serotypes in Northern Canada
IPD distribution in Northern Canada was assessed using data from all five Arctic regions captured in the ICS system. Overall, there were 159 isolates of invasive S. pneumoniae characterized between 2016 and 2020: 26% of S. pneumoniae isolates were PNEU-C-13 serotypes, 14% were PNEU-C-15/non-PNEU-C-13 serotypes, 23% were PNEU-C-20/non-PNEU-C-15 serotypes, 20% were PNEU-P-23/non-PNEU-C-20 serotypes, and 16% were NVT serotypes. However, trends were difficult to ascertain due to the small number of cases and relatively smaller population in the North.III.3 Burden of Pneumococcal community acquired pneumonia in Canada
Using CIRN SOS Network data from 13 hospitals across five provinces, Leblanc et al. (2022) reported on CAP incidence in hospitalized adults from 2010 to 2017 Footnote 16. During this period, 14.2% (1264/8912) of all-cause CAP was found to be caused by S. pneumoniae with 64.1% (811/1264) being non-bacteremic, and 35.9% (455/1264) being bacteremic. Among pCAP cases in adults, 49.8% occurred in those over 65 years of age, 31.3% in those 50 to 64 years of age and 19.0% in those 16-49 years of age. Among all pCAP cases, 89.1% had one or more co-morbidity, and 28.6% had an immunocompromising condition. Of all S. pneumoniae CAP cases captured during the study period, the serotype distribution showed serotypes 3, 7F, 9N, 11A, 19A, and 22F as common.
Data from the 2018 to 2019 Discharge Abstract Database (Canadian Institute for Health Information 2022) reported inpatient CAP cases per 100,000 with pneumonia as a significant diagnosis (excluding pneumonia due to influenza). These data showed that for adults 75 years of age and older, there were 5,104 cases/100,000 population in Northern Canada and 2,846 cases/100,000 population across the rest of Canada; for adults 60 to 74, there were 1,777/100,000 population cases in Northern Canada and 871/100,000 population across the rest of Canada; and for adults 50 to 64 years, there were 569 cases/100,000 population in Northern Canada and 348 cases/100,000 population across the rest of Canada.
III.4 High Risk Groups
The TIBDN Footnote 17 found that, in their population, IPD incidence among individuals aged 15 to 64 years with chronic underlying illness increased significantly from 7.3 cases/100,000/year in 2012 to 11.0 cases/100,000/year in 2019. During the same time period, the IPD incidence among adults aged 65 years and older decreased in those with underlying illness mainly because IPD cases due to PNEU-C-13 contained serotypes decreased from 10.0 to 4.6 cases/100,000/year in people with an underlying chronic illness, and from 27.0 to 16.0 cases/100,000/year in people with immunocompromising conditions.
The Calgary Area Streptococcus pneumonia Epidemiology Research (CASPER) Footnote 18 program, an active surveillance program in Calgary, found that between 2000 to 2013, IPD incidence rate among adults with underlying comorbidities decreased by 37% [from 11.8 cases/100,000/year before the introduction of pneumococcal conjugate vaccines (2000-2001) to 7.4 cases/100,000/year in the post-PNEU-C-13 period (2010-2013)].
III.5 Summary of Pneumococcal Immunization Coverage in Canada
The Vaccine Coverage and Effectiveness Monitoring program at PHAC collects pneumococcal vaccination coverage information among Canadians as part of the seasonal influenza vaccination coverage survey Footnote 19. The most recent survey conducted over the 2020-2021 influenza season showed that about 55% of adults 65 years of age and over reported receiving a pneumococcal vaccine in adulthood. The coverage was higher for females (60%) than males (40%). Overall, 26% of adults 18 to 64 years old with underlying medical conditions reported receiving pneumococcal vaccination. The survey did not differentiate between the two different pneumococcal vaccines recommended for adults.
IV. Vaccine
IV.1 Preparations authorized for use in Canada
Four preparations of pneumococcal vaccine are currently authorized for use in adults in Canada (Table 2).
PNEU-C-13 (Prevnar®13) Footnote 20 is a sterile solution of polysaccharide capsular antigen of 13 serotypes of S. pneumoniae (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F). The antigens are individually conjugated to a diphtheria, Corynebacterium diphtheriae (CRM197), protein carrier. The CRM197 protein carrier is adsorbed on aluminum phosphate as an adjuvant. Each dose of vaccine contains 4.4 mcg of the 6B polysaccharide, and 2.2 mcg each of the remaining polysaccharides. PNEU-C-13 is available as a 0.5mL single dose, prefilled syringe.
PNEU-C-15 (Vaxneuvance®) Footnote 21 is a sterile suspension of purified capsular polysaccharides from 15 serotypes of S. pneumoniae (PCV13 serotypes plus serotypes 22F and 33F). The antigens are individually conjugated to diphtheria CRM197 protein carrier. This CRM197 protein carrier is adsorbed on aluminum phosphate as an adjuvant. Each dose of vaccine contains 32 mcg of total pneumococcal polysaccharide (2.0 mcg each of polysaccharide Serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F, and 33F, and 4.0 mcg of polysaccharide serotype 6B) conjugated to 30 mcg of CRM197 carrier protein. PNEU-C-15 is available as a 0.5mL single-dose prefilled syringe.
PNEU-C-20 (Prevnar 20TM) Footnote 22 is a sterile saccharide suspension of the capsular antigens of 20 serotypes of S. pneumoniae (PCV13 serotypes + serotypes 8, 10A, 11A, 12F, 15B, 22F, and 33F). The antigens are individually conjugated to non-toxic diphtheria CRM197 protein. This CRM197 protein carrier is absorbed on aluminum phosphate as an adjuvant. Each dose of vaccine contains 4.4 mcg of the 6B polysaccharide, and 2.2 mcg each of the remaining polysaccharides. PNEU-C-20 is supplied as a 0.5mL single dose prefilled syringe.
PNEU-P-23 (Pneumovax®23) Footnote 23 is a sterile solution of 23 highly purified capsular polysaccharides (PCV13 serotypes with the exception of 6A, plus serotypes 2, 9N,17F, and 20). PNEU-P-23 is available as a single-dose vial containing 0.5 ml of liquid vaccine and a 0.5mL single dose prefilled syringe.
| PREVNAR® 13 (PNEU-C-13) |
VAXNEUVANCE® (PNEU-C-15) |
PREVNAR 20TM (PNEU-C-20) |
PNEUMOVAX 23® (PNEU-P-23) |
|
|---|---|---|---|---|
| Manufacturer | Pfizer | Merck | Pfizer | Merck |
| Date of initial authorization in Canada | December 21, 2009 | November 16, 2021 | May 9, 2022 | December 23, 1983 |
| Type of vaccine | Conjugate vaccine | Conjugate vaccine | Conjugate vaccine | Polysaccharide vaccine |
| Composition | 2.2 mcg of each saccharide for S. pneumoniae serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F and 23F, 4.4 mcg of saccharide for serotype 6B, 34 mcg of CRM197 carrier protein, 4.25 mg of sodium chloride, 100 mcg of polysorbate 80, 295 mcg of succinic acid and 125 mcg of aluminum as aluminum phosphate adjuvant and water for injection | 32 mcg of total pneumococcal polysaccharide (2.0 mcg each of polysaccharide serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F and 33F and 4.0 mcg of polysaccharide serotype 6B) conjugated to 30 mcg of CRM197 carrier protein, 125 mcg of aluminum (as aluminum phosphate adjuvant), 1.55mg of L-histidine, 1 mg of polysorbate 20, 4.50 mg of sodium chloride and water for injection |
Approximately 2.2 mcg of each of S. pneumoniae serotypes 1, 3, 4, 5, 6A, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F and 33F saccharides, 4.4 mcg of 6B saccharide, 51 mcg of CRM197 carrier protein, 100 mcg of polysorbate 80, 295 mcg of succinic acid, 4.4 mg of sodium chloride and 125 mcg of aluminum as aluminum phosphate adjuvant and water for injection | 25 mcg of capsular polysaccharides from each of S. pneumoniae serotypes 1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F and 33F, sodium chloride 0.9 % w/w, phenol 0.25% w/w and water for injection to volume |
| Schedule for immunocompetent adults | 1-dose schedule | 1-dose schedule | 1-dose schedule | 1-dose schedule |
| Route of administration | Intramuscular injection | Intramuscular injection | Intramuscular injection | Intramuscular or subcutaneous injection |
| Indications for adults | Indicated for active immunization of adults 18 years of age and older for prevention of pneumonia and invasive pneumococcal disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F | Indicated for active immunization of adults 18 years of age of older for the prevention of invasive disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, 22F, 23F and 33F | Indicated for active immunization of adults 18 years of age and older for the prevention of pneumonia and invasive pneumococcal disease caused by Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 8, 9V, 10A, 11A, 12F, 14, 15B, 18C, 19A, 19F, 22F, 23F, and 33F | Indicated for active immunization of adults 18 years of age and older for prevention of pneumococcal disease caused by pneumococcal types included in the vaccine (1, 2, 3, 4, 5, 6B, 7F, 8, 9N, 9V, 10A, 11A, 12F, 14, 15B, 17F, 18C, 19A, 19F, 20, 22F, 23F and 33F) |
Contraindications |
|
|
|
|
Precautions |
|
|
|
|
| Storage Requirements | Single-dose prefilled syringe. Refrigerate at 2°C to 8°C. Do not freeze. Store in original package | Single-dose prefilled syringe. Refrigerate at 2°C to 8°C. Do not freeze. Protect from light. Administer as soon as possible after being removed from the refrigerator | Single-dose prefilled syringe. Refrigerate at 2°C to 8°C. Store syringes horizontally in the refrigerator. Do not freeze. Administer as soon as possible after being removed from the refrigerator | Multi-dose vial. Refrigerate at 2°C to 8°C. Discard opened vial after 48 hours |
IV.2 Efficacy and effectiveness
There are currently no efficacy or effectiveness data available for PNEU-C-15 or PNEU-C-20 for any adult indication.
Recently reported systematic reviews continue to support the effectiveness of PNEU-C-13 against IPD and pneumococcal pneumonia among adults 65 and older Footnote 24 Footnote 25. Two observational studies included in the systematic review by Childs et al found a PNEU-C-13 vaccine effectiveness against pneumonia caused by vaccine-contained serotypes in the range of 38 to 68%. Three observational studies from the systematic review by Farrar et al found a PNEU-C-13 effectiveness against IPD caused by vaccine-contained serotypes in the range of 59 to 68%.
A recent systematic review Footnote 24 reported a pooled PNEU-P-23 effectiveness against IPD caused by vaccine-contained serotypes in adults 65 years of age and older to be 38%. Another systematic review Footnote 25 found a limited protection against pneumonia caused by vaccine-contained serotypes (pooled effectiveness of 18% from 3 observational studies with PNEU-P-23 given to adults 65 years and older less than 5 years before illness onset).
IV.3 Immunogenicity
IV.3.1 Measures of Immunogenicity
OPA assays were used to assess immune response for PNEU-C-15 and PNEU-C-20. While no specific threshold of OPA titer has been identified that correlates with protection against IPD or pneumonia in adults, OPA responses have been used as an established surrogate of protection to infer efficacy when comparing to an efficacious vaccine.
Previously, OPA responses were used as a surrogate marker of vaccine efficacy for IPD and pneumonia in the approval of PNEU-C-13 in adults.
IV.3.2 Immunogenicity of PNEU-C-15
Summary of PNEU-C-15 study characteristics
Immunogenicity of PNEU-C-15 was evaluated in two Phase 2 trials Footnote 26 Footnote 27 and five Phase 3 trials Footnote 28 Footnote 29 Footnote 30 Footnote 31 Footnote 32. Three studies evaluated medically stable, vaccine-naïve adults 50 years of age or older and one study focused on previously vaccinated adults 65 years of age and older. Data for adults 18 years of age and older with medical risk factors for PD were available in two studies (one as a study population subset analysis). One study evaluated adults with HIV. Most studies had participants of a majority white race and with gender balance (Table 5). Immunogenicity assessments were at a low RoB (Appendix A, Table 8).
Summary of PNEU-C-15 immunogenicity evidence
In immunocompetent pneumococcal vaccine-naïve adults 65 years of age and older, for shared serotypes, PNEU-C-15 demonstrated overall similar immune responses, including for serotype3, compared to PNEU-C-13 (Appendix A Tables 9). All analyses for serotypes not covered by PNEU-C-13 showed numerically higher responses with PNEU-C-15. However, seroresponses varied for the shared serotypes. Results from studies comparing PNEU-C-15 to PNEU-P-23 showed similar results, although seroresponse was higher with serotype3 with PNEU-C-15 (Appendix A, Tables 9 and 10).
While no studies evaluated non-inferiority for other age groups (50 to 64 years; 65 to 74 years; 75 years of age and older) observational comparisons among age groups and age subgroup data for seroresponse are reported in Appendix A, Tables 9 and 10. Non-inferiority for shared serotypes was not evaluated in the comparison with PNEU-C-13 for adults with previous PNEU-P-23 vaccination (Appendix A, Table 12), and adults with immunocompromising conditions (Appendix A, Table 14).
In pneumococcal vaccine-naïve adults over the age of 65, PNEU-C-15 administered concurrently with quadrivalent seasonal influenza vaccine, seroresponses were found to be similar for serotype 3 but numerically lower for the other shared serotypes (Appendix A, Table 11). In adults who subsequently received PNEU-P-23 following the receipt of PNEU-P-15, there was an observed numerically lower proportion of seroresponders with serotype 3, PNEU-C-15 unique serotypes, as well as some shared serotypes when compared to seroresponse rates following previous PNEU-C-13 vaccination in series with PNEU-P-23 for some shared serotypes (Appendix A, Table 15).
Non-inferiority for shared serotypes was not evaluated in the comparison with PNEU-C-13 for adults with previous PNEU-P-23 vaccination (Appendix A, Table 12), as well as people with chronic medical conditions (CMC) 18 to 64 years of age (Appendix A, Table 13) and with immunocompromising conditions (Appendix A, Table 14).
IV.3.3. Immunogenicity of PNEU-C-20
Summary of PNEU-C-20 study characteristics
Immunogenicity of PNEU-C-20 was evaluated in one Phase 2 trial3 Footnote 33 and two Phase 3 trials Footnote 34 Footnote 35. Two trials evaluated vaccine-naïve healthy adults, as well as adults with underlying CMCs. Of these studies, one recruited participants 60 to 64 years of age while the other enrolled participants 18 years of age or older into three age cohorts (i.e., 18 to 49, 50 to 59, 60 years and older). One study evaluated immune responses in previously PNEU-P-23 vaccinated adults 65 years of age or older. Studies were assessed to be at low RoB (Appendix A, Table 8).
Summary of PNEU-C-20 immunogenicity evidence
Non-inferiority criteria were met following the administration of PNEU-C-20 in vaccine-naïve populations over age 60. However, there was an observed lower proportion of seroresponders compared to PNEU-C-13 for shared serotypes (Appendix A, Table 16). While PNEU-C-20 was not directly compared to PNEU-C-13 or PNEU-P-23, individuals previously vaccinated with PNEU-P-23, PNEU-C-13 or both, showed robust immune responses following PNEU-C-20 vaccination (Appendix A, Tables 17 and 18). PNEU-C-20 was not evaluated in adults with immunocompromising conditions.
IV.4 Persistence of Immune Response
Persistence of PNEU-C- 15 immune response
Persistence of PNEU-C-15 immune response was observed 8 weeks Footnote 29, 6 months Footnote 30 and 1 year Footnote 31 following the sequential administration of PNEU-P-23 in adults 18 years of age or older living with immunocompromising conditions, in adults 18 to 49 living with CMCs and in healthy adults 65 years of age or older. In general, OPA GMTs at 8 weeks, 6 months and 1 year were lower than at day 30 post PNEU-C-15 vaccination but higher than at baseline. PNEU-C-15 elicited an immune response that was comparable to PNEU-C-13 at 30 days and 8 weeks, 6 months, and 12 months post- vaccination for the 13 shared serotypes and higher than PNEU-C-13 for the 2 serotypes 22F and 33F unique to PNEU-C-15.
Persistence of PNEU-C-20 immune response
Persistence of PNEU-C-20 immune response was observed at 12 months in healthy adults aged 60 through 64 years with no history of pneumococcal vaccination Footnote 33. OPA GMTs at 12 months declined compared with those at 30 days after vaccination but remained elevated above baseline. The same pattern of antibody decline in the 12 months after vaccination has previously been observed with PNEU-C-13. However, vaccine effectiveness against pneumonia caused by serotypes in the vaccine did not decline through 4 years of follow-up Footnote 36.
IV.5 Vaccine Administration and Schedule
PNEU-C-15 and PNEU-C-20 are supplied in a single-dose, prefilled syringe.
A 0.5mL dose of PNEU-C-15 should be administered intramuscularly. The standard schedule for immunization is one dose. The need for a booster dose or re-immunization is not indicated. Please see the product monograph for additional details Footnote 21.
A 0.5mL dose of PNEU-C-20 should be administered intramuscularly. The standard schedule for healthy adults is one dose. Please see the product monograph for additional details Footnote 22.
IV.6 Serological Testing
Serological testing is not recommended before or after receiving pneumococcal vaccine.
IV.7 Storage Requirements
PNEU-C-15 should be refrigerated at 2°C to 8°C. The vaccine should not be frozen. Protect the vaccine from light. The prefilled syringes should be administered as soon as possible after being removed from the refrigerator Footnote 21.
PNEU-C-20 should be refrigerated at 2°C to 8°C. The pre-filled syringes should be stored horizontally in the refrigerator to minimize the re-dispersion time. The vaccine should be discarded if it has been frozen. The vaccine should be administered as soon as possible after being removed from the refrigerator Footnote 22.
IV.8 Concurrent Administration with Other Vaccines
PNEU-C-15 and PNEU-C-20 can be concurrently administered with quadrivalent inactivated influenza vaccine (QIV) in adults, as concurrent administration has been demonstrated to be immunogenic and safe Footnote 37. However, lower pneumococcal OPA GMTs were reported when pneumococcal vaccines were co-administered with QIV compared with when pneumococcal vaccines were given alone Footnote 32 Footnote 37 Footnote 38. No data are available on co-administration of PNEU-C-15 or PNEU-C-20 with other adult vaccines. Preliminary data on the co-administration of PNEU-C-20 and the Pfizer-BioNTech Comirnaty mRNA COVID-19 vaccine showed no significant interference in the immune response Footnote 39.
IV.9 Vaccine Safety
Summary of PNEU-C-15 study characteristics
Safety of PNEU-C-15 was evaluated in two Phase 2 trials Footnote 26 Footnote 27 and five Phase 3 trials Footnote 28 Footnote 29 Footnote 30 Footnote 31 Footnote 32. Data on local and systemic AEs were solicited through electronic vaccine report cards for two weeks after each dose, as well as follow up for serious events for 6 months. Reported outcomes included SAEs, vaccine-related SAEs, as well as mild/moderate and severe systemic AEs (i.e., fever, fatigue, headache, muscle, and joint pain). Safety data was reported for pneumococcal vaccine-naïve individuals, concurrent administration with season influenza vaccine, and for specific populations of interest including adults aged 18 to 64 years with chronic medical or immunocompromising conditions, and previously vaccinated adults aged 65 years or older. Six studies were at low RoB for all domains. In one study the reasons for missing data were not reported in the assessment of SAEs and vaccine-related SAEs, which is challenging.
