A Dementia Strategy for Canada: Together We Achieve - 2021 Annual Report
Download the alternative format
(PDF format, 5.1 MB, 72 pages)
Organization: Public Health Agency of Canada
Date published: 2022-01-20
Cat.: HP22-1E-PDF
ISSN: 2562-7805
Pub.: 210471
Table of contents
- Minister's message
- Introduction
- Canada's COVID-19 response and dementia
- Preventing dementia through risk reduction
- Applying research and innovation to dementia challenges
- Keeping quality of life at the forefront
- Focusing on those at higher risk and facing barriers to equitable care
- Conclusion
- Appendix: Aspirations for Canada's efforts on dementia from the national dementia strategy
- Bibliography
- Endnotes
Minister's message
Since the preparation of last year's annual report to Parliament on A Dementia Strategy for Canada: Together We Aspire, Canadians have weathered many months of uncertainty as the challenges created by the coronavirus (COVID-19) pandemic continued to evolve. There is no question that the pandemic has created additional significant challenges for people living with dementia and those close to them, particularly caregivers.
The 2021 report to Parliament on the national dementia strategy includes a chapter focused on responses to the pandemic relevant to dementia such as efforts undertaken to support caregivers and Canadians living in long-term care. It notes examples of the numerous organizations that pivoted in the wake of an unprecedented public health crisis to continue delivering services and programs that support Canadians. The report also provides several new data points relevant to the strategy's national objectives that help to document our collective progress towards the aspirations set out for each objective. It highlights a variety of dementia-related initiatives and shares thoughts from just a few of the many Canadians involved in the efforts taking place across the country.
The Government of Canada is taking action that goes beyond acknowledging that older Canadians have been among the most affected by the impacts of the COVID-19 pandemic. Many of those living in long-term care were forced into distressing isolation while thousands of lives were cut short. As of February 15, 2021, 69% of COVID-19 deaths were in long-term care facilities where often the majority of residents are living with dementia.Footnote 1 To further enable provinces and territories to provide a high standard of care in long-term care facilities, Budget 2021 provides a $3 billion investment over five years, starting in 2022-23, to help. The Government of Canada is also committed to helping seniors age well at home for as long as possible. Budget 2021 proposed new funding to design interventions that promote safe relationships and prevent family violence, including elder abuse, as well as to provide funding for mental health interventions for populations disproportionately impacted by COVID-19, including seniors.
The Government of Canada continues to invest in dementia-specific initiatives focused on raising awareness to reduce risk and stigma, enhancing data through surveillance, improving guidance, and supporting research, innovation, and community-based projects. Over the last year, the Public Health Agency of Canada (PHAC) has funded and launched 16 new projects to support the national dementia strategy, with more to be announced in 2021.
Our ability to assess progress on the strategy's national objectives is tied to our capacity to monitor the state of dementia in Canada and its impact over time. The 2021 report almost doubles the number of data points compared to last year's report. It dives deeper into the results of PHAC's 2020 dementia baseline public opinion research, sharing responses from some of the populations identified as likely to be facing higher risks of developing dementia and / or facing barriers to care. Efforts on dementia need to consider how best to reach and support these populations so that we can move closer to health equity.
I want to express my deep appreciation for all those who have continued to make exceptional contributions towards the national objectives of Canada's dementia strategy, despite the challenges of the pandemic. These collective efforts are helping to advance our essential work on dementia.