Summary of PNEU-C-15 Safety
There was little to no difference reported in clinical trials between PNEU-C-15 and PNEU-P-23 or PNEU-C-13 for all mild/moderate and severe systemic AEs occurring within 14 days of vaccination as well as reported SAEs up to six months after vaccination in all evaluated populations (Appendix A, Tables 9, 10 and 13 to 15). Results were similar following sequential administration of PNEU-P-23 after PNEU-C-15 or PNEU-C-13 in adults 65 years of age or older with an immunocompromising condition (Appendix A, Tables 14 and 15).
There was little to no difference in SAEs for PNEU-C-15 administered concomitantly with QIV for vaccine-naïve adults (Appendix A, Table 11). Results were similar with respect to severe fatigue, joint and muscle pain up to 14 days after vaccination. There was no difference between groups for severe and mild/moderate systemic AEs.
Summary of PNEU-C-20 study characteristics
The safety of PNEU-C-20 was primarily evaluated for GRADE in one Phase 2 trial Footnote 33 and two Phase 3 trials Footnote 34 Footnote 35. Data were available for pneumococcal vaccine-naïve adults 18 years of age and older, and previously vaccinated adults 65 years of age and older. The full safety evaluation included 6 pre-licensure clinical trials, with safety data collection including solicited local reactions within 10 days of vaccination and systemic events within 7 days. Unsolicited events were collected for 1 month after vaccination and SAEs and newly diagnosed CMCs within 6 months after vaccination.
Safety of PNEU-C-20
There was little to no difference between PNEU-C-20 and PNEU-C-13 in SAEs up to one month post-vaccination for vaccine-naïve adults aged 60 years or older. Results showed no difference for all mild/moderate and severe systemic AEs up to seven days post-vaccination. Certainty of evidence varied across assessments ranging from moderate to high (Appendix A, Table 16).
For adults 65 years of age and older previously vaccinated with PNEU-P-23 one to five years prior, SAEs up to six months and systemic AEs 7 days after vaccination were similar between PNEU-C-20 and PNEU-C-13 (Appendix A, Table 18). Findings were similar when PNEU-C-20 and PNEU-P-23 were compared among those previously vaccinated with PNEU-13 at least six months prior (Appendix A, Table 17).
IV.10 Contraindications and Precautions
PNEU-C-15 and PNEU-C-20 are contraindicated in individuals with a history of a severe allergic reaction (e.g., anaphylaxis) to any component of the vaccine or any diphtheria toxoid-containing vaccine. Administration of vaccine should be postponed in persons suffering from acute severe febrile illness.
V. Vaccination of Specific Populations
V.1. Immunization in Pregnancy and Breastfeeding
There are no adequate and well-controlled studies of PNEU-C-15 and PNEU-C-20 in individuals who are pregnant or breastfeeding.
V.2. Immunization of Immunocompromised persons
Individuals with altered immunocompetence, including those receiving immunosuppressive therapy, may have a reduced immune response to the vaccine.
VI. Ethics, Equity, Feasibility and Acceptability Considerations
NACI uses a published, peer-reviewed framework and evidence-informed tools to ensure that issues related to ethics, equity, feasibility, and acceptability (EEFA) are systematically assessed and integrated into its guidance Footnote 40.
NACI evaluated the following ethical considerations when making its recommendations: promoting well-being and minimizing risk of harm, maintaining trust, respect for persons and fostering autonomy, and promoting justice and equity. NACI took into account the available evidence from the clinical studies of PNEU-C-15 and PNEU-C-20 along with the real-world evidence on the effectiveness and safety of currently available pneumococcal vaccines PNEU-C-13 and PNEU-P-23, as well as data on the burden of illness of PD and evolving serotype distribution, and risk factors in particular for IPD.
Achieving coverage of 80% of adults 65 years old or older vaccinated with a pneumococcal vaccine, as well as reducing overall burden of disease by 5% by 2025, is one of the goals of the Canadian national immunization strategy. However, vaccine uptake in adults 65 years of age or older is well below the target, with approximately 55% reporting receiving a pneumococcal vaccine in Canada. Uptake is even lower among younger adults 18 to 64 years of age with underlying medical conditions that predispose them to PD at approximately 26%). A survey conducted in Quebec in 2020 reported that lack of awareness that the pneumococcal vaccine is needed or recommended is the most frequent reason for not being vaccinated.
The new higher-valent pneumococcal conjugate vaccines offer an opportunity to protect individuals against additional serotypes and further reduce the burden of disease in adults. PNEU-C-20 covers more than 90% of serotypes included in PNEU-P-23, with the additional benefits of conjugate vaccines. Thus, PNEU-C-20 may be offered in programs as a single dose without a subsequent dose of PNEU-P-23, unlike PNEU-C-15 which is recommended to be administered in series with PNEU-P-23 to optimize protection. A single dose vaccine schedule minimizes complexity and cost in a vaccine program and can facilitate vaccination of populations that are otherwise difficult to reach to complete a series requiring more than one dose.
Among factors that may contribute to health inequity as described in NACI’s EFFA framework, pre-existing disease, social factors, place of residence, and age are important to consider with pneumococcal recommendations. Pneumococcal disease burden increases with age and adults with pre-existing conditions are at greater risk. Therefore, by providing age-based and risk-based recommendations as well as inclusion of settings of higher disease burden, inequity may be reduced.
First Nations, Metis, or Inuit communities in Canada have a younger age distribution compared to the general Canadian population but have also been observed to have increased risk for severe PD due to a variety of intersecting factors including underlying medical conditions and potential decreased access to health care. Therefore, age-based recommendations may need to be modified to offer effective protection to individuals in these communities. Autonomous decisions should be made by Indigenous Peoples with the support of healthcare and public health partners in accordance with the United Nations Declaration on the Rights of Indigenous Peoples.
VII. Economics
A systematic review, de novo model-based economic evaluation, and a multi-model comparison were used as economic evidence to support decision-making for the use of PNEU-C-15 and PNEU-C-20.
Full details of these analysis, including assumptions and limitations, are provided in a supplementary appendix.
A review of the peer-reviewed and grey literature identified four cost-utility studies of PNEU-C-15 and PNEU-C-20 compared to current vaccination recommendations for adults in the United States (that are PNEU-P-23 plus optional PNEU-C-13 under shared clinical decision-making for adults aged 65 years or older; PNEU-P-23 at diagnosis of CMCs if under age 65 years; and PNEU-C-13 in series with PNEU-P-23 at diagnosis of immunocompromising condition if under age 65 years) Footnote 41. The studies generally found that PNEU-C-20 use in older adults was associated with increased QALYs, and with lower ICERs when the vaccine was used in adults aged 65 years and older compared to programs in adults aged 50 years and older. ICER estimates for PNEU-C-15 use in series with PNEU-P-23 at age 65 showed variability across studies. The estimated impact of adding risk-based programs for younger adults with IC/CMC to an age-based strategy depended on the vaccine product, with lower ICERs reported for PNEU-C-20 than for PNEU-C-15 in series with PNEU-P-23.
A cost-utility model developed by NACI was used to evaluate the cost-effectiveness of different age-based recommendations for PNEU-C-15 and PNEU-C-20 vaccines (used alone or in series with PNEU-P-23) in the Canadian population compared to current recommendations. Results are presented for the health system perspective. The base-case analysis, supported by scenario analyses, indicated that PNEU-C-20 used alone is likely a cost-effective strategy at age 65 or 75, with ICERs ranging from $6,500 to $17,400 per QALY gained. The ICERs for PNEU-C-20 at age 50 were higher than for ages 65 or 75. In sequential analysis that compared all possible vaccination strategies, PNEU-C-15 was dominated (more costly and less effective) or subject to extended dominance (i.e., would never be the optimal option regardless of the cost-effectiveness threshold) by PNEU-C-20. PNEU-C-20 plus PNEU-P-23 at age 65 or age 75 had ICERs ranging from 80,000 to $113,500 per QALY gained. Findings were sensitive to the assumed vaccine prices for PNEU-C-15 and PNEU-C-20 (see supplementary appendix). Analysis of populations in Northern Canada showed similar trends as the rest of Canada.
In a multi-model comparison, three cost-utility models with harmonized parameter values and using the same health system perspective and discount rate, showed qualitatively consistent results despite differing model structures and assumptions. The comparison supported the finding that, based on currently available data, PNEU-C-20 used alone ($4,100-106,000 per QALY gained) could be a cost-effective strategy for use in the adult Canadian population, depending on the cost-effectiveness threshold used. All models estimated PNEU-C-15 or PNEU-C-15 in series with PNEU-P-23 to be dominated (more costly and less effective) or subject to extended dominance (would never be the optimal option regardless of the cost-effectiveness threshold) by PNEU-C-20.
VIII. Recommendations
Following the review of available evidence summarized above, NACI makes the following recommendations for public health level decision-making. Considerations in the management options table should also be reviewed in order to inform decision making.
A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present.
A discretionary recommendation may be considered for some populations/individuals in some circumstances. Alternative approaches may be reasonable.
Please see Appendix A for a more detailed explanation of strength of NACI recommendations (Table 19) and the GRADE assessment of the body of evidence (Table 6).
NACI will continue to carefully monitor the scientific developments related to pneumococcal vaccination in adults and will update recommendations as evidence evolves.
VIII.1 Recommendations for Public Health Program Level Decision-Making
In considering NACI recommendations for publicly funded immunization programs and for the purposes of publicly funded program implementation, provinces and territories may take into account other local operational factors (e.g., current immunization programs, resources). Recognizing that there are differences in operational contexts across Canada, jurisdictions may wish to refer to Management Options Tables 3 and 4 below for a summary of the considerations for using different products (e.g., with respect to cost-effectiveness and feasibility).
For adults not previously vaccinated with a pneumococcal vaccine, or adults whose vaccination status is unknown
- NACI recommends that pneumococcal conjugate vaccine PNEU-C-20 should be offered to pneumococcal vaccine naïve adults or adults whose vaccination status is unknown and who are 65 years of age and older, or who are 50 to 64 years of age living with risk factors placing them at higher risk of pneumococcal disease, or who are 18 to 49 years of age living with immunocompromising conditions. (Strong NACI recommendation).
Summary of evidence and rationale
- Conjugate vaccines induce memory, provide longer duration of protection, and provide ability for boosting by involving T cells in a way that polysaccharide vaccines cannot. The more durable protection offered by conjugate vaccines may result in fewer cases of PD, even though they protect against fewer serotypes than polysaccharide vaccine.
- In immunocompetent adults 65 years of age and older, PNEU-C-20 has been demonstrated to produce a similar (non-inferior) immune response compared to PNEU-C-13, although immune responses were noted to be lower following PNEU-C-20, and superior immune responses compared to PNEU-C-23 for shared serotypes.
- No PNEU-C-20 studies in immunocompromised adults have been conducted. Among persons with ICs for PD, PNEU-C-20 is expected to be similarly efficacious as PNEU-C-13 against disease attributable to the 13 matched serotypes.
- PNEU-C-20 has a comparable safety profile to PNEU-C-13 in adults.
- Immunization of older adults with PNEU-C-20 vaccine is expected to be cost-effective, based on the current burden of IPD and assumptions regarding pricing of the PNEU-C-15, PNEU-C-20, and PNEU-P-23.
- Individuals at increasing age and/or with certain underlying medical conditions (both non-immunocompromising and immunocompromising) and other risk factors are at higher risk of IPD (see Table 1). Adults 65 years of age and older have the highest incidence rate of IPD compared to other adult age groups, followed by adults 50 to 64 years of age. However, the benefit of vaccinating adults 50 to 64 with underlying medical conditions or other risk factors that place them at higher risk for IPD are anticipated to be greater than vaccinating all adults in this age group.
- Age-based recommendations may need to be modified for communities with younger age distributions. In First Nations, Metis, or Inuit communities, autonomous decisions should be made by Indigenous Peoples with the support of healthcare and public health partners in accordance with the United Nations Declaration on the Rights of Indigenous Peoples.
- Current uptake of pneumococcal vaccines among older adults and adults living with underlying medical conditions, both non-immunocompromising and immunocompromising, is well below national goals.
- Program feasibility and vaccine acceptability and uptake may be superior with single dose PNEU-C-20 as compared to a PNEU-C-15 + PNEU-P-23 strategy, the latter of which would require coordination of two doses of different vaccine products.
- NACI recommends that PNEU-C-15 followed by PNEU-P-23 may be offered as an alternative to PNEU-C-20 to pneumococcal vaccine naïve adults or adults whose vaccination status is unknown and who are 65 years of age and older, or who are 50 to 64 years of age living with risk factors placing them at higher risk of pneumococcal disease, or who are 18 to 64 years of age living with immunocompromising conditions. (Discretionary NACI recommendation)
Summary of evidence and rationale
- In immunocompetent adults 65 years of age and older, PNEU-C-15 has demonstrated to produce a similar (non-inferior) immune response compared to PNEU-C-13 for shared serotypes.
- In adults with underlying medical conditions, including ICs, PNEU-C-15 has shown comparable immune responses to PNEU-C-13 for 13 shared serotypes.
- An interval between PNEU-C-15 and PNEU-P-23 of 1 year is recommended for adults 65 years of age and older and adults 50 to 64 years of age living with risk factors for PD to provide expanded protection to 8 additional serotypes not in PNEU-C-15.
- An interval between PNEU-C-15 and PNEU-P-23 of 8 weeks is recommended for adults 18 to 64 years of age living with ICs to provide expanded protection to additional serotypes not in PNEU-C-15 allowing for quicker completion of series in vulnerable population. A longer interval may result in less blunting of immune responses and could be considered if risk of pneumococcal infection if low.
- Although PNEU-C-15 is not expected to yield the same population-level epidemiological benefits as PNEU-C-20 and requires a second dose with PNEU-P-23, it is anticipated to improve disease outcomes compared to offering PNEU-P-23 alone.
- Although PNEU-C-20 dominated PNEU-C-15 + PNEU-P-23 in cost-effectiveness analyses, the results were sensitive to vaccine price. A large enough differential in vaccine price between PNEU-C-20 and PNEU-C-15 + PNEU-P-23 would result in similar cost-effectiveness (i.e., PNEU-C-15 + PNEU-P-23 would no longer be dominated).
For adults previously vaccinated with a pneumococcal vaccine
- NACI recommends that pneumococcal conjugate vaccine PNEU-C-20 should be offered to adults 65 years of age and older who have been immunized previously with PNEU-P-23 alone, or PNEU-C-13 and PNEU-P-23 in series, if it has been at least 5 years from the last dose of a previous pneumococcal vaccine (PNEU-P-23 or PNEU-C-13). (Strong NACI recommendation)
Summary of evidence and rationale
- Robust immune responses were reported for PNEU-C-20 in adults previously vaccinated with PNEU-P-23 alone or together with PNEU-C-13; however, the data were non-comparative to PNEU-C-13.
- PNEU-C-20 has shown little to no difference in safety profiles to PNEU-C-13 in adults 65 years of age and older previously vaccinated.
- An interval of 5 years between PNEU-P-23 and PNEU-C-20 takes advantage of the estimated effectiveness duration of PNEU-P-23 and the boosting anticipated with PNEU-C-20; it also maximizes the total duration of protection against pneumococcal infection.
- There may be benefit to offering PNEU-C-15 to adults 65 years of age and older who have received PNEU-P-23 alone if PNEU-C-20 is not available. For adults 65 years of age and older who are also at the highest risk of IPD, an additional dose of PNEU-P-23 may be offered one year later. There is limited benefit to giving PNEU-C-15 to individuals who received PNEU-C-13 as it will only offer protection against two additional serotypes.
- NACI recommends that pneumococcal conjugate vaccine PNEU-C-20 may be offered to adults 65 years of age and older who have been immunized previously with PNEU-C-13 alone, if it has been 1 year from the last dose of PNEU-C-13. (Discretionary NACI recommendation)
Summary of evidence and rationale
- Robust immune responses were reported for PNEU-C-20 in adults previously vaccinated with PNEU-C-13 only; however, the data were non-comparative to PNEU-C-13.
- An interval of 1 year between PNEU-C-13 and PNEU-C 20 is to expand serotype coverage offered by PNEU-C-13 in a time-effective manner.
- A shorter interval of 8 weeks might be considered to align with immunization clinics and/or programs.
- The additional benefit of offering PNEU-C-15 is limited as PNEU-C-15 will only offer protection against two additional serotypes. However, PNEU-C-15 in series with PNEU-P-23 or PNEU-P-23 alone can be considered if PNEU-C-20 is unavailable or inaccessible.
For hematopoietic stem cell transplant recipients
- NACI recommends that pneumococcal conjugate vaccine PNEU-C-20 should be offered to adults 18 years old or older who received a hematopoietic stem cell transplant (HSCT) after consultation with transplant specialist. A primary series of 3 doses of PNEU-C-20 starting 3 to 9 months after transplant should be administered at least 4 weeks apart, followed by a booster dose of PNEU-C-20 12 to 18 months post-transplant (6 to 12 months after the last dose of PNEU-C-20). (Strong NACI recommendation)
Summary of evidence and rationale
- No studies assessing immunogenicity and safety of PNEU-C-20 in HSCT recipients were available; however, PNEU-C-20 is expected to have similar immunogenicity and safety profiles to PNEU-C-13 in this population.
- The recommended timing of PNEU-C-20 for HSCT recipients should be determined in consultation with the recipient’s transplant specialist.
- PNEU-C-15 may be considered if PNEU-C-20 is unavailable or inaccessible to ensure these individuals will receive the needed protection.
Considerations for continued PNEU-C-13 and PNEU-P-23 use and other risk groups
- NACI supports the continued use of PNEU-C-13 and PNEU-P-23 in adults only when PNEU-C-15 and/or PNEU-C-20 are unavailable or inaccessible.
- At this time, there are no public health level recommendations on the use of PNEU-C-15 or PNEU-C-20 for adults 18 to 49 years of age with non-immunocompromising risk factors that place them at high risk of IPD as additional analyses on the cost-effectiveness of conjugate PNEU-C-15 and PNEU-C-20 in this population are needed. PNEU-C-15 or PNEU-C-20 may be considered at clinical discretion for these adults.
Management options
Options for the vaccine schedule, vaccine type (VT), age cohort and risk group are available, and the decision on which option is preferable may depend on one or more considerations outlined below.
| Options: Choice of Product |
Factors for Consideration |
Decision Points |
|---|---|---|
Pneumococcal conjugate vaccine – PNEU-C-20 |
PNEU-C-13
|
Epidemiology
Unknowns
Duration of protection
Unknowns
Immunogenicity
Unknowns
Safety
Economics Based on a cost utility analysis:
Unknowns
Feasibility/Acceptability
Unknowns
|
Pneumococcal conjugate vaccine – PNEU-C-15 |
|
|
Pneumococcal conjugate vaccine – PNEU-C-13 |
|
Feasibility/Acceptability
|
Pneumococcal polysaccharide vaccine |
|
Feasibility/Acceptability
|
| Options Age Cohorts | Factors for consideration | Decision points |
|---|---|---|
18 to 49 years of age with risk factors for IPD |
|
18 to 49 years of age
|
50 years of age and older |
|
50 years of age and older
|
65 years of age and older |
65 years of age and older
|
|
75 years of age and older |
75 years of age and older
|
IX. Research priorities
- Estimates/assessments of the PNEU-C-15 and PNEU-C-20 vaccine effectiveness in the general population of individuals 65 years of age and older and in additional populations (e.g., indigenous people, people living with chronic medical, social, and immunocompromising conditions).
- Cost-effectiveness analyses on the use of PNEU-C-15 and PNEU-C-20 in adults 18 to 49 years of age with risk factors that place them at high risk of IPD.
- Assessment of the effects of community immunity and serotype replacement of PNEU-C-15 childhood programs over time on the incidence of IPD, VT IPD, CAP, and VT CAP and on carriage within the Canadian population of individuals 65 years of age and older and in additional populations (e.g., indigenous, people living with chronic medical, social, and immunocompromising conditions).
- Estimates of efficacy and effectiveness of PNEU-C-15 and PNEU-C-20 boosters in immunocompetent adults over 65 years of age.
- Assessment of pneumococcal vaccination programs on the reduction of myocardial infarction and stoke.
X. Surveillance issues
Ongoing surveillance is fundamental to planning, implementation, evaluation, and evidence-based decision-making. (Indicate if the disease to be prevented is reportable nationally.) To support such efforts, NACI encourages surveillance improvements in the following areas:
- Nationally representative data is not currently available on the burden of CAP and VT pCAP in Canada
- National surveillance data on vaccination status are not available for identified cases of IPD and VT IPD in Canada, which limits extension of findings
- National surveillance on pneumococcal vaccine coverage by age and time since vaccine administration (and in the future) and the number of doses received is limited
- Additional risk factors (e.g., comorbidities) are not available for identified cases of IPD and VT IPD, which limits extensions of findings to high-risk groups due to underlying health conditions
- Missing data was present within both the CNDSS and NML datasets.
- Enhanced surveillance that includes high risk individuals and can provide incidence of IPD stratified by risk factors and serotypes for individuals in the greater than 65-year age group.
- Epidemiological studies of non-invasive disease such as CAP or acute otitis media in children caused by S. pneumoniae.
XI. Characteristics of included studies
| Study | Comparisons | Study Design | Participants |
|---|---|---|---|
| PNEU-C-15 studies | |||
Ermlich et al., Vaccine, 2018;36 (45): 6875-6882. V114-002 Multicenter: 25 sites from across Canada, Denmark, Israel, Norway, Poland, Spain, Sweden, United States. Study period: March 2012-February 2013 Funder: Merck |
|
Phase 2. Randomized to PNEU-C-15 (N=230),
PNEU-P-23 (N=231), or PNEU-C-13 (N=230) |
Community-dwelling adults aged ≥50 years who are vaccine-naïve Gender (total study): 53% female Ethnicity (total study): 93% non-Hispanic or non-Latino Race (total study): 93% White Age (total study):
Authors state participants were similar across groups for distribution of age, gender, race/ethnicity, key pre-existing medical conditions (chronic heart disease, COPD, diabetes mellitus), and prior and concomitant treatment. |
Song et al., Vaccine, 2021;39 (43): 6422-6436. Study period: June 2018-December 2016 Funding: Merck Sharp & Dohme Corp. |
Vaccine series at 12-month interval |
Phase 3, Randomized to single dose of PNEU-C-15 (N=327) or PNEU-C-13 (N=325) at Day 1 followed by single dose PNEU-P-23 (both arms) at month 12 Total randomized = 652 |
Adults aged ≥50 years, in good health and/or with stable underlying medical conditions, without a history of invasive pneumococcal disease, and who are vaccine-naïve. Gender (total study): 56.8% female Ethnicity (total study): 87.4% non-Hispanic or non-Latino Race (total study): 61.6% White Median age: 65.0 years Age (total study):
Authors state participants were similar across groups for distribution of variables including age, sex, race, and ethnicity. |
Platt et al., Vaccine, 2022;40 (1): 162-172 V114-019 Multicenter: 30 sites from across Canada, United States, Japan, Spain, Taiwan. Study period: June 2019-March 2020 Funding: Merck Sharp & Dohme Corp. |
|
Phase 3, Randomized to single dose of PNEU-C-15 (N=604) or PNEU-C-13 (601) Total randomized = 1205 |
Adults aged ≥50 years, in good health and/or with stable underlying medical conditions, without a history of invasive pneumococcal disease, and who are vaccine-naïve Gender (total study): 57.3% female Ethnicity (total study): 78.0% non-Hispanic or non-Latino Race (total study): 67.7% White Median age: 66.0 years Age (total study):
Authors state participant demographics were similar between groups. |
Peterson et al., Human vaccines & immunotherapeutics, 2019;15 (3): 540-548. V114-007 Multicenter: 17 sites in United States Study period: November 2015-January 2016 Funder: Merck |
|
Phase 2. Randomized to PNEU-C-15 (N=127) or PNEU-C-13 (N=126) Total randomized = 253 Randomization was stratified according to age and time since vaccination (groupings as shown in adjacent column). |
Adults aged ≥65 years, with a history of prior PNEU-P-23 vaccination at least one year prior to study entry Gender (whole study): 59.7% female Median Age (whole study): 72.0 years Age distribution: 65-74 years, 70%; ≥75 years, 30% Race (whole study): 94.1% White Ethnicity (whole study): 84.6% non-Hispanic or non-Latino Time since PNEU-P-23 vaccination: 1-3 years, 32.4%; >3 years, 67.6% Authors state groups were similar for gender, age, ethnicity/race, pre-existing conditions, prior therapy, and time interval since PNEU-P-23 vaccination. |
Hammitt et al., Open forum infectious diseases, 2022;9 (3): ofab605 Study period: July 2018 to July 2020 Funder: Merck |
Vaccine series at 6-month interval |
Total randomized: 1515. |
Adults aged 18-49 years who are immunocompetent and are with or without risk factor(s) for pneumococcal disease Gender (total study): 52% female Ethnicity (total study): 87% non-Hispanic or non-Latino Race (total study): 51% White, 39% Indigenous (US. 39% of participants were from US Center for American Indian Health (CAIH) sites. Mean age: 36.0 years No risk factors: 25% Risk factors included: chronic lung disease including asthma, tobacco use, diabetes mellitus, chronic liver disease, chronic heart disease, and alcohol consumption. All subjects with no risk factor and subjects with single risk factor of alcohol consumption were enrolled at CAIH sites. Authors state that demographic and baseline characteristics were similar between groups. |
Mohapi et al., AIDS (London, England), 2022;36 (3): 373-382 Study period: July 2018-January 2020 Funder: Merck |
|
Randomization stratified by CD4+ cell count, with intent of ≥50% participants enrolled in the middle stratum: ≥50 to <200; ≥200 to <500, and ≥500 cells/μL |
Adults aged >=18 years who have HIV (CD4+ ≥50 cells/μL and plasma HIV RNA <50,000 copies/mL), are vaccine-naïve, and no IPD or culture-positive pneumococcal disease within prior 3 years. Gender (total study): 21% female Ethnicity (total study): 68% non-Hispanic or non-Latino Race (total study): 31% Black, 30% White, 21% more than one race, 18% Asian Median age: 41y. Of the total study, 72% were 18-49y. Few participants (3.6%) were ≥65y. By CD4+ T-cell count (cells/µL):
Authors state groups were similar for demographic and baseline characteristics. |
Severance et al. Human Vaccines & Immunotherapeutics, 2022; 18 (1); e1976581 V114-021 Multicenter: 45 sites in United States Study period: September 24, 2018-June 24, 2019 Funding: Merck Sharp & Dohme Corp. |
PNEU-C-15+QIV, with placebo on day 30 (concurrent) Vs QIV + placebo, with PNEU-C-15 on day 30 (non-concomitant) |
Phase 3, randomized to concomitant (N=600) or non-concomitant (N=600) groups. Total randomized = 1200 Randomization was 1:1 but stratified according to age (50-64y, 65-74y, ≥75y) and history of PNEU-P-23 vaccination. |
Adults aged ≥50 years, in good health and/or stable underlying medical conditions and without a history of invasive or other pneumococcal disease. Prior vaccination of PNEU-P-23 eligible if received >12 months before first study visit but designed to have at least 50% of participants vaccine-naive. Gender (total study): 56.1% female Ethnicity (total study): 78.8% non-Hispanic or non-Latino Race (total study): 82.5% White Median age: 65.0 years Age (total study):
Prior vaccination with PNEU-P-23: 20.9% Authors state that groups were similar for baseline characteristics, including age, sex, race, ethnicity, underlying medical conditions, and prior vaccination with PNEU-P-23. |
| PNEU-C-20 studies | |||
Hurley et al., Clinical Infectious Diseases, 2021; 73 (7): e1489-1497 Funding: Pfizer Inc. |
Series delivered |
Phase 2, Randomized to single dose of PNEU-C-20 (N=222) or PNEU-C-13 (N=222) followed by single dose saline (PNEU-C-20 arm) or PNEU-P-23 (PNEU-C-13 arm) one month after first vaccination |
Adults aged 60-64 years, generally healthy (including those with stable underlying medical conditions), without a history of laboratory-confirmed invasive pneumococcal disease, and vaccine-naïve. Ethnicity (total study): 87.4% non-Hispanic or non-Latino Race: 75.4% White Median age: 62.0 years Authors state participant demographics were similar between groups. |
Essink et al., Pivotal Phase 3 Randomized Clinical Trial of the Safety, Tolerability, and Immunogenicity of 20-valent Pneumococcal Conjugate Vaccine in Adults Aged ≥18 Years, Clinical Infectious Diseases, 2022; ciab990. Online ahead of print. Funding: Pfizer Inc. |
Adults ≥60 years: PNEU-C-13 followed by |
Phase 3, Randomization stratified by age subgroup: Participants ≥60 years of age were randomized to single dose of PNEU-C-20 (N=1514) or PNEU-C-13 (N=1495) followed by single dose saline (PNEU-C-20 arm) or PNEU-P-23 (PNEU-C-13 arm) one month after first vaccination. Participants 50-59 years randomized to single dose PNEU-C-20 (N=334) or PNEU-C-13 (N=111). Participants 18-49 years randomized to single dose PNEU-C-20 (N=336) or PNEU-C-13 (N=112).
|
Adults aged ≥18 years without a serious chronic disorder or other acute or chronic medical or psychiatric condition, without a history of laboratory-confirmed invasive pneumococcal disease, and vaccine-naïve.
Ethnicity, % non-Hispanic or non-Latino (by age cohort):
Race, % White (by age cohort):
Age (≥60 year cohort):
Authors state participant demographics were similar between intervention groups for each of the age-specific cohorts. |
Cannon et al., Vaccine, 2021: 39 (51):7494-7502. Multicenter: 33 sites in United States and 8 sites in Sweden. Study period: February 2019-February 2020 Funding: Pfizer Inc. |
Comparison dependent on cohort:
|
Phase 3. Randomized 2:1: PNEU-P-23+ PNEU-C-20 (N=253) vs PNEU-P-23+ PNEU-C-13 (N=122) PNEU-C-13+ PNEU-C-20 (N=248) vs PNEU-C-13+ PNEU-P-23 (N=127) Total randomized as relevant to this review: 750. |
Adults aged ≥65 years with prior vaccination to PNEU-P-23 or PNEU-C-13. Participants with stable underlying medical conditions and without prior S. pneumoniae infection were eligible. A third cohort with prior vaccination to both PNEU-P-23 and PNEU-C-13 was not in this review as it was not a randomized comparison.
Authors state that demographic characteristics were similar among groups. |
List of Abbreviations
- AE
- Adverse event
- CAPiTA
- Community-Acquired Pneumonia immunization Trial in Adults
- CAP
- Community-acquired pneumonia
- CI
- Confidence Interval
- CIRN
- Canadian Immunization Research Network
- CMC
- Chronic Medical Condition
- CNDSS
- Canadian Notifiable Disease Surveillance System
- CRM197
- Corynebacterium diphtheriae
- CSF
- Chronic cerebrospinal fluid
- DALY
- Disability adjusted life years
- EEFA
- Ethics, equity, feasibility, acceptability
- EtD
- Evidence to Decision
- GRADE
- Grading of Recommendations, Assessment, Development and Evaluation
- HIV
- Human Immunodeficiency Virus
- HSCT
- Hematopoietic Stem Cell Transplant
- IC
- Immunocompromising conditions
- ICD
- International Classification of Diseases
- ICER
- Incremental cost-effective ratio
- ICS
- International Circumpolar Surveillance
- IM
- Intramuscularly
- IPD
- Invasive pneumococcal disease
- GMT
- Geometric mean titre
- GMFR
- Geometric mean fold rises
- LLOQ
- Lower limit of quantitation
- LSPQ
- Laboratoire de santé publique du Québec
- LTCF
- Long term care facility
- NACI
- National Advisory Committee on Immunization
- NDCMC
- Newly diagnosed chronic medical conditions
- NML
- National Microbiology Laboratory
- NOC
- Notice of compliance
- NVT
- Non-vaccine type
- NWT
- Northwest Territories
- OPA
- Opsonophagocytic Activity
- OR
- Odds ratio
- pCAP
- Pneumococcal community-acquired pneumonia
- PD
- Pneumococcal disease
- Pop
- Population
- PP
- Pneumococcal pneumonia
- P-Y
- Population per year
- PHAC
- Public Health Agency of Canada
- PNEU-C
- Pneumococcal conjugate vaccine
- PNEU-C-15 (Vaxneuvance)
- 15-valent pneumococcal conjugate vaccine
- PNEU-C-20 (PREVNAR20)
- 20-valent pneumococcal conjugate vaccine
- PNEU-C-13 (PREVNAR13)
- 13-valent pneumococcal conjugate vaccine
- PNEU-P
- Pneumococcal polysaccharide vaccine
- PNEU-P-23
- 23-valent pneumococcal polysaccharide vaccine
- PWG
- Pneumococcal Working Group
- QALY
- Quality adjusted life-years
- QIV
- Quadrivalent inactivated influenza vaccine
- RCT
- Randomized controlled trial
- RoB
- Risk of bias
- SAE
- Serious adverse events
- SOS
- Serious Outcome Surveillance
- SSE
- Solicited systemic events
- ST3
- Serotype 3
- TIBDN
- Toronto Invasive Bacterial Diseases Network
- UAD
- Urine antigen detection
- US
- United States
- VT
- Vaccine type
Acknowledgments
This statement was prepared by: K Hildebrand, A Nam, R Pless, A Stevens, A Tuite, A Wierzbowski, and E Wong on behalf of the NACI Pneumococcal Working Group and was approved by NACI.
NACI gratefully acknowledges the contribution of M Hersi, N Islam, CY Jeong, A Li, R MacTavish, A Golden, W Demczuk, A Griffith, I Martin, E Tarrataca, C Tremblay, M Tunis, MW Yeung, K Young, and R Ximenes.
NACI Pneumococcal Working Group
Members: K Hildebrand (Chair), J Bettinger, N Brousseau, P De Wals, D Fisman, J Kellner, A McGeer, J Papenburg, S Rechner, and G Tyrell
Ex-officio representatives: G Coleman (Biologic and Radiopharmaceutical Drugs Directorate [BRDD] Health Canada [HC]), M Kobayashi (Centre for Disease Control [CDC] United States), A Li (Vaccine Preventable Diseases Surveillance [VPDS] PHAC), I Martin (National Microbiology Lab [NML] PHAC), G Metz (Vaccine Safety [VS] PHAC), and A Monohan (First Nations and Inuit Health Branch [FNIHB], Indigenous Services Canada [ISC])
PHAC Participants: A Wierzbowski (Technical lead), R Pless (Medical lead), N Islam, A Y Li, I Martin, A Stevens, C Tremblay, A Tuite, and K Young
NACI
NACI members: S Deeks (Chair), R Harrison (Vice-Chair), M Andrew, J Bettinger, N Brousseau, H Decaluwe, P De Wals, E Dubé, V Dubey, K Hildebrand, K Klein, M O’Driscoll, J Papenburg, A Pham-Huy, B Sander, and S Wilson.
Former NACI members: S Smith
Liaison representatives: L Bill / M Nowgesic (Canadian Indigenous Nurses Association), LM Bucci (Canadian Public Health Association), E Castillo (Society of Obstetricians and Gynaecologists of Canada), J Comeau (Association of Medical Microbiology and Infectious Disease Canada), J MacNeil (Centers for Disease Control and Prevention, United States), L Dupuis (Canadian Nurses Association), M Osmack (Indigenous Physicians Association of Canada), J Potter (College of Family Physicians of Canada), M Lavoie (Council of Chief Medical Officers of Health), D Moore (Canadian Paediatric Society), M Naus (Canadian Immunization Committee), and A Ung (Canadian Pharmacists Association).
Former liaison representatives: L Dupuis (Canadian Nurses Association), D Fell (Canadian Association for Immunization Research and Evaluation), J Hu (College of Family Physicians of Canada)
Ex-officio representatives: V Beswick-Escanlar (National Defence and the Canadian Armed Forces), E Henry (Centre for Immunization and Respiratory Infectious Diseases (CIRID), PHAC), M Lacroix (Public Health Ethics Consultative Group, PHAC), C Pham (Biologic and Radiopharmaceutical Drugs Directorate, Health Canada), D MacDonald (COVID-19 Epidemiology and Surveillance, PHAC), S Ogunnaike-Cooke (CIRID, PHAC), P Fandja (Marketed Health Products Directorate, HC), M Routledge (National Microbiology Laboratory, PHAC), and T Wong (First Nations and Inuit Health Branch, Indigenous Services Canada).