The Honourable Jean-Yves Duclos
Minister of Health
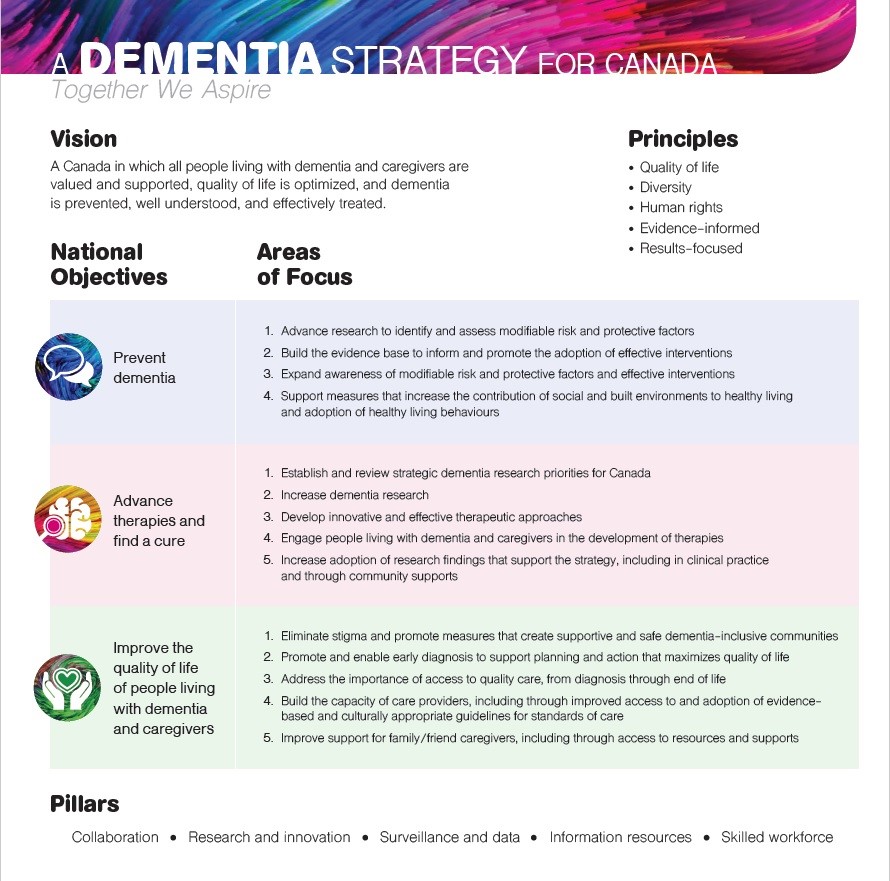
Figure 1: Text equivalent
A Dementia Strategy for Canada: Together We Aspire
Vision: a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated.
Principles:
- Quality of life
- Diversity
- Human rights
- Evidence-informed
- Results-focused
| National objectives | Areas of focus |
|---|---|
| Prevent dementia |
|
| Advance therapies and find a cure |
|
| Improve the quality of life of people living with dementia and caregivers |
|
Pillars:
- Collaboration
- Research and innovation
- Surveillance and data
- Information resources
- Skilled workforce
Introduction
For many Canadians living with dementia and those supporting them, the past year has been exceptionally difficult.Footnote 2 Prolonged periods of isolation resulting from the COVID-19 pandemic have contributed to mental health issues and caregiver stress. Social distancing and other public health requirements prevented caregivers from visiting long-term care facilities, and caused disruptions to available supports and services for both caregivers and people living with dementia. Some caregivers report that the long periods of separation and reduced social interaction appear to have hastened cognitive decline and reduced quality of life among people living with dementia. Tragically, in the initial months of the pandemic when many of the reported COVID-19-related deaths were among older Canadians, 80% of those deaths took place in long-term care facilities and retirement homes, where the majority of residents are those living with dementia.Footnote 3
This year's report includes a COVID-19 section that touches on some of the responses across Canada assisting people living with dementia and caregivers who continue to face the daily challenges created by the pandemic. Many initiatives were launched or adapted including: guidance to provide timely, safe and supportive care within long-term care facilities in the context of the pandemic; increased resources for organizations providing critical assistance to those in need; and new uses of technology to continue to reach individuals while adhering to public health guidance. Organizations often found ways to maintain programming and services for people living with dementia and caregivers, although some were forced to postpone or cancel activities.
The 2021 annual report to Parliament on Canada's national dementia strategy, A Dementia Strategy for Canada: Together We Aspire, shares with Canadians a variety of dementia-related efforts conducted by many different organizations across the country. Some of these initiatives focus on furthering dementia prevention through risk reduction by supporting healthy aging and built environments that encourage social contact and physical activity. Other initiatives emphasize the need to advance alternative dementia therapies to support quality of life, including through the use of innovative technologies, while work continues to find a cure. Efforts to promote the quality of life and wellbeing of people living with dementia and caregivers include those that highlight the importance of supporting intergenerational connections, improving navigation of community supports and the health care system, and promoting continued education for health and care providers.
The report once again shares selected data points to provide a snapshot of the state of dementia in Canada and insight on collective progress on the aspirations embedded in the strategy's national objectives. The number of data points in this year's report has nearly doubled from last year. Topics for the data points include stigma, caregiver distress, knowledge of Canadians about reducing the risk of dementia, quality of life in long-term care, as well as trainees engaged in dementia-related work funded by the Canadian Institutes of Health Research (CIHR).
Some populations within Canada have been identified as more likely to face barriers to equitable care and/or are at higher risk of developing dementia. A chapter focused on these populations notes some relevant initiatives such as work focused on the experiences of transgender and non-binary adults living with dementia, dementia-related stigma in Indigenous communities, and providing training to care providers in rural and remote communities on person-centred approaches. The 2021 report also includes informative data relevant to some of these priority populations. Survey responses to a 2020 dementia baseline survey commissioned by the Public Health Agency of Canada (PHAC) related to prevention, stigma and dementia-inclusive communities are shared this year for three priority populations – Indigenous peoples, ethnic populations and rural and remote communities.