Former ex-officio representatives: C Lourenco (Biologic and Radiopharmaceutical Drugs Directorate, Health Canada), K Robinson (Marketed Health Products Directorate, HC)
Appendix A: Tables
| GRADE rating | Description |
|---|---|
| High | Very confident that the true effect lies close to that of the effect estimate. |
| Moderate | Moderately confident: the true effect is likely to be close to the effect, but there is a possibility that it is substantially different. |
| Low | Limited confidence: the true effect may be substantially different from the effect estimate. |
| Very Low | Very little confidence: true effect likely to be substantially different from the effect estimate. |
| Outcome | Definition |
|---|---|
| Clinical outcomes: Benefits | |
| All Invasive Pneumococcal Disease (IPD) | Clinical evidence of pneumonia with bacteremia, bacteremia without a known site of infection, and/or meningitis with laboratory confirmation of infection and isolation of Streptococcus pneumoniae or its DNA from a normally sterile site. |
| Vaccine-type Invasive Pneumococcal Disease (VT IPD) | Clinical evidence of invasive disease (pneumonia with bacteremia, bacteremia without a known site of infection, and/or meningitis) with laboratory confirmation of infection and isolation of Streptococcus pneumoniae or its DNA from a normally sterile site confirmed by serotyping as S. pneumoniae serotype 4, 9V, 6B, 14, 18C, 19F, 23F, 1, 5, 7F, 3, 6A, 19A, 2, 8, 9N, 10A, 11A, 12F, 15B, 17F, 20, 22F, or 33F. |
| All Community-Acquired Pneumonia | Community acquired pneumonia is defined if a presentation occurred within 72 hours of hospital admission with a new or evolving pulmonary infiltrate on chest radiograph suggestive of pneumonia, with ≥2 signs or symptoms (temperature >38°C, cough, sputum production, shortness of breath, pleuritic chest pain, crackles, or consolidation on chest examination) |
| pneumococcal Community Acquired Pneumonia (pCAP) | A pCAP is a CAP case which has a confirmation of S. pneumoniae from urine antigen detection or isolation of S. pneumoniae from blood or sputum culture. |
| pCAP due to vaccine preventable serotype | Laboratory confirmation of infection and isolation of Streptococcus pneumoniae or its DNA from a non-sterile site (sputum) confirmed by serotyping as S. pneumoniae serotype 4, 9V, 6B, 14, 18C, 19F, 23F, 1, 5, 7F, 3, 6A, 19A, 2, 8, 9N, 10A, 11A, 12F, 15B, 17F, 20, 22F, or 33F. |
| Death due to vaccine preventable serotype | Death caused as a result of S. pneumoniae infection which was laboratory confirmed to be as S. pneumoniae serotype 4, 9V, 6B, 14, 18C, 19F, 23F, 1, 5, 7F, 3, 6A, 19A, 2, 8, 9N, 10A, 11A, 12F, 15B, 17F, 20, 22F, or 33F. |
| All-cause death | Death due to any cause. |
| Immunogenicity outcomes - Benefits | |
| Determined by opsonophagocytic activity (OPA) | OPA represents functional antibodies capable of opsonizing pneumococcal capsular polysaccharides for presentation to phagocytic cells for engulfment and subsequent killing and is considered an important immunologic surrogate measure of protection against pneumococcal disease. |
| Immune responses |
Assessed by serotype-specific OPA assay and OPA geometric mean titers (GMTs) after vaccination. It can also be measured as geometric mean fold rises (GMFRs) of serotype-specific OPA titers from before to after vaccination, percentage of participants with a >4-fold rise in OPA titers from before to after vaccination, and percentage of participants with OPA titers greater than or equal to the lower limit of quantitation (LLOQ) after vaccination. Percentage of participants with a >4-fold rise (seroresponders) in serotype-specific pneumococcal OPA titers from before vaccination to after vaccination along with corresponding 2-sided 95% CIs are calculated. |
| Non-inferiority |
Defined based on the lower bound of the 2-sided 95% CI of the OPA GMT ratio between intervention and comparator to be greater than 0.5 at a pre-determined time (e.g.,30 days) post-vaccination. Based on the between-group comparisons of OPA GMTs and proportions of participants with a ≥4-fold rise in serotype-specific OPA titers from pre-vaccination to post-vaccination. |
| Superiority | Conclusion of superiority for serotype 3 is based on the lower bound of the 95% CI for the estimated GMT ratio (intervention/comparator) being > 1.2. Conclusion of superiority for the unique serotypes is based on the lower bound of the 95% CI for the estimated GMT ratio (comparator/intervention) being > 2.0. |
| Clinical outcomes - Harms | |
| Local adverse reactions |
Solicited reactions of redness, swelling, pain at the site of injection site monitored for a specified (7-10 days) period following the vaccination. |
| Redness | Redness and swelling defined as mild (greater than [>] e.g.,2.0 to 5.0 cm), moderate (>5.0 to 10.0 cm) and severe (>10.0 cm). |
| Pain | Pain at injection site was graded as mild (did not interfere with activity), moderate (interfered with activity), and severe (prevented daily activity). |
| Local systematic reaction | Solicited reactions of fatigue, headache, muscle pain, join paint, or fever monitored for a specific period of time (e.g.,7 days) post-vaccination. Fever was defined as greater than or equal to (>) 38.0 degree Celsius (C) and categorized to >38.0 to 38.4 degree C, >38.4 to 38.9 degree C, >38.9 to 40.0 degree C and >40.0 degree C. Fatigue, headache, muscle pain and joint pain were graded as mild (did not interfere with activity), moderate (some interference with activity) and severe (prevented daily routine activity). |
| Serious adverse events (SAE) within 6 months after vaccination | An SAE is defined as any untoward medical occurrence that results in death; is life-threatening (immediate risk of death); requires inpatient hospitalization or prolongation of existing hospitalization; results in persistent or significant disability/incapacity (substantial disruption in the ability to conduct normal life functions); results in congenital anomaly/birth defect or that is considered to be an important medical event. |
| Newly Diagnosed Chronic Medical Conditions (NDCMCs) within 6 months after vaccination | Newly Diagnosed Chronic Medical Conditions (NDCMCs) defined as a disease or medical conditions, not previously identified, that are expected to be persistent or was otherwise long lasting in their effects. |
| Study | Risk of Bias Domains Table 8 Footnote a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RSG | AC | B-PP | B-OA | MOD | BI | SR | ||||
| Immunogenicity | AE | Immunogenicity | AE | |||||||
PNEU-C-15 studies |
||||||||||
| Ermlich 2018 | L | L | L | L | L | L | L | L | L | |
| Song 2021 | L | L | L | L | L | L | L | L | L | |
| Platt 2022 | L | L | L | L | L | L | L Table 8 Footnote b | S Table 8 Footnote b | L | L |
| Peterson 2018 | L | L | L | L | L | L | L | L | L | |
| Hammitt 2022 | L | L | L | L | L | L | L | L | L | |
| Mohapi 2022 | L | L | L | L | L | L | L | L | L | |
| Severance 2022 | L | L | L | L | L | L | L | L | L | |
| PNEU-C-20 studies | ||||||||||
| Hurley 2021 | L | L | L | L | L | L | L | L | L | |
| Essink 2022 | L | L | L | L | L | L | L | L | L | |
| Cannon 2021 | L | L | L | n/a | H | L | L | L | L | |
Abbreviations: AE = adverse events; L = low risk of bias; H = high risk of bias; n/a = not applicable; S=some concerns or unclear.
|
||||||||||
Evidence synthesis tables
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating (Table 1) |
|---|---|---|---|
Geometric Mean Titers (per protocol) 1 month after vaccine |
1 RCT (Platt 2022); PNEU-C-15: Range N=594-598 analysed across serotypes PNEU-C-13: Range N=586-598 analysed across serotypes |
Shared serotypes All except ST3: GMT ratio estimate ranged 0.68 (ST4) to 1.23 (ST6B). ST3: 1.60. Non-inferiority for PNEU-C-15 met for all shared serotypes (margin >0.5; lowest CI bound across serotypes 0.57 [ST4]). Additional data (not GRADEd): Unique serotypes, 22F, 33F. GMT ratio estimates 31.83 and 7.11, respectively. Numerically higher responses for the unique serotypes. Two additional studies in adults ≥50 years provided immunogenicity information (combined n>500 by serotype analysis). One study used a non-inferiority threshold calculated for another comparison, while the other did not evaluate for non-inferiority. For both studies, most serotypes showed numerically higher GMT ratio point estimates and differed in which serotypes showed numerically lower point estimates (ST4 and 7F in one study; 19F in the other study). Subgroups for age (50 to 64y vs ≥65y). No studies evaluated non-inferiority according to a 50 to 64y population. One study (V114-019; Platt 2022) provided sufficient information to evaluate overlap visually between 50 to 64y and ≥65y. There was substantive overlap for most shared serotypes. Serotypes 5, 14, and 23F had apparent higher numerical estimates, especially ST14. Overlapping but with a higher apparent estimate in the ≥65 y group was observed for ST3 when compared with the 50 to 64y group. There was substantive overlap with 22F and 33F. In general, there was congruency between subgroup across serotypes. Subgroups for age (65-74y vs ≥75y). No studies evaluated non-inferiority according to a ≥75y population. One study (V114-019; Platt 2022) provided sufficient information to evaluate overlap visually between 65-74y and ≥75y. There was substantive overlap for most shared serotypes. Serotype19A had a higher apparent numerical estimate and especially that for 6B. For serotype18C, there was no overlap with PNEU-C-15 showing higher values. Substantive overlap in age groups for ST3 and the unique serotypes 22F and 33F. In general, there was congruency between subgroup across serotypes. |
Moderate Table 9 Footnote a PNEU-C-15 is probably not inferior to PNEU-C-13 in immune response for shared serotypes. |
% Seroresponders 1 month after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: Range N=1031-1108 analysed across serotypes PNEU-C-13: Range N=1044-1110 analysed across serotypes |
Shared serotypes except ST3. Mixed results among studies. In the largest study (N~1100), almost two-thirds of serotypes showed a numerically lower proportion of seroresponders with PNEU-C-15 than PNEU-C-13. In the remaining studies (combined N~900-1000), most serotypes showed a greater numerical proportion of seroresponders with PNEU-C-15. ST6B, 18C, and 23F show numerically higher seroresponders across studies. No one serotype was consistently showing a lower seroresponse with PNEU-C-15 in all three studies. Additional data (not GRADEd): Age subgroups (50 to 64y vs ≥65y). One study (V114-002; Ermlich 2018) provided information by subgroup (50 to 64y, 65-74y, ≥75y), but is based on small sample sizes (range 132-144 analyzed across subgroups). Mixed results across serotypes. Serotypes 1, 3, and 9V show a higher numerical point estimate with PNEU-C-15 for all subgroups; a lower numerical point estimate was observed across the subgroups for serotypes 6A, 7F, and 19F. For serotype 5, the 50 to 64y and 65-74y both show a higher numerical point estimate. For serotype 6B, the 50 to 64y subgroup shows a lower numerical point estimate, in contrast to the other two subgroups. For serotypes 14, 18C, and 19A, only the 65-74y subgroup shows a higher numerical point estimate with PNEU-C-15. Age subgroups (65-74y vs ≥75y). One study (V114-002; Ermlich 2018) provided information by subgroup (65-74y, ≥75y), but are based on small sample sizes (range 132-144 analyzed across subgroups). Similar results are observed for most serotypes. Conversely to the 65-74y age group, the ≥75y subgroup is showing fewer numerical seroresponders with PNEU-C-15 for serotypes 5, 14, 18C, 19A, and 23F. Both age groups are showing more numerical seroresponders with PNEU-C-15 for ST3 and fewer with 6A. |
Low Table 9 Footnote b Table 9 Footnote c There may be variability across shared serotypes (except ST3) as to whether a numerically higher proportion of seroresponders is observed with PNEU-C-15. |
% Seroresponders 1 month after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: Range N=1095 analysed PNEU-C-13: Range N=1099 analysed |
Shared serotype, ST3. Higher numerical seroresponse estimate with PNEU-C-15 (RR range 1.13 to 1.41; RD range 9.9% to 21%). |
Moderate Table 9 Footnote c Table 9 Footnote d There is probably a higher numerical proportion of seroresponders with PNEU-C-15 for ST3. |
% Seroresponders 1 month after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: Range N 982 to 1093 analysed PNEU-C-13: Range N 944 to 1068 analysed |
Unique serotypes. Numerically higher proportion of seroresponders with PNEU-C-15. 22F: RR range 4.41 to 6.47; RD range 56.3% to 64.6%. 33F: RR 6.61 to 20.43; RD 50.4% to 58.3%.
Age subgroups (50 to 64y vs ≥65y). Higher numerical point estimates are observed for serotypes 22F and 33F across subgroups (range 125-137 analyzed across subgroups). Age subgroups (65-74y vs ≥75y). Higher numerical point estimates are observed for serotypes 22F and 33F across subgroups (range 125-137 analyzed across subgroups). |
Moderate Table 9 Footnote c Table 9 Footnote d There is probably a higher numerical proportion of seroresponders with PNEU-C-15 with serotypes 22F and 33F. |
Vaccine-related Serious AE Up to 6 months after vaccine |
2 RCTs (Platt 2022, Ermlich 2018) PNEU-C-15: 0/645 PNEU-C-13: 0/644 |
No vaccine-related SAE observed in either group. |
Moderate Table 9 Footnote c Table 9 Footnote e |
Serious AE Up to 6 months after vaccine |
2 RCTs (Platt 2022, Ermlich 2018) PNEU-C-15: 13/645 PNEU-C-13: 13/644 |
Relative effects: Peto OR 1.00 (0.46 to 2.17) Absolute effects: 0 fewer per 1,000 (11 fewer to 23 more) SAEs reported in Ermlich 2018. PNEU-C-15: coronary artery occlusion, appendicitis, anal cancer, anxiety. PNEU-P-23: cardiac failure, myocardial infarction, vertigo, gastrointestinal disorder, death, appendicitis, benign urinary tract neoplasm. The second study not providing a list of SAEs indicated that no deaths occurred during the study period. |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of SAEs up to 6 months after vaccine administration. None of those events were deemed to be vaccine-related by study authors. |
Severe Systemic AE - Fatigue Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 6/1158 PNEU-C-13: 7/1154 |
Relative effects: Peto OR 0.86 (0.29 to 2.55) Absolute effects: 1 fewer per 1,000 (4 fewer to 9 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe fatigue within 14 days after vaccine administration. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 6/1158 PNEU-C-13: 7/1154 |
Relative effects: Peto OR 0.86 (0.29 to 2.55) Absolute effects: 1 fewer per 1,000 (4 fewer to 9 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe headache within 14 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 3/1158 PNEU-C-13: 8/1154 |
Relative effects: Peto OR 0.40 (0.12 to 1.31) Absolute effects: 4 fewer per 1,000 (6 fewer to 2 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe muscle pain within 14 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 2/1158 PNEU-C-13: 2/1154 |
Relative effects: Peto OR 1.00 (0.14 to 7.13) Absolute effects: 0 fewer per 1,000 (1 fewer to 10 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe joint pain within 14 days after vaccine administration. |
Severe Systemic AE - Fever Up to 5 days after vaccine |
2 RCTs (Platt 2022, Song 2021) PNEU-C-15: 3/925 (0.3%) PNEU-C-13: 2/921 (0.2%) |
Relative effects: Peto OR 1.49 (0.26 to 8.60) Absolute effects: 1 more per 1,000 (2 fewer to 16 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe fever within 5 days after vaccine administration. |
Mild/Moderate Systemic AE - Fatigue Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 232/1158 PNEU-C-13: 197/1154 |
Relative effects: RR 1.20 (0.89 to 1.63) Absolute effects: 34 more per 1,000 (19 fewer to 108 more |
Moderate Table 9 Footnote c Table 9 Footnote f There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate fatigue within 14 days after vaccine administration. |
Mild/Moderate Systemic AE - Headache Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 151/1158 PNEU-C-13: 140/1154 |
Relative effects: RR 1.11 (0.83 to 1.48) Absolute effects: 13 more per 1,000 (21 fewer to 58 more) |
Low Table 9 Footnote c Table 9 Footnote g There may be little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate headache within 14 days after vaccine administration. |
Mild/Moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 215/1158 PNEU-C-13: 150/1154 |
Relative effects: RR 1.43 (1.18 to 1.73) Absolute effects: 56 more per 1,000 (23 more to 95 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably a trivial difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate muscle pain within 14 days after vaccine administration. |
Mild/Moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
3 RCTs (Platt 2022, Ermlich 2018, Song 2021) PNEU-C-15: 90/1158 PNEU-C-13: 90/1154 |
Relative effects: RR 1.00 (0.76 to 1.31) Absolute effects: 0 fewer per 1,000 (19 fewer to 24 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate joint pain within 14 days after vaccine administration. |
Mild/Moderate Systemic AE - Fever Up to 5 days after vaccine |
2 RCTs (Platt 2022, Song 2021) PNEU-C-15: 4/925 PNEU-C-13: 10/923 |
Relative effects: Peto OR 0.42 (0.15 to 1.20) Absolute effects: 6 fewer per 1,000 (9 fewer to 2 more) |
Moderate Table 9 Footnote c Table 9 Footnote e There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate fever within 5 days after vaccine administration. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; SAE= serious adverse events; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15 vs PNEU-P-23. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers 1 month after vaccine |
1 RCT (Ermlich 2018);
|
Shared serotypes All except ST3: GMT ratio estimate ranged 0.77 (19F) to 5.64 (ST23F). ST3: 1.96. Non-inferiority for PNEU-C-15 met for all 14 shared serotypes (margin ≥0.33; lowest CI bound across serotypes 0.55 [19F]). Additional data (not GRADEd): Unique serotype, 6A. GMT ratio estimate 8.59. Numerically higher response for the unique serotype. Subgroups by Age. GMT Ratios. Non-inferiority for the age 65-74y (n=65-67) and ≥75y age (n=70-72) groups were not available. Across serotypes, most GMT ratios >1 except 19F (both age groups). For ST3, GMT Ratios were 2.68 and 1.44, respectively. For ST6A, GMT ratios were 9.61 and 8.67, respectively. |
Low Table 10 Footnote a Table 10 Footnote b PNEU-C-15 may be non-inferior to PNEU-P-23 in immune response for shared serotypes. |
% Seroresponders (≥4-fold risk in risk in serotype specific OPA) |
|
Shared serotypes: Unique serotype, 6A: RR 1.36, RD 21.6%. Numerically higher proportion of seroresponders with most serotypes, favouring PNEU-C-15. Additional data (not GRADEd): Across serotypes, most show a higher numerical proportion of seroresponders with PNEU-C-15 in the 65-74y (RR 0.94 to 1.31; RD -4.61% to 18.46%) and ≥75y (RR 0.83 to 1.37; RD -12.02% to 21.86%) age groups, with variation in exceptions between age groups. ST6A values were the highest in those groups (RR 1.25 and RD 16.48; RR 1.51 and RD 26.06, respectively. |
Low Table 10 Footnote a Table 10 Footnote b PNEU-C-15 may result in a numerically higher proportion of seroresponders for most serotypes compared with PNEU-P-23. |
Vaccine-related Serious AE Up to 6 months after vaccine |
1 RCT (Ermlich 2018);
|
No vaccine related serious AE observed in either group. |
Moderate Table 10 Footnote b Table 10 Footnote c |
SAE |
1 RCT (Ermlich 2018);
|
Relative effects: Peto OR 0.58 (0.17 to 1.90) Absolute effects: 13 fewer per 1,000 (from 25 fewer to 26 more)
|
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in SAEs between PNEU-C-15 and PNEU-P-23. None were vaccine related. |
Severe Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: Peto OR 0.51 (0.10 to 2.56) Absolute effects: 8 fewer per 1,000 (from 16 fewer to 26 more) |
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in severe fatigue between PNEU-C-15 and PNEU-P-23. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: Peto OR 2.75 (0.38 to 19.64) Absolute effects: 8 more per 1,000 (3 fewer to 75 more) |