What is dementia?
Dementia is a term used to describe symptoms affecting brain function. It may be characterized by a decline in cognitive (thinking) abilities such as: memory; planning; judgement; basic math skills; and awareness of person, place and time. Dementia can also affect language, mood and behaviour, and the ability to maintain activities of daily living. Dementia is not an inevitable part of aging.
Dementia is a chronic and progressive condition that may be caused by neurodegenerative diseases (affecting nerve cells in the brain), vascular diseases (affecting blood vessels like arteries and veins) or injuries. Types of dementia include vascular, Lewy body, frontotemporal, Alzheimer's disease and mixed (a combination of more than one type). In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease.Footnote 4
Key investments by the Public Health Agency of Canada
Beyond monitoring the implementation of the broad scope of the national dementia strategy, PHAC continues to support implementation of elements of the strategy that fall within its mandate. Investments are being made in enhanced surveillance, community-based projects, improved dementia guidance and evidence-based public education and awareness raising activities that aim to prevent dementia, reduce stigma, and enable dementia-inclusive communities. To ensure that the perspectives of those with lived experience are included, people living with dementia and caregivers are meaningfully engaged and included in all initiatives supported through PHAC's work.
Dementia Strategic Fund
The Dementia Strategic Fund supports efforts to further progress on two of the strategy's national objectives, prevention and quality of life, through the creation of a national public education/awareness campaign and targeted awareness raising activities, improvements to dementia guidance such as guidelines and best practices, and the creation of a comprehensive online dementia portal to share information resources.
National awareness campaign
PHAC will be implementing a national public awareness campaign to generate awareness and educate Canadians about dementia, risks and stigma. Public education efforts include a multimedia ad campaign that is expected to be launched in 2022 and will use various media tactics such as social media, digital banners and videos, digital billboards and print. Other outreach activities include a digital influencer campaign, a video series focusing on people living with dementia and a proactive media tour with two well-known spokespeople who will help amplify the messages of the campaign by sharing their own lived experiences with dementia.
François Morency is a French-Canadian comedian, actor, author and television host. He currently stars in a hit TV show that is largely based on his relationship with his parents and is watched by millions. He recently lost his mother. She was 92 and had dementia.
Jay Ingram is an author, broadcaster and science communicator. He has written many books, including The End of Memory: A Natural History of Alzheimer's and Aging, which is based on his personal and professional observations of the impact of dementia.
In early 2021, news articles, a video, and a radio spot about risk reduction, healthy lifestyle behaviours and how to help people living with dementia were produced and made available to media outlets. Between January and May 2021, this content was picked up 139 times and integrated into local and national media channels with an estimated reach of 9.7 million impressions across Canada.
Targeted awareness raising activities
PHAC is funding organizations to put in place awareness raising projects across the country aimed at reducing the risk of developing dementia, reducing stigma and encouraging communities to be more dementia inclusive. These two-year projects, launched in 2021, are based on a clear evidence base supporting the need for and approach to the work. Projects were encouraged to address health equity, such as focusing on populations identified as being likely to be at higher risk of developing dementia and/or facing barriers to equitable dementia care.
Dementia guidance
Through the Dementia Guidelines and Best Practices Initiative, PHAC supports efforts intended to improve access to and use of guidance relevant to dementia such as guidelines, tools and best practices. Dementia guidance is often obtained through online resources, print materials, and person-to-person consultations and interactions.
This work has three phases, with the first two phases focused on better understanding the needs and priorities for dementia guidance in Canada. Guidance on prevention, screening and early diagnosis, treatment and management, stigma reduction, dementia-inclusive communities, and emergency preparedness was the focus of these first two phases. The results of this initial work is helping to inform a Phase III funding opportunity, anticipated to be launched in 2021-22.
Phase I has produced an assessment of the quality of relevant dementia guidance available in Canada and abroad to gain a thorough understanding of the quality of the methodology used to develop this guidance, and identify gaps. A 17-member expert panel brought together the perspectives, expertise and experiences of people living with dementia, dementia advocates, family caregivers, researchers, personal support workers, government employees, and health professionals and provided feedback at key stages. The project examined guidance related to 23 priority research questions such as effective ways to manage the transition between different care settings, stigma reduction, and dementia screening. The initial scan located 1720 documents, with 242 guidance documents selected for assessment to support recommendations on whether the guidance documents are ready to consider for use as is, or would first require updating or adaptation to the Canadian context.