Moderate Table 10 Footnote b Table 10 Footnote d |
Severe Systemic AE - Muscle pain Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: Peto OR 0.51 (0.14 to 0.90) Absolute effects: 13 fewer per 1,000 (22 fewer to 22 more) |
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in severe muscle pain between PNEU-C-15 and PNEU-P-23. |
Severe Systemic AE - Joint pain Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: Peto OR 0.37 (0.05 to 2.62) Absolute effects: 8 fewer per 1,000 (12 fewer to 20 more) |
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in severe joint pain between PNEU-C-15 and PNEU-P-23. |
Severe Systemic AE – Fever Up to 14 days after vaccine |
Not reported by severity |
||
Mild/moderate Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: RR 0.92 (0.67 to 1.27) Absolute effects: 21 fewer per 1,000 (85 fewer to 69 more) |
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in mild/moderate fatigue between PNEU-C-15 and PNEU-P-23. |
Mild/moderate Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: RR 1.53 (0.95 to 2.44) Absolute effects: 58 more per 1,000 (5 fewer to 157 more) |
Moderate Table 10 Footnote b Table 10 Footnote d There is probably little to no difference in mild/moderate headache between PNEU-C-15 and PNEU-P-23. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: RR 1.19 (0.87 to 1.63) Absolute effects: 45 more per 1,000 (31 fewer to 148 more) |
Moderate Table 10 Footnote b Table 10 Footnote d There is probably little to no difference in mild/moderate muscle pain between PNEU-C-15 and PNEU-P-23. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Ermlich 2018);
|
Relative effects: RR 1.00 (0.67 to 1.51) Absolute effects: 0 fewer per 1,000 (55 fewer to 84 more) |
Moderate Table 10 Footnote b Table 10 Footnote c There is probably little to no difference in mild/moderate joint pain between PNEU-C-15 and PNEU-P-23. |
Mild/moderate Systemic AE – Fever Up to 14 days after vaccine |
Not reported by severity |
||
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RCT = randomized controlled trial; RD = risk difference; RR = relative risk; SAE = Serious adverse events; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15+QIV concomitantly vs PNEU-C-15+QIV non-concomitantly. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers (per protocol) 1 month after vaccine |
1 RCT (Severance 2022);
|
All except ST3: GMT ratio estimate ranged from 0.66 (ST1) to 1.02 (ST19F). ST3: 0.94. Non-inferiority for PNEU-C-15 administered concomitantly with QIV met for all 15 serotypes (margin >0.5; lowest CI bound across serotypes 0.54 [ST1]). Additional data (not GRADEd): Influenza strains. QIV administered concomitantly with PNEU-C-15 was not inferior to non-concomitant administration for all four influenza strains (margin >0.5; lowest CI bound across strains 0.86 [B-Victoria]). Subgroup by age. One study (Severance 2022) reported GMT ratios for 50 to 64, 65-74, and ≥75 year olds. Across subgroups, serotype-specific GMT OPAs tended to be higher for the younger age group (50 to 64 years) compared to the older age groups, however, there was substantive overlap in the GMT ratio confidence intervals. Subgroup by PNEU-P- vaccination history. The study also performed subgroup analysis by history of PNEU-P-23 vaccination and reported generally similar ratios as compared to the overall study population. |
Moderate Table 11 Footnote a PNEU-C-15 administered concomitantly with QIV is probably not inferior to PNEU-C-15 administered non-concomitantly with QIV. |
% Seroresponders 1 month after vaccine |
1 RCT (Severance 2022);
|
Serotypes except ST3. Numerically lower proportion of seroresponders with concomitant administration compared to non-concomitant administration for all shared serotypes except serotypes 7F, 9V, 19F, and 23F. Subgroup data by age and PNEU-P-23 vaccination history not provided. |
Moderate Table 11 Footnote a PNEU-C-15 administered with QIV probably results in a numerically lower proportion of seroresponders for most serotypes compared with PNEU-C-15 administered non-concomitantly with QIV. |
% Seroresponders 1 month after vaccine |
1 RCT (Severance 2022);
|
ST3. Similar seroresponse estimate between concomitant and non-concomitant administration of PNEU-C-15 and QIV (RR: 1.00; RD: -0.1%) Subgroup data by age and PNEU-P-23 vaccination history not provided. |
Moderate Table 11 Footnote a PNEU-C-15 administered with QIV probably results in a similar proportion of seroresponders for ST3 compared to PNEU-C-15 administered non-concomitantly with QIV. |
Vaccine-related Serious AE Through 7 months after vaccine |
1 RCT (Severance 2022);
|
No vaccine-related events observed in either group. |
Moderate Table 11 Footnote b There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of SAEs through 7 months after vaccine administration. None of those events were deemed to be vaccine-related by study authors. AEs listed were for the study population as a whole, which included 50% of the population <65 years of age. |
Serious AE Through 7 months after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 1.45 (0.62 to 3.40) Absolute effects: 13 more per 1,000 (11 fewer to 65 more) |
|
Severe Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 0.32 (0.13 to 0.82) Absolute effects: 16 fewer per 1,000 (20 fewer to 4 fewer) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably a trivial difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of severe fatigue within 14 days after vaccine administration. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 1.64 (0.41 to 6.59) Absolute effects: 3 more per 1,000 (3 fewer to 27 more) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of severe headache within 14 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 0.36 (0.13 to 0.97) Absolute effects: 13 fewer per 1,000 (17 fewer to 1 fewer) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably a trivial difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of severe muscle pain within 14 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 0.18 (0.06 to 0.58) Absolute effects: 15 fewer per 1,000 (17 fewer to 8 fewer) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably a trivial difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of severe joint pain within 14 days after vaccine administration. |
Severe Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 0.13 (0.01 to 1.29) Absolute effects: 4 fewer per 1,000 (5 fewer to 1 more) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of severe fever within 5 days after vaccine administration. |
Mild/moderate Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: RR 0.96 (0.79 to 1.15) Absolute effects: 11 fewer per 1,000 (58 fewer to 42 more) |
Moderate Table 11 Footnote d Table 11 Footnote e There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of mild/moderate fatigue within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: RR 0.89 (0.72 to 1.11) Absolute effects: 25 fewer per 1,000 (64 fewer to 25 more) |
Moderate Table 11 Footnote d Table 11 Footnote e There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of mild/moderate headache within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: RR 1.18 (0.95 to 1.48) Absolute effects: 35 more per 1,000 (10 fewer to 93 more) |
Moderate Table 11 Footnote d Table 11 Footnote e There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of mild/moderate muscle pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: RR 0.94 (0.66 to 1.34) Absolute effects: 6 fewer per 1,000 (33 fewer to 33 more) |
Moderate Table 11 Footnote d Table 11 Footnote e There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of mild/moderate joint pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Severance 2022);
|
Relative effects: Peto OR 1.77 (0.62 to 5.08) Absolute effects: 6 fewer per 1,000 (3 fewer to 33 more) |
Moderate Table 11 Footnote c Table 11 Footnote d There is probably little to no difference between concomitant and non-concomitant administration of PNEU-C-15 and QIV in the occurrence of mild/moderate fever within 5 days after vaccine administration. |
Abbreviations: AE = adverse events; OR = odds ratio; RR = relative risk; RCT = randomised controlled trial; SAE = Serious adverse events; vs = versus.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses.) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers (per protocol) 1 month after vaccine |
1 RCT (Peterson);
|
Non-inferiority was not evaluated. Additional data (not GRADEd) Shared serotypes All except ST3: GMT ratio estimate ranged 0.68 (4) to 1.23 (6B). ST3: 1.6. Unique serotypes. 22F: 13.9; 33F: 3.5. Numerically higher responses for the unique serotypes. |
No GRADE rating Table 12 Footnote a |
% Seroresponders(≥4-fold risk in GMFR) (per protocol) 1 month after vaccine |
1 RCT (Peterson);
|
Shared serotypes: All except ST3: RR range 0.80 to 1.25. ST3: RR 1.37. Favours PNEU-C-15 except for serotypes 4, 5, 6A, 6B, and 7F. Unique serotypes, 22F: RR 5.13; 33F : RR 6.10. Numerically higher proportion of seroresponders with most serotypes, favouring PNEU-C-15. |
Low Table 12 Footnote b Table 12 Footnote c PNEU-C-15 may result in a numerically higher proportion of seroresponders for most serotypes compared with PNEU-C-13. |
Vaccine-related Serious AE Up to 6 months after vaccine |
1 RCT (Peterson);
|
No vaccine related events observed in either group. |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in SAEs between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. None were vaccine related |
Serious AE Up to 6 months after vaccine |
1 RCT (Peterson);
|
Relative effects: Peto OR 0.13 (0.01 to 2.14) Absolute effects: 14 fewer per 1,000 (from 16 fewer to 17 more) The two AEs in the PNEU-C-13 group were acute myocardial infarction and periprosthetic fracture. |
|
Severe Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: Peto OR: 0.99 (0.06 to 15.95) Absolute effects: 7 fewer per 1,000 (from 16 fewer to 105 more) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in severe fatigue between PNEU-C-15 and PNEU-C-13. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: Peto OR: 0.13 (0.003 to 6.77) Absolute effects: 7 fewer per 1,000 (8 fewer to 21 more) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in severe headache between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE - Muscle pain Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: Peto OR: 7.33 (0.15 to 369.5) Absolute effectse: 10 more per 1,000 (10 fewer to 30 more per 1,000). |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in severe muscle pain between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE - Joint pain Up to 14 days after vaccine |
1 RCT (Peterson);
|
No events observed in either group. |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in severe joint pain between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Peterson);
|
No events observed in either group. |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in severe fever between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Peterson); |
Relative effects: RR 0.95 (0.56 to 1.61) |
Moderatec,d |
Mild/moderate Systemic AE – Headache Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: RR 0.89 (0.48 to 1.63) Absolute effects: 17 fewer per 1,000 (78 fewer to 95 more) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in mild/moderate headache between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: RR 1.33 (0.70 to 2.53) Absolute effects: 37 more per 1,000 (33 fewer to 170 more) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in mild/moderate muscle pain between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: RR 0.63 (0.25 to 1.58) Absolute effects: 32 fewer per 1,000 (65 fewer to 51 more) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in mild/moderate joint pain between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23 |
Mild/moderate Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Peterson);
|
Relative effects: Peto OR: 7.39 (0.46 to 118.80) Absolute effects: 20 more per 1,000 (10 fewer to 40 more per 1,000) |
Moderate Table 12 Footnote c Table 12 Footnote d There is probably little to no difference in mild/moderate fever between PNEU-C-15 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; SAE = Serious adverse events; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers (per protocol) 1 month after vaccine |
2 RCTs (Ermlich 2018; Hammitt 2022)
|
Shared serotypes Additional data (not GRADEd) Shared serotype data. All except ST3. Varied results between studies and by condition, using GMT ratio of 1 as a threshold, but analyses by condition had low power. ST3. All analyses with GMT ratio >1. Unique serotypes, 22F, 33F. GMT ratio estimates >1 across studies/analyses. Numerically higher responses for the unique serotypes, but some analyses had low power. |
No GRADE rating Table 13 Footnote a Whether PNEU-C-15 is non-inferior to PNEU-C-13 is not known. |
% Seroresponders(≥4-fold risk in risk in serotype specific OPA) 1 month after vaccine |
2 RCTs (Ermlich 2018; Hammitt 2022)
|
Shared serotypes except ST3. Mixed results between studies and across conditions in serotypes showing a higher numerical seroresponse estimate with PNEU-C-15. ST3. Numerically higher proportion of seroresponders with PNEU-C-15 (RR range 1.10 to 1.18; RD range 5.4% to 14%). Unique serotypes. Analyses showing numerically higher proportion of seroresponders with PNEU-C-15 for all but one analysis (22F for diabetes subgroup). |
There may be a higher numerical proportion of seroresponders with PNEU-C-15 for the unique serotypes (22F, 33F) and ST3 but unclear for remaining shared serotypes. |
Vaccine-related Serious AE Up to 6 months after vaccine |
1 RCT (Hammitt 2022)
|
No vaccine-related events observed. |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of SAEs up to 6 months after vaccine administration. None of those events were deemed to be vaccine-related by study authors. This study reported only on the number of deaths in each group (3 vs 2). |
Serious AE Up to 6 months after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: RR 1.45 (0.68 to 3.10) Absolute effects: 13 more per 1,000 (9 fewer to 60 more) SAEs by the relevant population group were not listed. |
|
Severe Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: Peto OR 1.21 (0.36 to 4.08) Absolute effects: 2 more per 1,000 (5 fewer to 24 more) |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe fatigue within 14 days after vaccine administration. |
Severe Systemic AE – Headache Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: Peto OR 1.21 (0.36 to 4.08) Absolute effects: 1 more per 1,000 (3 fewer to 16 more) |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe headache within 14 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: Peto OR 0.45 (0.06 to 3.40) Absolute effects: 3 fewer per 1,000 (5 fewer to 12 more) |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe muscle pain within 14 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: Peto OR 3.80 (0.39 to 36.65) Absolute effects: 0 per 1,000 (0 to 10 more) |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe joint pain within 14 days after vaccine administration. |
Severe Systemic AE – Fever Up to 5 days after vaccine |
No studies addressed this outcome |
||
Mild/moderate Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: RR 0.93 (0.79 to 1.08) Absolute effects: 25 fewer per 1,000 (76 fewer to 29 more) |
High There is little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate fatigue within 14 days after vaccine administration. |
Mild/moderate Systemic AE – Headache Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: RR 1.05 (0.86 to 1.29) Absolute effects: 12 more per 1,000 (34 fewer to 71 more) |
Moderate Table 13 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate headache within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: RR 1.10 (0.91 to 1.34) Absolute effects: 26 more per 1,000 (23 fewer to 88 more) |
High There is little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate muscle pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Hammitt 2022)
|
Relative effects: RR 1.06 (0.77 to 1.46) Absolute effects: 7 more per 1,000 (27 fewer to 54 more) |
Moderate Table 13 Footnote d There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate joint pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE – Fever Up to 5 days after vaccine |
No studies addressed this outcome |
||
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; SAE = Serious adverse events; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers 1 month after vaccine |
1 RCT (Mohapi 2022) |
Non-inferiority was not evaluated Additional data (not GRADEd): One study (Mohapi 2022) in adults ≥18 years living with HIV reported OPA GMTs (range N 299-300 across groups by serotype analysis). All serotypes except serotypes 4 and 7F showed numerically higher GMTs for PNEU-C-15 compared to PNEU-C-13. GMT ratios ranged from 0.55 (4) to 1.81 (18C) for shared serotypes and the lowest 95% CI lower bound across serotypes was 0.38. For unique serotypes, GMT ratios were 42.86 (95% CI 26.53 to 69.25) and 5.41 (4.07 to 7.19) for ST22F and ST33F, respectively. Subgroups for age (18-49y vs ≥50y), shared serotypes. One study (Mohapi 2022) reported OPA GMTs for 18-49 and ≥50 year subgroups; however, GMT ratios and corresponding 95% confidence intervals were not provided. GMTs were numerically higher for PNEU-C-15 across subgroups for the following serotypes: 1, 3, 6A, 6B, 9V, 14, 18C, 19A, and 19F. Serotype 4 showed a numerically lower GMT for PNEU-C-15 in both subgroups. For remaining serotypes (i.e., 5, 7F, 23F), GMTs were numerically higher for PNEU-C-15 for all three serotypes for the ≥50-year subgroup but numerically lower for the same serotypes for the 18-49 year subgroup. Subgroups for age (18-49y vs ≥50y), unique serotypes. GMTs were numerically higher for PNEU-C-15 for both unique serotypes (i.e., 22F and 33F) across subgroups. |
No GRADE rating Table 14 Footnote a |
% Seroresponders 1 month after vaccine |
1 RCT (Mohapi 2022);
|
Shared serotypes except ST3. Numerically higher proportion of seroresponders with PNEU-C-15 than PNEU-C-13 for all shared serotypes except serotypes 1, 4, 5, and 7F. |
PNEU-C-15 may result in a numerically higher proportion of seroresponders for most shared serotypes compared with PNEU-C-13. |
% Seroresponders 1 month after vaccine |
1 RCT (Mohapi 2022);
|
Shared serotype, ST3. Higher numerical seroresponse estimate with PNEU-C-15 (RR 1.53; RD 20.3) |
PNEU-C-15 may result in a numerically higher proportion of seroresponders for ST3 as compared to PNEU-C-13. |
% Seroresponders 1 month after vaccine |
1 RCT (Mohapi 2022);
|
Unique serotype, ST22F. Higher numerical seroresponse estimate with PNEU-C-15 (RR 5.68; RD 64.1). Unique serotype, ST33F. Higher numerical seroresponse estimate with PNEU-C-15 (RR 11.04; RD 49.2) |
PNEU-C-15 may result in a numerically higher proportion of seroresponders for both unique serotypes as compared to PNEU-C-13. |
Vaccine-related Serious AE Up to week 8 |
1 RCT (Mohapi 2022);
|
No vaccine-related serious AE observed in either group. |
Moderate Table 14 Footnote c |
Serious AE Up to week 8 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 7.39 (0.76 to 71.59) Absolute effects: 0 fewer per 1,000 (0 fewer to 0 fewer) The three events with PNEU-C-15 were musculoskeletal/connective tissue disorder, transient ischaemic attack (nervous system), suicide. Subgroups for age (18-49y vs ≥50y). One study (Mohapi 2022) provided data on SAEs for 18-49 and ≥50 years olds. Due to too few studies, subgroup analyses could not be performed. Confidence intervals around relative effect estimates overlapped between age groups; however, there were small number of events [18-49 years – Peto OR 7.67, 95% CI: 0.15-386.82; ≥50 years – Peto OR 6.62, 95% CI: 0.40-108.34]. |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in SAEs. None were vaccine related.
|
Severe Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
No events observed. |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe fatigue within 14 days after vaccine administration. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.99 (0.06 to 15.85) Absolute effects: 0 fewer per 1,000 (6 fewer to 89 more) |
Moderate Table 14 Footnote d There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe headache within 14 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
No events observed. |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe muscle pain within 14 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
No events observed. |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe joint pain within 14 days after vaccine administration. |
Severe Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Mohapi 2022);
|
No events observed. |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of severe fever up to 5 days after vaccination. |
Mild/moderate Systemic AE - Fatigue Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: RR 1.53 (0.91 to 2.56) Absolute effects: 71 more per 1,000 (12 fewer to 208 more) |
Moderate Table 14 Footnote d There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate fatigue within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: RR 1.34 (0.70 to 2.57) Absolute effects: 32 more per 1,000 (28 fewer to 147 more) |
Moderate Table 14 Footnote d There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate headache within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: RR 1.34 (0.70 to 2.57) Absolute effects: 32 more per 1,000 (28 fewer to 147 more) |
Moderate Table 14 Footnote d There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate muscle pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.82 (0.25 to 2.72) Absolute effects: 7 fewer per 1,000 (30 fewer to 62 more) |
Moderate Table 14 Footnote c There is probably little to no difference between PNEU-C-15 and PNEU-C-13 in the occurrence of mild/moderate joint pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 1.93 (0.20 to 18.7) Absolute effects: 6 more per 1,000 (5 fewer to 105 more) |
Moderate Table 14 Footnote d |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; SAE = Serious adverse events; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-15+PNEU-P-23 vs PNEU-C-13+PNEU-P-23. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers 12 weeks (1 month after PNEU-P-23 vaccine) |
1 RCT (Mohapi 2022) |
No studies evaluated non-inferiority. Additional data (not GRADEd): One study in adults ≥18 years living with HIV reported OPA GMTs (range N 299-300 across groups by serotype analysis) but did not evaluate non-inferiority. All serotypes except serotypes 4 and 33F showed numerically higher GMTs for PNEU-C-15+PNEU-P-23 compared to PNEU-C-13+PNEU-P-23. GMT ratios ranged from 0.99 (ST4) to 1.57 (ST18C) for shared serotypes and the lowest 95% CI lower bound across serotypes was 0.72. For unique serotypes, GMT ratios were 1.15 (95% CI 0.81 to 1.64) and 0.90 (0.67 to 1.21) for ST22F and ST33F, respectively. |
No GRADE rating Table 15 Footnote a |
% Seroresponders 12 weeks (1 month after PNEU-P-23 vaccine) |
1 RCT (Mohapi 2022);
|
Shared serotypes except ST3. Numerically higher proportion of seroresponders with PNEU-C-15+PNEU-P-23 than PNEU-C-13+PNEU-P-23 for all shared serotypes except serotypes 9V. |
|
% Seroresponders 12 weeks (1 month after PNEU-P-23 vaccine) |
1 RCT (Mohapi 2022);
|
Shared serotype, ST3. Lower numerical seroresponse estimate with PNEU-C-15+PNEU-P-23 (RR 0.97; RD -1.8) compared to PNEU-C-13+PNEU-P-23. |
PNEU-C-15+PNEU-P-23 may result in a numerically lower proportion of seroresponders for ST3 as compared to PNEU-C-13+PNEU-P-23. |
% Seroresponders 12 weeks (1 month after PNEU-P-23 vaccine) |
1 RCT (Mohapi 2022);
|
Unique serotype, ST22F. Lower numerical seroresponse estimate with PNEU-C-15+PNEU-P-23 (RR 0.98; RD -1.7). Unique serotype, ST33F. Lower numerical seroresponse estimate with PNEU-C-15+PNEU-P-23 (RR 0.90; RD -6.9) |
PNEU-C-15+PNEU-P-23 may result in a numerically lower proportion of seroresponders for both unique serotypes as compared to PNEU-C-13+PNEU-P-23. |
Vaccine-related Serious AE From week 8 up to month 6 |
1 RCT (Mohapi 2022);
|
No vaccine-related serious AE observed in either group. |
Moderate Table 15 Footnote c |
Serious AE From week 8 up to month 6 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.35 (0.09 to 1.44) Absolute effects: 26 fewer per 1,000 (37 fewer to 17 more) The two events with PNEU-C-15+PNEU-P-23 were appendicitis and pulmonary embolism. Events with PNEU-C-13+PNEU-P-23 were chest pain, herpes zoster, peritonitis, soft tissue infection, foot fracture, and dry gangrene. |
Moderate Table 15 Footnote c There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in serious adverse events. None were vaccine related. |
Severe Systemic AE - Fatigue Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.99 (0.06 to 15.85) Absolute effects: 0 fewer per 1,000 (6 fewer to 91 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of severe fatigue within 14 days after vaccine administration. |
Severe Systemic AE - Headache Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.13 (0.00 to 6.73) Absolute effects: 6 fewer per 1,000 (- to 37 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of severe headache within 14 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 7.29 (0.14 to 367.49) Absolute effects: 0 fewer per 1,000 (0 fewer to 0 fewer) |
Moderate Table 15 Footnote c There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of severe muscle pain within 14 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 7.29 (0.14 to 367.49) Absolute effects: 0 fewer per 1,000 (0 fewer to 0 fewer) |
Moderate Table 15 Footnote c There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of severe joint pain within 14 days after vaccine administration. |
Severe Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Mohapi 2022);
|
No events observed. |
Moderate Table 15 Footnote c There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of severe fever up to 5 days after vaccination. |
Mild/moderate Systemic AE - Fatigue Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: RR 1.18 (0.62 to 2.26) Absolute effects: 18 more per 1,000 (39 fewer to 128 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of mild/moderate fatigue within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Headache Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: RR 1.07 (0.50 to 2.27) Absolute effects: 6 more per 1,000 (41 fewer to 103 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of mild/moderate headache within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: RR 0.88 (0.47 to 1.65) Absolute effects: 15 fewer per 1,000 (64 fewer to 79 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of mild/moderate muscle pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccination with PNEU-P-23 |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 1.48 (0.25 to 8.64) Absolute effects: 6 more per 1,000 (10 fewer to 92 more) |
Moderate Table 15 Footnote d There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of mild/moderate joint pain within 14 days after vaccine administration. |
Mild/moderate Systemic AE - Fever Up to 5 days after vaccine |
1 RCT (Mohapi 2022);
|
Relative effects: Peto OR 0.66 (0.19 to 2.28) Absolute effects: 14 fewer per 1,000 (33 fewer to 52 more) |
Moderate Table 15 Footnote c There is probably little to no difference between PNEU-C-15+PNEU-P-23 and PNEU-C-13+PNEU-P-23 in the occurrence of mild/moderate fever up to 5 days after vaccination. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-15 = 15-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-20 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses. For immunogenicity data, specific serotypes are provided in parentheses) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers 1 month after vaccine |
1 RCT (Essink 2021);
|
Shared serotypes All except ST3: GMT ratio estimate ranged 0.76 (ST6A) to 1.00 (ST14). ST3: 0.85. Non-inferiority for PNEU-C-20 met for all shared serotypes (margin >0.5; lowest CI bound across serotypes 0.66 [ST6A]). Additional data (not GRADEd): Shared serotypes. One additional study (Hurley 2021) in adults 60-64 years provided immunogenicity information (range N 400-413 across groups by serotype analysis) but did not evaluate non-inferiority. All serotypes showed numerically lower GMT mean titers for PNEU-C-20 compared to PNEU-C-13 (GMT ratio <1.00 for all serotypes). Subgroups for age (50-59y vs 60-64y). One study (Essink 2021) bridged PNEU-C-20 -elicited immune responses in younger participants (50-59 years) to those in older adults (60-64 years). PNEU-C-20 met non-inferiority for all 13 shared serotypes for participants aged 50-59 as compared to those 60-64 years. |
Moderate Table 16 Footnote a Table 16 Footnote b PNEU-C-20 is probably not inferior to PNEU-C-13 in immune response for shared serotypes. |
% Seroresponders 1 month after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Shared serotypes except ST3. Both studies report numerically lower proportion of seroresponders with PNEU-C-20 than PNEU-C-13 for all but one serotype. The only serotypes showing a higher proportion of seroresponders with PNEU-C-20 were ST14 in one study and ST6A in the second study. |
Moderate Table 16 Footnote a Table 16 Footnote b PNEU-C-20 probably results in a numerically lower proportion of seroresponders for most serotypes compared with PNEU-C-13. Data not available for unique serotypes for this comparison. |
% Seroresponders 1 month after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Shared serotype, ST3. Lower numerical seroresponse estimate with PNEU-C-20 (RR range 0.91-0.93; RD range |
Moderatea Table 16 Footnote a Table 16 Footnote b PNEU-C-20 probably results in a numerically lower proportion of seroresponders for ST3 as compared to PNEU-C-13. |
Vaccine-related Serious AE Up to 1 month after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
No vaccine-related serious AE observed in either group. |
Moderate Table 16 Footnote b Table 16 Footnote c |
Serious AE Up to 1 month after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 0.88 (0.34 to 2.28) Absolute effects: 1 fewer per 1,000 (3 fewer to 7 more) Studies did not report type of SAEs that occurred after first vaccine (PNEU-C-20 or PNEU-C-13). Types of SAEs were only reported at longer follow-up (after second vaccine with saline or PNEU-P-23). Additional data (not GRADEd): Subgroups for age (50-59y vs ≥60y). One study (Essink 2021) provided data on serious adverse events as well as mild/moderate and severe systemic adverse events for 50-59 and ≥60 year-olds. Due to too few studies, subgroup analyses could not be performed. Confidence intervals around relative effect estimates overlapped between age groups for serious adverse events and all systemic events; however, there were small number of events for some safety outcomes (i.e., serious adverse events and severe systemic events). |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of serious adverse events after vaccine administration. None of those events were deemed to be vaccine-related by study authors. |
Severe Systemic AE - Fatigue Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 0.85 (0.46 to 1.58) Absolute effects: 2 fewer per 1,000 (7 fewer to 7 more) Additional data (not GRADEd): Subgroups for age (50-59y vs ≥60y). As above. |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of severe fatigue within 7 days after vaccine administration. |
Severe Systemic AE - Headache Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021) |
Relative effects: Peto OR 1.55 (0.61 to 3.90) Additional data (not GRADEd): |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of severe headache within 7 days after vaccine administration. |
Severe Systemic AE – Muscle Pain Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 0.84 (0.28 to 2.51) Absolute effects: 1 fewer per 1,000 (3 fewer to 6 more) Additional data (not GRADEd): Subgroups for age (50-59y vs ≥60y). As above. |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of severe muscle pain within 7 days after vaccine administration. |
Severe Systemic AE – Joint Pain Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 1.23 (0.33 to 4.57) Absolute effects: 1 more per 1,000 (2 fewer to 8 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of severe joint pain within 7 days after vaccine administration. |
Severe Systemic AE - Fever Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 1.63 (0.41 to 6.51) Absolute effects: 1 more per 1,000 (1 fewer to 10 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of severe fever within 7 days after vaccine administration. |
Mild/moderate Systemic AE - Fatigue Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: RR 0.99 (0.90 to 1.10) Absolute effects: 3 fewer per 1,000 (29 fewer to 29 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
High Table 16 Footnote b There is little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of mild/moderate fatigue within 7 days after vaccine administration. |
Mild/moderate Systemic AE - Headache Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: RR 0.91 (0.80 to 1.03) Absolute effects: 21 fewer per 1,000 (46 fewer to 7 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
High Table 16 Footnote b There is little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of mild/moderate headache within 7 days after vaccine administration. |
Mild/moderate Systemic AE - Muscle Pain Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: RR 1.07 (0.98 to 1.16) Absolute effects: 26 more per 1,000 (7 fewer to 59 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
High Table 16 Footnote b There is little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of mild/moderate muscle pain within 7 days after vaccine administration. |
Mild/moderate Systemic AE - Joint Pain Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: RR 0.93 (0.79 to 1.11) Absolute effects: 9 fewer per 1,000 (28 fewer to 15 more) Additional data (not GRADEd): Subgroups for age (50-59y vs 60-64y). As above. |
High Table 16 Footnote b There is little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of mild/moderate joint pain within 7 days after vaccine administration. |
Mild/moderate Systemic AE - Fever Up to 7 days after vaccine |
2 RCTs (Essink 2021, Hurley 2021)
|
Relative effects: Peto OR 0.89 (0.36 to 2.19) Absolute effects: 1 fewer per 1,000 (4 fewer to 7 more) |
Moderate Table 16 Footnote b Table 16 Footnote c There is probably little to no difference between PNEU-C-20 and PNEU-C-13 in the occurrence of mild/moderate fever within 7 days after vaccine administration. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RR = relative risk; RCT = randomised controlled trial; vs = versus.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-20 vs PNEU-C-13. Relative and absolute effects shown with 95% CI in parentheses.) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers |
No comparative immunogenicity data are available |
||
% Seroresponders |
|||
Vaccine-related Serious AE Up to 6 months after vaccine |
1 RCT (Cannon 2021);
|
No vaccine related events observed in either group. |
There may be little to no difference in serious adverse events between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. None were vaccine related. |
Serious AE Up to 6 months after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR 0.44 (0.05 to 3.65) Absolute effects: 9 fewer per 1,000 (from 16 fewer to 41 more) Type of serious AE not reported. |
|
Severe Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR: 0.04 (0.004 to 0.51) Absolute effects: 24 fewer per 1,000 (from 25 fewer to 12 fewer) |
There may be little to no difference in severe fatigue between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR: 4.39 (0.07 to 289.42) Absolute effectsb: 0 per 1,000 (10 fewer to 20 more) |
There may be little to no difference in severe headache between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE - Muscle pain Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR: 0.14 (0.02 to 1.15) Absolute effects: 21 fewer per 1,000 (24 fewer to 4 more) |
There may be little to no difference in severe muscle pain between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE - Joint pain Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR: 0.05 (0.001 to 3.00) Absolute effects: 8 fewer per 1,000 (8 fewer to 16 more) |
There may be little to no difference in severe joint pain between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Severe Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
No events observed in either group. |
There may be little to no difference in severe fever between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: RR 1.45 (0.97 to 2.19) Absolute effects: 89 more per 1,000 (6 fewer to 236 more) |
There may be little to no difference in mild/moderate fatigue between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE – Headache Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: RR 0.96 (0.60 to 1.52) Absolute effects: 7 fewer per 1,000 (73 fewer to 95 more) |
There may be little to no difference in mild/moderate headache between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: RR 0.68 (0.33 to 1.37) Absolute effects: 32 fewer per 1,000 (66 fewer to 37 more) |
There may be little to no difference in mild/moderate joint pain between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: RR 1.09 (0.78 to 1.53) Absolute effects: 26 more per 1,000 (64 fewer to 153 more) |
There may be little to no difference in mild/moderate muscle pain between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Mild/moderate Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Cannon 2021);
|
Relative effects: Peto OR: 4.39 (0.23 to 85.53) Absolute effectsb: 10 more per 1,000 (10 fewer to 20 more) |
There may be little to no difference in mild/moderate fever between PNEU-C-20 and PNEU-C-13 in individuals previously vaccinated with PNEU-P-23. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-20 = 20-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; vs = versus; y=years.
|
|||
| Outcome | Studies contributing data; n/N (where available) | Synthesised result (Relative effects as PNEU-C-20 vs PNEU-P-23. Relative and absolute effects shown with 95% CI in parentheses.) |
GRADE certainty of evidence rating |
|---|---|---|---|
Geometric Mean Titers |
No comparative immunogenicity data are available |
||
% Seroresponders |
|||
Vaccine-related Serious AE Up to 6 months after vaccine |
1 RCT (Cannon 2022);
|
No vaccine related events observed in either group. |
There may be little to no difference in serious adverse events between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Serious AE |
1 RCT (Cannon 2022);
|
Relative effects: Peto OR 4.65 (0.85 to 25.46) Absolute effectsb: 20 more per 1,000 (0 to 5 more) |
|
Severe Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: Peto OR: 4.58 (0.42 to 50.32) Absolute effectsb: 10 more per 1,000 (10 fewer to 30 more) |
There may be little to no difference in severe fatigue between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Mild/moderate Systemic AE – Fatigue Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: RR 0.89 (0.65 to 1.22) Absolute effects: 37 fewer per 1,000 (127 fewer to 73 more) |
There may be little to no difference in mild/moderate fatigue between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Severe Systemic AE - Muscle pain Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: Peto OR: 0.05 (0.01 to 0.57) Absolute effects: 23 fewer per 1,000 (24 fewer to 10 fewer) |
There may be little to no difference in severe muscle pain between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Severe Systemic AE - Headache Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
No events observed in either group. |
There may be little to no difference in severe headache between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Mild/moderate Systemic AE – Headache Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: RR 0.63 (0.40 to 1.00) |
There may be little to no difference in mild/moderate headache between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Severe Systemic AE - Joint pain Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
No events observed in either group. |
There may be little to no difference in severe joint pain between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Mild/moderate Systemic AE - Joint Pain Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: RR 0.75 (0.44 to 1.26) Absolute effects: 40 fewer per 1,000 (89 fewer to 41 more) |
There may be little to no difference in mild/moderate joint pain between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Severe Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
No events observed in either group. |
There is maybe little to no difference in severe fever between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Mild/moderate Systemic AE - Muscle Pain Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: RR 0.77 (0.60 to 1.01) Absolute effects: 100 fewer per 1,000 (175 fewer to 4 more) |
There may be little to no difference in mild/moderate muscle pain between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Mild/moderate Systemic AE – Fever Up to 14 days after vaccine |
1 RCT (Cannon 2022);
|
Relative effects: Peto OR: 0.05 (0.002 to 0.98) Absolute effects: 15 fewer per 1,000 (16 fewer to 0 fewer) |
There may be little to no difference in mild/moderate fever between PNEU-C-20 and PNEU-P-23 in individuals previously vaccinated with PNEU-C-13. |
Abbreviations: AE = adverse events; OR = odds ratio; PNEU-C-13 = 13-valent pneumococcal conjugate vaccine; PNEU-C-20 = 20-valent pneumococcal conjugate vaccine; PNEU-P-23 = 23-valent pneumococcal polysaccharide vaccine; RCT = randomised controlled trial; RD = risk difference; RR = relative risk; vs = versus; y=years.
|
|||
|
Strong | Discretionary |
|---|---|---|
| Wording | “should/should not be offered” | “may/may not be offered” |
| Rationale | Known/anticipated advantages outweigh known/anticipated disadvantages (“should”), or Known/anticipated disadvantages outweigh known/anticipated advantages (“should not”) |
Known/anticipated advantages are closely balanced with known/anticipated disadvantages, or Uncertainty in the evidence of advantages and disadvantages exists |
| Implications | A strong recommendation applies to most populations/individuals and should be followed unless a clear and compelling rationale for an alternative approach is present. | A discretionary recommendation may be offered for some populations/individuals in some circumstances. Alternative approaches may be reasonable. |
Epidemiology tables
| Serotype (n by year) | 2016 (n=2855) | 2017 (n=3270) | 2018 (n=3328) | 2019 (n=3673) | 2020 (n=2108) |
|---|---|---|---|---|---|
| 1Footnote * (4,0,0,0,1)Footnote ‡ | 0.1% | 0.0% | 0.0% | 0.0% | 0.0% |
| 3Footnote * (272,312,398,427,229) | 9.5% | 9.5% | 12.0% | 11.6% | 10.9% |
| 4Footnote * (182,234,205,262,237) | 6.4% | 7.2% | 6.2% | 7.1% | 11.2% |
| 6AFootnote * (19,7,14,8,3) | 0.7% | 0.2% | 0.4% | 0.2% | 0.1% |
| 6BFootnote * (20,9,8,8,1) | 0.7% | 0.3% | 0.2% | 0.2% | 0.0% |
| 7FFootnote * (109,116,106,119,59) | 3.8% | 3.5% | 3.2% | 3.2% | 2.8% |
| 9VFootnote * (5,15,35,48,54) | 0.2% | 0.5% | 1.1% | 1.3% | 2.6% |
| 14Footnote * (16,29,13,11,6) | 0.6% | 0.9% | 0.4% | 0.3% | 0.3% |
| 18CFootnote * (9,8,4,15,9) | 0.3% | 0.2% | 0.1% | 0.4% | 0.4% |
| 19AFootnote * (179,165,181,154,88) | 6.3% | 5.0% | 5.4% | 4.2% | 4.2% |
| 19FFootnote * (46,91,75,75,46) | 1.6% | 2.8% | 2.3% | 2.0% | 2.2% |
| 23FFootnote * (4,2,2,2,2) | 0.1% | 0.1% | 0.1% | 0.1% | 0.1% |
| 22FFootnote ** (260,283,292,362,149) | 9.1% | 8.7% | 8.8% | 9.9% | 7.1% |
| 33FFootnote ** (100,107,96,145,52) | 3.5% | 3.3% | 2.9% | 3.9% | 2.5% |
| 8Footnote ^ (148,158,187,221,151) | 5.2% | 4.8% | 5.6% | 6.0% | 7.2% |
| 10AFootnote ^ (51,67,65,69,52) | 1.8% | 2.0% | 2.0% | 1.9% | 2.5% |
| 11AFootnote ^ (93,95,117,100,68) | 3.3% | 2.9% | 3.5% | 2.7% | 3.2% |
| 12FFootnote ^ (102,127,160,145,120) | 3.6% | 3.9% | 4.8% | 3.9% | 5.7% |
| 15B/CFootnote ^ (132,131,105,102,49) | 4.6% | 4.0% | 3.2% | 2.8% | 2.3% |
| 2Footnote ~ (0,1,4,0,0) | 0.0% | 0.0% | 0.1% | 0.0% | 0.0% |
| 9NFootnote ~ (141,214,189,254,135) | 4.9% | 6.5% | 5.7% | 6.9% | 6.4% |
| 17FFootnote ~ (29,38,37,35,17) | 1.0% | 1.2% | 1.1% | 1.0% | 0.8% |
| 20Footnote ~ (81,118,127,134,82) | 2.8% | 3.6% | 3.8% | 3.6% | 3.9% |
| 6C (73,66,58,69,32) | 2.6% | 2.0% | 1.7% | 1.9% | 1.5% |
| 7C (45,28,57,44,24) | 1.6% | 0.9% | 1.7% | 1.2% | 1.1% |
| 13 (9,6,10,9,4) | 0.3% | 0.2% | 0.3% | 0.2% | 0.2% |
| 15A (123,155,130,159,74) | 4.3% | 4.7% | 3.9% | 4.3% | 3.5% |
| 16F (72,77,71,107,57) | 2.5% | 2.4% | 2.1% | 2.9% | 2.7% |
| 21 (14,21,15,12,4) | 0.5% | 0.6% | 0.5% | 0.3% | 0.2% |
| 23A (108,155,115,132,64) | 3.8% | 4.7% | 3.5% | 3.6% | 3.0% |
| 23B (90,104,118,118,52) | 3.2% | 3.2% | 3.5% | 3.2% | 2.5% |
| 24F (24,27,24,20,4) | 0.8% | 0.8% | 0.7% | 0.5% | 0.2% |
| 28A (5,10,10,9,7) | 0.2% | 0.3% | 0.3% | 0.2% | 0.3% |
| 29 (10,4,7,6,1) | 0.4% | 0.1% | 0.2% | 0.2% | 0.0% |
| 31 (50,51,54,45,35) | 1.8% | 1.6% | 1.6% | 1.2% | 1.7% |
| 34 (30,29,33,35,17) | 1.1% | 0.9% | 1.0% | 1.0% | 0.8% |
| 35B (64,79,76,81,48) | 2.2% | 2.4% | 2.3% | 2.2% | 2.3% |
| 35F (58,51,46,55,38) | 2.0% | 1.6% | 1.4% | 1.5% | 1.8% |
| 38 (48,53,51,27,13) | 1.7% | 1.6% | 1.5% | 0.7% | 0.6% |
| NT (6,4,10,13,2) | 0.2% | 0.1% | 0.3% | 0.4% | 0.1% |
| Other (24,23,23,36,22) | 0.8% | 0.7% | 0.7% | 1.0% | 1.0% |
|
|||||
| Serotype | 2016 | 2017 | 2018 | 2019 | 2020 | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PNEU-C-13 | PNEU-C-13 all | 40.9% | (259) | 43.6% | (281) | 38.4% | (286) | 42.0% | (343) | 47.1% | (262) | 1431 |
| 4 | 15.0% | (95) | 16.9% | (109) | 11.8% | (88) | 14.5% | (118) | 20.9% | (116) | 526 | |
| 6B | 0.2% | (1) | 0.0% | (0) | 0.1% | (1) | 0.2% | (2) | 0.0% | (0) | 4 | |
| 9V | 0.3% | (2) | 0.8% | (5) | 1.1% | (8) | 2.1% | (17) | 5.6% | (31) | 63 | |
| 14 | 0.6% | (4) | 0.6% | (4) | 0.5% | (4) | 0.2% | (2) | 0.5% | (3) | 17 | |
| 18C | 0.5% | (3) | 0.3% | (2) | 0.0% | (0) | 0.5% | (4) | 0.4% | (2) | 11 | |
| 19F | 1.7% | (11) | 2.6% | (17) | 1.9% | (14) | 2.2% | (18) | 2.0% | (11) | 71 | |
| 23F | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.1% | (1) | 0.2% | (1) | 2 | |
| 1 | 0.3% | (2) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.2% | (1) | 3 | |
| 3 | 8.5% | (54) | 8.4% | (54) | 10.1% | (75) | 10.0% | (82) | 8.8% | (49) | 314 | |
| 5 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 6A/C* | 2.4% | (15) | 0.8% | (5) | 1.7% | (13) | 0.5% | (4) | 0.7% | (4) | 41 | |
| 7F | 6.6% | (42) | 8.2% | (53) | 6.7% | (50) | 7.4% | (60) | 4.9% | (27) | 232 | |
| 19A | 4.7% | (30) | 5.0% | (32) | 4.4% | (33) | 4.3% | (35) | 3.1% | (17) | 147 | |
| PNEU-C-15 (non- PNEU-C-13) |
PNEU-C-15 all | 10.0% | (63) | 7.8% | (50) | 7.7% | (57) | 10.5% | (86) | 6.7% | (37) | 293 |
| 22F | 6.8% | (43) | 5.9% | (38) | 5.8% | (43) | 6.9% | (56) | 4.5% | (25) | 205 | |
| 33F | 3.2% | (20) | 1.9% | (12) | 1.9% | (14) | 3.7% | (30) | 2.2% | (12) | 88 | |
| PNEU-C-20 (non- PNEU-C-15) |
PNEU-C-20 all | 20.5% | (130) | 21.3% | (137) | 23.0% | (171) | 21.3% | (174) | 26.1% | (145) | 757 |
| 8 | 7.6% | (48) | 7.6% | (49) | 9.3% | (69) | 9.3% | (76) | 11.0% | (61) | 303 | |
| 10A | 0.9% | (6) | 0.8% | (5) | 1.5% | (11) | 1.2% | (10) | 1.1% | (6) | 38 | |
| 11A | 3.2% | (20) | 2.2% | (14) | 2.2% | (16) | 1.2% | (10) | 2.0% | (11) | 71 | |
| 12F | 6.5% | (41) | 8.1% | (52) | 9.0% | (67) | 8.2% | (67) | 11.2% | (62) | 289 | |
| 15B/C | 2.4% | (15) | 2.6% | (17) | 1.1% | (8) | 1.3% | (11) | 0.9% | (5) | 56 | |
| PNEU-P-23 unique | PNEU-P-23 all | 11.7% | (74) | 12.9% | (83) | 13.2% | (98) | 11.9% | (97) | 10.1% | (56) | 408 |
| 2 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 9N | 6.2% | (39) | 7.1% | (46) | 6.0% | (45) | 7.1% | (58) | 5.9% | (33) | 221 | |
| 17F | 0.8% | (5) | 0.5% | (3) | 1.3% | (10) | 0.6% | (5) | 0.2% | (1) | 24 | |
| 20 | 4.7% | (30) | 5.3% | (34) | 5.8% | (43) | 4.2% | (34) | 4.0% | (22) | 163 | |
| NVT | NVT all | 16.9% | (107) | 14.4% | (93) | 17.7% | (132) | 14.2% | (116) | 10.1% | (56) | 504 |
| 23A | 2.4% | (15) | 3.4% | (22) | 2.0% | (15) | 2.6% | (21) | 1.8% | (10) | 83 | |
| 15A | 1.6% | (10) | 2.2% | (14) | 2.3% | (17) | 1.8% | (15) | 1.4% | (8) | 64 | |
| 23B | 1.7% | (11) | 1.2% | (8) | 2.4% | (18) | 2.1% | (17) | 1.4% | (8) | 62 | |
| 16F | 2.1% | (13) | 2.0% | (13) | 1.1% | (8) | 2.0% | (16) | 0.7% | (4) | 54 | |
| 31 | 1.7% | (11) | 0.9% | (6) | 1.3% | (10) | 0.9% | (7) | 1.4% | (8) | 42 | |
| 35B | 2.1% | (13) | 0.5% | (3) | 0.9% | (7) | 1.0% | (8) | 1.1% | (6) | 37 | |
| 7C | 0.9% | (6) | 0.3% | (2) | 1.1% | (8) | 0.9% | (7) | 0.5% | (3) | 26 | |
| 35F | 0.5% | (3) | 0.9% | (6) | 0.9% | (7) | 0.5% | (4) | 0.2% | (1) | 21 | |
| 34 | 0.5% | (3) | 0.5% | (3) | 1.1% | (8) | 0.6% | (5) | 0.2% | (1) | 20 | |
| 28A | 0.5% | (3) | 0.8% | (5) | 0.8% | (6) | 0.0% | (0) | 0.2% | (1) | 15 | |
| 38 | 0.2% | (1) | 0.3% | (2) | 0.8% | (6) | 0.6% | (5) | 0.2% | (1) | 15 | |
| Other | 2.8% | (18) | 1.4% | (9) | 3.0% | (22) | 1.3% | (11) | 0.9% | (5) | 65 | |
| Total | (633) | (644) | (744) | (816) | (556) | 3393 | ||||||
| Serotype | 2016 | 2017 | 2018 | 2019 | 2020 | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PNEU-C-13 | PNEU-C-13 all | 35.7% | (274) | 37.1% | (332) | 37.1% | (357) | 32.8% | (337) | 37.8% | (249) | 1549 |
| 4 | 7.8% | (60) | 9.8% | (88) | 7.8% | (75) | 8.4% | (86) | 11.4% | (75) | 384 | |
| 6B | 0.4% | (3) | 0.2% | (2) | 0.3% | (3) | 0.0% | (0) | 0.0% | (0) | 8 | |
| 9V | 0.1% | (1) | 0.1% | (1) | 1.4% | (13) | 1.6% | (16) | 2.1% | (14) | 45 | |
| 14 | 0.4% | (3) | 0.9% | (8) | 0.2% | (2) | 0.2% | (2) | 0.2% | (1) | 16 | |
| 18C | 0.4% | (3) | 0.6% | (5) | 0.2% | (2) | 0.3% | (3) | 0.9% | (6) | 19 | |
| 19F | 1.4% | (11) | 2.8% | (25) | 2.2% | (21) | 1.0% | (10) | 1.8% | (12) | 79 | |
| 23F | 0.0% | (0) | 0.1% | (1) | 0.2% | (2) | 0.0% | (0) | 0.2% | (1) | 4 | |
| 1 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 3 | 11.3% | (87) | 11.2% | (100) | 13.2% | (127) | 11.5% | (118) | 12.6% | (83) | 515 | |
| 5 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 6A/C* | 1.6% | (12) | 2.1% | (19) | 1.9% | (18) | 2.5% | (26) | 2.0% | (13) | 88 | |
| 7F | 4.6% | (35) | 4.1% | (37) | 4.2% | (40) | 3.6% | (37) | 2.9% | (19) | 168 | |
| 19A | 7.7% | (59) | 5.1% | (46) | 5.6% | (54) | 3.8% | (39) | 3.8% | (25) | 223 | |
| PNEU-C-15 (non- PNEU-C-13) |
PNEU-C-15 all | 12.6% | (97) | 11.7% | (105) | 10.0% | (96) | 12.2% | (126) | 7.1% | (47) | 471 |
| 22F | 8.9% | (68) | 8.4% | (75) | 7.3% | (70) | 9.4% | (97) | 5.2% | (34) | 344 | |
| 33F | 3.8% | (29) | 3.3% | (30) | 2.7% | (26) | 2.8% | (29) | 2.0% | (13) | 127 | |
| PNEU-C-20 (non- PNEU-C-15) |
PNEU-C-20 all | 15.9% | (122) | 15.8% | (142) | 19.2% | (185) | 19.2% | (198) | 21.2% | (140) | 787 |
| 8 | 4.2% | (32) | 5.0% | (45) | 6.4% | (62) | 7.7% | (79) | 8.6% | (57) | 275 | |
| 10A | 1.6% | (12) | 1.8% | (16) | 1.2% | (12) | 1.9% | (20) | 1.8% | (12) | 72 | |
| 11A | 3.3% | (25) | 2.8% | (25) | 3.6% | (35) | 2.9% | (30) | 2.7% | (18) | 133 | |
| 12F | 3.5% | (27) | 4.4% | (39) | 6.2% | (60) | 4.4% | (45) | 5.8% | (38) | 209 | |
| 15B/C | 3.4% | (26) | 1.9% | (17) | 1.7% | (16) | 2.3% | (24) | 2.3% | (15) | 98 | |
| PNEU-P-23 unique | PNEU-P-23 all | 11.7% | (90) | 14.6% | (131) | 12.3% | (118) | 15.7% | (162) | 13.8% | (91) | 592 |
| 2 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 9N | 6.6% | (51) | 7.9% | (71) | 5.9% | (57) | 8.9% | (92) | 6.8% | (45) | 316 | |
| 17F | 1.7% | (13) | 1.6% | (14) | 1.1% | (11) | 0.9% | (9) | 0.8% | (5) | 52 | |
| 20 | 3.4% | (26) | 5.1% | (46) | 5.2% | (50) | 5.9% | (61) | 6.2% | (41) | 224 | |
| NVT | NVT all | 24.1% | (185) | 20.8% | (186) | 21.4% | (206) | 20.0% | (206) | 20.0% | (132) | 915 |
| 23A | 4.2% | (32) | 3.1% | (28) | 3.7% | (36) | 2.5% | (26) | 2.9% | (19) | 141 | |
| 15A | 3.8% | (29) | 3.3% | (30) | 2.9% | (28) | 2.6% | (27) | 3.6% | (24) | 138 | |
| 23B | 2.6% | (20) | 2.5% | (22) | 2.6% | (25) | 3.1% | (32) | 1.8% | (12) | 111 | |
| 16F | 2.9% | (22) | 1.9% | (17) | 2.3% | (22) | 3.1% | (32) | 2.6% | (17) | 110 | |
| 35B | 1.6% | (12) | 2.3% | (21) | 2.0% | (19) | 1.4% | (14) | 1.7% | (11) | 77 | |
| 35F | 2.0% | (15) | 1.3% | (12) | 1.1% | (11) | 1.3% | (13) | 1.7% | (11) | 62 | |
| 31 | 2.3% | (18) | 1.7% | (15) | 0.9% | (9) | 0.7% | (7) | 1.5% | (10) | 59 | |
| 7C | 1.2% | (9) | 0.7% | (6) | 1.7% | (16) | 1.3% | (13) | 0.8% | (5) | 49 | |
| 34 | 0.5% | (4) | 0.9% | (8) | 0.9% | (9) | 1.1% | (11) | 0.9% | (6) | 38 | |
| 38 | 1.0% | (8) | 0.4% | (4) | 1.0% | (10) | 0.3% | (3) | 0.6% | (4) | 29 | |
| Other | 2.1% | (16) | 2.6% | (23) | 2.2% | (21) | 2.7% | (28) | 2.0% | (13) | 101 | |
| Total | (768) | (896) | (962) | (1029) | (659) | 4314 | ||||||
| Serotype | 2016 | 2017 | 2018 | 2019 | 2020 | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PNEU-C-13 | PNEU-C-13 all | 29.1% | (307) | 26.5% | (355) | 28.8% | (367) | 29.3% | (431) | 27.4% | (197) | 1657 |
| 4 | 2.4% | (25) | 2.7% | (36) | 3.2% | (41) | 3.6% | (53) | 5.4% | (39) | 194 | |
| 6B | 1.3% | (14) | 0.5% | (7) | 0.3% | (4) | 0.4% | (6) | 0.1% | (1) | 32 | |
| 9V | 0.2% | (2) | 0.7% | (9) | 0.9% | (12) | 0.8% | (12) | 1.3% | (9) | 44 | |
| 14 | 0.8% | (8) | 1.0% | (14) | 0.3% | (4) | 0.3% | (5) | 0.1% | (1) | 32 | |
| 18C | 0.2% | (2) | 0.1% | (1) | 0.2% | (2) | 0.5% | (7) | 0.1% | (1) | 13 | |
| 19F | 1.4% | (15) | 2.6% | (35) | 2.2% | (28) | 2.1% | (31) | 2.2% | (16) | 125 | |
| 23F | 0.1% | (1) | 0.1% | (1) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 2 | |
| 1 | 0.1% | (1) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 1 | |
| 3 | 9.1% | (96) | 9.6% | (129) | 12.4% | (158) | 13.2% | (195) | 10.4% | (75) | 653 | |
| 5 | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 0 | |
| 6A/C* | 5.4% | (57) | 3.4% | (45) | 3.1% | (39) | 3.1% | (45) | 2.4% | (17) | 203 | |
| 7F | 2.2% | (23) | 1.5% | (20) | 1.2% | (15) | 1.2% | (17) | 1.1% | (8) | 83 | |
| 19A | 6.0% | (63) | 4.3% | (58) | 5.0% | (64) | 4.1% | (60) | 4.2% | (30) | 275 | |
| PNEU-C-15 (non- PNEU-C-13) |
PNEU-C-15 all | 12.7% | (134) | 12.7% | (171) | 14.2% | (181) | 15.4% | (226) | 13.2% | (95) | 807 |
| 22F | 10.1% | (106) | 10.1% | (135) | 11.0% | (140) | 11.5% | (169) | 10.3% | (74) | 624 | |
| 33F | 2.7% | (28) | 2.7% | (36) | 3.2% | (41) | 3.9% | (57) | 2.9% | (21) | 183 | |
| PNEU-C-20 (non- PNEU-C-15) |
PNEU-C-20 all | 16.8% | (177) | 15.9% | (213) | 15.1% | (192) | 13.5% | (199) | 15.2% | (109) | 890 |
| 8 | 5.2% | (55) | 4.2% | (57) | 3.5% | (44) | 3.9% | (58) | 3.5% | (25) | 239 | |
| 10A | 1.5% | (16) | 1.9% | (26) | 2.0% | (25) | 2.2% | (32) | 2.5% | (18) | 117 | |
| 11A | 4.2% | (44) | 3.6% | (48) | 4.5% | (57) | 3.2% | (47) | 4.3% | (31) | 227 | |
| 12F | 2.6% | (27) | 2.2% | (30) | 2.0% | (25) | 1.9% | (28) | 2.6% | (19) | 129 | |
| 15B/C | 3.3% | (35) | 3.9% | (52) | 3.2% | (41) | 2.3% | (34) | 2.2% | (16) | 178 | |
| PNEU-P-23 unique | PNEU-P-23 all | 7.2% | (76) | 10.4% | (139) | 9.9% | (126) | 10.1% | (149) | 11.1% | (80) | 570 |
| 2 | 0.0% | (0) | 0.1% | (1) | 0.0% | (0) | 0.0% | (0) | 0.0% | (0) | 1 | |
| 9N | 4.2% | (44) | 6.8% | (91) | 6.2% | (79) | 6.3% | (93) | 7.5% | (54) | 361 | |
| 17F | 0.9% | (10) | 1.3% | (17) | 1.2% | (15) | 1.4% | (20) | 1.5% | (11) | 73 | |
| 20 | 2.1% | (22) | 2.2% | (30) | 2.5% | (32) | 2.4% | (36) | 2.1% | (15) | 135 | |
| NVT | NVT all | 34.2% | (360) | 34.6% | (464) | 32.0% | (408) | 31.7% | (467) | 33.0% | (237) | 1936 |
| 15A | 7.1% | (75) | 7.1% | (95) | 6.0% | (77) | 6.8% | (100) | 4.7% | (34) | 381 | |
| 23A | 5.0% | (53) | 6.7% | (90) | 3.8% | (49) | 5.1% | (75) | 4.7% | (34) | 301 | |
| 16F | 3.2% | (34) | 3.2% | (43) | 2.8% | (36) | 3.3% | (48) | 4.2% | (30) | 198 | |
| 35B | 2.8% | (30) | 3.4% | (45) | 3.3% | (42) | 3.4% | (50) | 3.8% | (27) | 194 | |
| 23B | 2.9% | (31) | 3.4% | (46) | 4.0% | (51) | 3.3% | (49) | 2.9% | (21) | 191 | |
| 35F | 2.7% | (28) | 1.8% | (24) | 1.7% | (22) | 2.1% | (31) | 3.2% | (23) | 128 | |
| 31 | 1.9% | (20) | 2.1% | (28) | 2.7% | (34) | 1.7% | (25) | 2.4% | (17) | 124 | |
| 38 | 2.2% | (23) | 1.9% | (26) | 1.6% | (20) | 1.0% | (15) | 1.1% | (8) | 106 | |
| 7C | 1.9% | (20) | 1.5% | (20) | 2.4% | (30) | 1.5% | (22) | 1.9% | (14) | 92 | |
| 34 | 2.0% | (21) | 1.0% | (13) | 1.1% | (14) | 1.2% | (17) | 1.1% | (8) | 73 | |
| 24F | 1.1% | (12) | 1.0% | (13) | 0.9% | (11) | 0.5% | (7) | 0.3% | (2) | 45 | |
| Other | 1.2% | (13) | 1.6% | (21) | 1.7% | (22) | 1.9% | (28) | 2.6% | (19) | 104 | |
| Total | (1054) | (1342) | (1274) | (1472) | (718) | 5860 | ||||||
Figure 6. Proportion of IPD isolates from 2016 to 2020 by vaccine, for 18 to 49 and 50 to 64 age groups
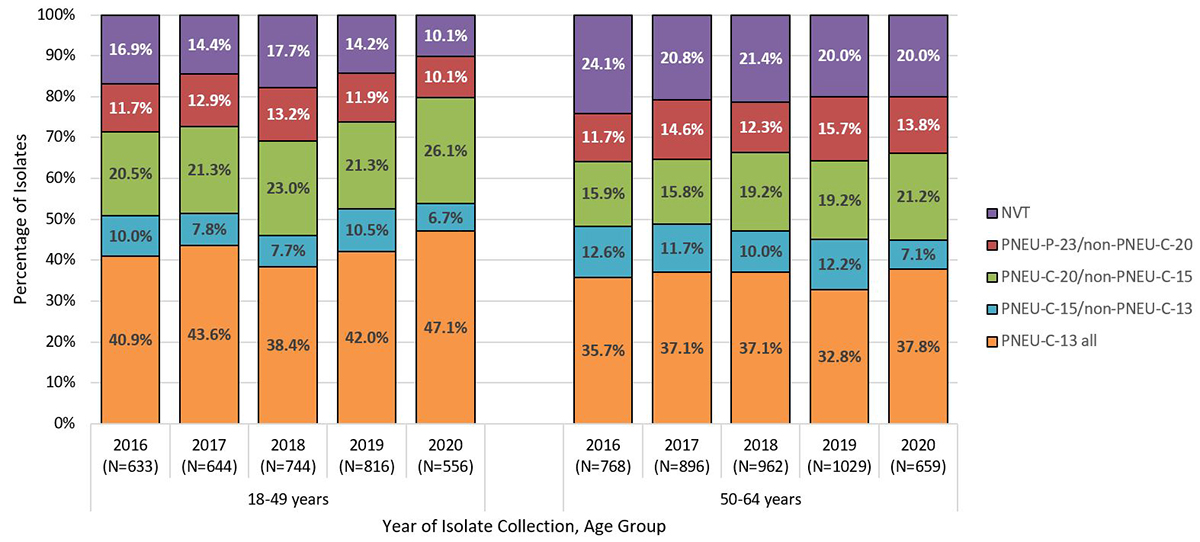
*Vaccine serotypes include PNEU-C-13 (1, 3, 4, 5, 6A/C, 6B, 7F, 9V, 14, 19A, 19F, 18C, 23F); PNEU-C-15 (all PNEU-C-13 plus 22F and 33F); PNEU-C-20 (All PNEU-C-15 plus 8, 10A, 11A, 12F, 15B/C) and PNEU-P-23 (PNEU-C-20 serotypes except 6A, plus 2, 9N, 17F, 20); NVT = all serotypes not included in PNEU-C-13, PNEU-C-15, PNEU-C-20 and PNEU-P-23. Serotype 6C included in PNEU-C-13 serotypes due to cross protection with 6A. Serotypes 15B and 15C were grouped together as 15B/C because of reported reversible switching between them in vivo during infection, making it difficult to precisely differentiate between the two types.
Text Description
Figure 6 shows a stacked bar graph displaying the percentage of Streptococcus pneumoniae collected from each vaccine category (PNEU-C-13, PNEU-C-15/non-PNEU-C-13, PNEU-C-20/non-PNEU-C-15, PNEU-P-23/non-PNEU-C-20 and other non-vaccine serotypes) for the 18 to 49 and 50 to 64 age groups, from 2016 to 2020.
| Age Group | Year | PNEU-C-13 (%, N) |
PNEU-C-15/ non-PNEU-C-13 (%, N) |
PNEU-C-20/ non-PNEU-C-15 (%, N) |
PNEU-P-23/ non-PNEU-C-20 (%, N) |
NVT (%, N) |
Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 18-49 years | 2016 | 40.9% | (259) | 10.0% | (63) | 20.5% | (130) | 11.7% | (74) | 16.9% | (107) | (657) |
| 2017 | 43.6% | (281) | 7.8% | (50) | 21.3% | (137) | 12.9% | (83) | 14.4% | (93) | (659) | |
| 2018 | 38.4% | (286) | 7.7% | (57) | 23.0% | (171) | 13.2% | (98) | 17.7% | (132) | (762) | |
| 2019 | 42.0% | (343) | 10.5% | (86) | 21.3% | (174) | 11.9% | (97) | 14.2% | (116) | (834) | |
| 2020 | 47.1% | (262) | 6.7% | (37) | 26.1% | (145) | 10.1% | (56) | 10.1% | (56) | (567) | |
| 50-64 years | 2016 | 35.7% | (274) | 12.6% | (97) | 15.9% | (122) | 11.7% | (90) | 24.1% | (185) | (768) |
| 2017 | 37.1% | (332) | 11.7% | (105) | 15.8% | (142) | 14.6% | (131) | 20.8% | (186) | (896) | |
| 2018 | 37.1% | (357) | 10.0% | (96) | 19.2% | (185) | 12.3% | (118) | 21.4% | (206) | (962) | |
| 2019 | 32.8% | (337) | 12.2% | (126) | 19.2% | (198) | 15.7% | (162) | 20.0% | (206) | (1029) | |
| 2020 | 37.8% | (249) | 7.1% | (47) | 21.2% | (140) | 13.8% | (91) | 20.0% | (132) | (659) | |
References
- Footnote 1
-
Warshawsky B, Gemmill I, Crowcroft N, Et. Al. An Advisory Committee Statement (ACS) National Advisory Committee on Immunization (NACI): Statement on the Use of Conjugate Pneumococcal Vaccine – 13 Valent in Adults (PNEU-C-13) [Internet]. Public Health Agency of Canada. 2013 [cited 2022 Jun 16]. Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2013-39/statement-on-use-conjugate-pneumococcal-vaccine-13-valent-adults-pneu-13.html
- Footnote 2
-
National Advisory Committee on Immunization (NACI). Update on the Use of 13-Valent Pneumococcal Conjugate Vaccine (PNEU-C-13) in Addition to 23-Valent Pneumococcal Polysaccharide Vaccine (PNEU-P-23) in Immunocompetent Adults 65 Years of Age and Older – Interim Recommendation [Internet]. Public Health Agency of Canada. 2016 [cited 2022 Jun 16]. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/update-use-of-13-valent-pneumococcal-conjugate-vaccine-pneu-c-13-in-addition-to-23-valent-pneumococcal-polysaccharide-vaccine-pneu-p-23-immunocompetent-adults-65-years-and-older-interim-recommendation.html
- Footnote 3
-
Kraicer-Melamed H, Baclic O, De Wals P, Et. Al. An Advisory Committee Statement (ACS) National Advisory Committee on Immunization (NACI): Update on the Use of Pneumococcal Vaccines in Adults 65 Years of Age and Older – A Public Health Perspective [Internet]. Public Health Agency of Canada. 2018 [cited 2022 Jun 16]. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/update-on-the-use-of-pneumococcal-vaccines-in-adult.html#a11
- Footnote 4
-
Guyatt G, Oxman A, Akl E, Et. Al. GRADE Guidelines: 1. Introduction-GRADE Evidence Profiles and Summary of Findings Tables. J Clin Epidemiol. 2011;64(4):383–94.
- Footnote 5
-
Balshem H, Helfand M, Schünemann H, Et. Al. GRADE Guidelines: 3. Rating the Quality of Evidence. J Clin Epidemiol. 2011;64(4):401–6.
- Footnote 6
-
Moher D, Shamseer L, Clarke M, Et. Al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst Rev. 2015;4(1):1.
- Footnote 7
-
Alonso-Coello P, Schünemann H, Moberg J, Et Al. GRADE Evidence to Decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016;353:i2016.
- Footnote 8
-
Public Health Agency of Canada. National Laboratory Surveillance of Invasive Streptococcal Disease in Canada – Annual Summary 2019 [Internet]. Government of Canada. 2021 [cited 2022 Jun 6]. Available from: https://www.canada.ca/en/public-health/services/publications/drugs-health-products/national-laboratory-surveillance-invasive-streptococcal-disease-canada-annual-summary-2019.html
- Footnote 9
-
Golden A, Griffith A, Demczuk W, Et. Al. Invasive Pneumococcal Disease Surveillance in Canada, 2020. Can Commun Dis Rep. 2022;48(9):396–406.
- Footnote 10
-
Cooper D, Yu X, Sidhu M, Et. Al. The 13-Valent Pneumococcal Conjugate Vaccine (PCV13) Elicits Cross-Functional Opsonophagocytic Killing Responses in Humans to Streptococcus pneumoniae Serotypes 6C and 7A. Vaccine. 2011;29(41):7201–11.
- Footnote 11
-
Venkateswaran P, Stanton N, Austrian R. Type Variation of Strains of Streptococcus pneumoniae in Capsular Serogroup 15. J Infect Dis. 1983;147(6):1041–54.
- Footnote 12
-
van Selm S, van Cann L, Kolkman M, Et. Al. Genetic basis for the structural difference between Streptococcus pneumoniae serotype 15B and 15C capsular polysaccharides. Infect Immun. 2003;71(11):6192–8.
- Footnote 13
-
Higgins J, Altman D, Gøtzsche P, Et. Al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
- Footnote 14
-
Shigayeva A, Chung H, Kwong J, Et. Al. Burden of Invasive Pneumococcal Disease among Adults with Underlying Chronic Conditions Post Implementation of PCV13 Immunization Programs in South Central Ontario Canada. Poster presented at: ISPPD 12. Toronto (ON): Mount Sinai Hospital; 2022.
- Footnote 15
-
Huang G, Martin I, Tsang R, Et. Al. Invasive Bacterial Diseases in Northern Canada, 1999 to 2018. Can Commun Dis Rep. 2021;47(11):491–9.
- Footnote 16
-
LeBlanc J, El Sherif M, Ye L, Et. Al. Recalibrated Estimates of Non-Bacteremic and Bacteremic Pneumococcal Community Acquired Pneumonia in Hospitalized Canadian Adults From 2010 to 2017 With Addition of an Extended Spectrum Serotype-Specific Urine Antigen Detection Assay. Vaccine. 2022;40(18):2635–46.
- Footnote 17
-
Shigayeva A, Rudnick W, Green K, Et. Al. Invasive Pneumococcal Disease Among Immunocompromised Persons: Implications for Vaccination Programs. Clin Infect Dis. 2016;62(2):139, 147.
- Footnote 18
-
Cabaj J, Nettel-Aguirre A, MacDonald J, Et. Al. Influence of Childhood Pneumococcal Conjugate Vaccines on Invasive Pneumococcal Disease in Adults With Underlying Comorbidities in Calgary, Alberta (2000-2013). Clin Infect Dis. 2016;62(12):1521–6.
- Footnote 19
-
Government of Canada. Vaccination Coverage Goals and Vaccine Preventable Disease Reduction Targets by 2025 [Internet]. 2022 [cited 2022 Jul 10]. Available from: https://www.canada.ca/en/public-health/services/immunization-vaccine-priorities/national-immunization-strategy/vaccination-coverage-goals-vaccine-preventable-diseases-reduction-targets-2025.html
- Footnote 20
-
Pfizer Canada. Product Monograph: PrevnarTM 13 Pneumococcal 13-valent Conjugate Vaccine (Diphtheria CRM197 Protein) [Internet]. 2019 [cited 2022 Jul 10]. Available from: https://pdf.hres.ca/dpd_pm/00052583.PDF
- Footnote 21
-
Merck Canada Inc. Product Monograph Including Patient Medication Information: Vaxneuvance® (Pneumococcal 15-Valent Conjugate Vaccine [Crm197 Protein], Adsorbed) [Internet]. 2021 [cited 2022 Jun 16]. Available from: https://pdf.hres.ca/dpd_pm/00063580.PDF
- Footnote 22
-
Pfizer Canada U. Product Monograph Including Patient Medication Information: Prevnar 20tm (Pneumococcal 20-Valent Conjugate Vaccine (Diphtheria Crm197 Protein)) [Internet]. 2022 [cited 2022 Jun 16]. Available from: https://pdf.hres.ca/dpd_pm/00065729.PDF
- Footnote 23
-
Merck Canada. Product Monograph: Pneumovax® 23 Pneumococcal Vaccine, Polyvalent, MSD Std. [Internet]. 2016 [cited 2022 Oct 24]. Available from: https://pdf.hres.ca/dpd_pm/00035855.PDF
- Footnote 24
-
Farrar J, Kobayashi M, Childs L, Et. Al. Systematic Review and Meta-Analysis of Pneumococcal Vaccine Effectiveness against Invasive Pneumococcal Disease among Adults. Open Forum Infectious Diseases. 2021;8(Supp 1):S134–5.
- Footnote 25
-
Childs L, Kobayashi M, Farrar J. The Efficacy and Effectiveness of Pneumococcal Vaccines against Pneumococcal Pneumonia among Adults: A Systematic Review and Meta-Analysis. Open Forum Infectious Diseases. 2021;8(Supp 1):S130–1.
- Footnote 26
-
Ermlich S, Andrews C, Folkerth S, Et. Al. Safety and Immunogenicity of 15-Valent Pneumococcal Conjugate Vaccine in Pneumococcal Vaccine-Naïve Adults ≥50 Years of Age. Vaccine. 2018;36(45):6875–82.
- Footnote 27
-
Peterson J, Stacey H, MacNair J, Et. Al. Safety and Immunogenicity of 15-Valent Pneumococcal Conjugate Vaccine Compared to 13-Valent Pneumococcal Conjugate Vaccine in Adults ≥65 Years of Age Previously Vaccinated with 23-Valent Pneumococcal Polysaccharide Vaccine. Hum Vaccin Immunother. 2019;15(3):540–8.
- Footnote 28
-
Platt H, Cardona J, Haranaka M, Et. Al. A phase 3 Trial of Safety, Tolerability, and Immunogenicity of V114, 15-Valent Pneumococcal Conjugate Vaccine, Compared with 13-Valent Pneumococcal Conjugate Vaccine in Adults 50 Years of Age and Older (PNEU-AGE). Vaccine. 2022;40(1):162–72.
- Footnote 29
-
Mohapi L, Pinedo Y, Osiyemi O, Et. Al. Safety and Immunogenicity of V114, a 15-Valent Pneumococcal Conjugate Vaccine, in Adults Living with HIV. AIDS. 2022;36(3):373–82.
- Footnote 30
-
Hammitt L, Quinn D, Janczewska E, Et. Al. Immunogenicity, Safety, and Tolerability of V114, a 15-Valent Pneumococcal Conjugate Vaccine, in Immunocompetent Adults Aged 18-49 Years With or Without Risk Factors for Pneumococcal Disease: A Randomized Phase 3 Trial (PNEU-DAY). Open Forum Infect Dis. 2021;9(3):ofab605.
- Footnote 31
-
Song JY, Chang C, Andrews C, Et. Al. Safety, Tolerability, and Immunogenicity of V114, a 15-Valent Pneumococcal Conjugate Vaccine, Followed by Sequential PPSV23 Vaccination in Healthy Adults Aged ≥50Yyears: A Randomized Phase III Trial (PNEU-PATH). Vaccine. 2021;39(43):6422–36.
- Footnote 32
-
Severance R, Schwartz H, Dagan R, Et. Al. Safety, tolerability, and immunogenicity of V114, a 15-valent pneumococcal conjugate vaccine, administered concomitantly with influenza vaccine in healthy adults aged ≥50 years: a randomized phase 3 trial (PNEU-FLU). Hum Vaccin Immunother. 2022;18(1):1–14.
- Footnote 33
-
Hurley D, Griffin C, Young M, Et. Al. Safety, Tolerability, and Immunogenicity of a 20-Valent Pneumococcal Conjugate Vaccine (PCV20) in Adults 60 to 64 Years of Age. Clin Infect Dis. 2021;73(7):e1489–97.
- Footnote 34
-
Essink B, Sabharwal C, Cannon K, Et. Al. Pivotal Phase 3 Randomized Clinical Trial of the Safety, Tolerability, and Immunogenicity of 20-Valent Pneumococcal Conjugate Vaccine in Adults 18 Years and Older. Clin Infect Dis. 2021;75(3):390–8.
- Footnote 35
-
Cannon K, Elder C, Young M, Et. Al. A Trial To Evaluate the Safety and Immunogenicity of a 20-Valent Pneumococcal Conjugate Vaccine in Populations of Adults ≥65 Years of Age with Different Prior Pneumococcal Vaccination. Vaccine. 2021;39(51):7494–502.
- Footnote 36
-
Bonten M, Huijts S, Bolkenbaas M, Et. Al. Polysaccharide Conjugate Vaccine Against Pneumococcal Pneumonia in Adults. N Engl J Med. 2015;372(12):1114–25.
- Footnote 37
-
Kobayashi M, Farrar J, Gierke R, Et. Al. Use of 15-Valent Pneumococcal Conjugate Vaccine Among U.S. Children: Updated Recommendations of the Advisory Committee on Immunization Practices — United States, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1174–81.
- Footnote 38
-
Cannon, Et. Al. Immunogenicity and Safety of a 20-Valent Pneumococcal Conjugate Vaccine (PCV20) Administered Concomitantly With a Quadrivalent Inactivated Influenza Vaccine in Adults Over 65 Years of Age. Poster Presented At: 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID). Lisbon (PT). 2022 Apr 23;
- Footnote 39
-
Fitz-Patrick, Et. Al. Safety, Tolerability, and Immunogenicity of BNT162b2 COVID-19 Vaccine Coadministered with 20-Valent Pneumococcal Conjugate Vaccine (PCV20) in Adults 65 Years of Age and Above. Poster Presented at: 32nd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID). Lisbon (PT). 2022 Apr 23;
- Footnote 40
-
Langley J. ARCHIVED - Canada Communicable Disease Report: Evidence-Based Recommendations for Immunization – Methods of the National Advisory Committee on Immunization [Internet]. Public Health Agency of Canada. 2009 [cited 2022 Jul 10]. Available from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2009-35/methods-national-advisory-committee-immunization.html
- Footnote 41
-
Matanock A, Lee G, Gierke R, Et. Al. Use of 13-Valent Pneumococcal Conjugate Vaccine and 23-Valent Pneumococcal Polysaccharide Vaccine Among Adults Aged ≥65 Years: Updated Recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2019;68(46):1069–75.