Overview of some key gaps in dementia guidance identified through Phase I
- Diagnosis: key considerations when delivering a dementia diagnosis to an individual and their support network
- Treatment and management: key considerations for pharmacological and non-pharmacological dementia management strategies when other chronic conditions are present; transitions in care; effective management strategies during palliative or end of life care
- Stigma reduction: training and education for care providers
- Dementia-inclusive communities: physical accessibility; navigation assistance
- Emergency preparedness and response: supporting people living with dementia during events such as fires, floods, earthquakes and pandemics
- Culturally-appropriate guidance: resources tailored to the cultural context of populations, including those that may be at higher risk of developing dementia and/or face barriers to care such as Indigenous peoples, ethnic and cultural minority communities, official language minority communities, and LGBTQ2 individuals.
Phase II focused on consultations with guidance users to better understand use and uptake, including barriers to obtaining or using dementia guidance. An online questionnaire gathered 248 responses across Canada from dementia guidance users and those familiar with this guidance, including: people living with dementia, caregivers, health care professionals, researchers, personal support workers, and government officials supporting dementia-related services and activities. In-depth follow up discussions were also conducted through 13 virtual roundtable discussions (total of 63 participants) and 31 virtual one-on-one informant interviews.
"As a caregiver, I have had difficulty finding high quality and relevant dementia guidance informed not only by those dealing directly with the condition, but by other key stakeholders. For me, I think it is particularly important that more work is done when it comes to effectively communicating with people living with dementia and caregivers upon diagnosis. I found the assessment of dementia guidance available to Canadians led by Optimus SBR on behalf of PHAC to be very thorough. This first phase of PHAC's Dementia Guidelines and Best Practices Initiative benefitted from the feedback informed by the broad experiences of expert panelists, resulting in a well-documented identification and assessment of dementia guidance." – Paul Blanchet, Caregiver
Dementia Community Investment
The Dementia Community Investment (DCI) funds community-based projects that are developing, testing and scaling-up resources, information, and programs to improve the wellbeing of people living with dementia and family/friend caregivers and to increase knowledge about dementia and its risk and protective factors. All projects funded by the DCI are required to undertake intervention research to assess the effectiveness of the initiative and have knowledge transfer and sustainability plans to help mobilize and share results. The DCI currently funds 19 projects, which include a wide-range of projects such as the development and testing of a National Dementia-Friendly Toolkit to help educate and train diverse sector professionals (e.g. transportation, recreation, library), and development of culturally appropriate resources for family/friend caregivers in select Inuit communities.
Knowledge hub spotlight
A knowledge hub, led by the Schlegel-University of Waterloo Research Institute for Aging (RIA), is facilitating a community of practice for all DCI projects to enable them to build capacity, amplify findings, learn from each other and support collaboration. The knowledge hub will be guided by a community advisory committee, which includes people living with dementia and family/friend caregivers, to ensure that lived experience is integrated into its work.
The knowledge hub is currently engaged in building the community of practice through information sharing and identifying opportunities for learning and collaboration. This will be enhanced through the development of a website which will showcase DCI projects and resources.
The knowledge hub will also mobilize key findings from individual projects and broader lessons learned to inform dementia policy and programming across Canada. Building these connections will help ensure DCI investments can benefit more Canadians living with dementia, family/friend caregivers, and the communities in which they live.
Enhanced Dementia Surveillance Initiative
The Enhanced Dementia Surveillance Initiative funds projects that support the surveillance and data pillar of the national dementia strategy. It advances the overarching goal of the strategy to improve the national surveillance of dementia, leading to better data to inform prevention, supportive care and health care related to the condition. Nine projects are underway to better understand how dementia affects Canadians. Through collaboration between PHAC, provincial and federal partners, as well as other stakeholders, new approaches are being explored and designed to collect data on topics such as undiagnosed dementia, co-occurrence of dementia and other chronic conditions and diseases, and dementia in long-term care settings. Of these nine projects, this report highlights three projects supporting the national objective to prevent dementia, and four projects supporting the national objective to improve the quality of life for people living with dementia and caregivers.
In addition to these investments, PHAC also provides leadership and promotes collaboration on dementia. PHAC serves as the secretariat to the Ministerial Advisory Board on Dementia, which provides the Minister of Health with expert advice, including from those with lived experience. To facilitate coordinated action across the country, PHAC co-chairs the Federal, Provincial, and Territorial Coordinating Committee on Dementia which facilitates information sharing and collaboration across Canada. PHAC also supports federal collaboration on dementia by chairing the Interdepartmental Coordinating Committee on Dementia, with members from 13 federal departments. In addition to PHAC, many federal departments contribute to the objectives of the national dementia strategy, including Employment and Social Development Canada, the Department of Justice, and the Canada Revenue Agency.
Dementia by the numbers
- As of 2017-18, almost 452,000 Canadians 65+ or older (6.7% of all Canadians 65+) were living with diagnosed dementia (data pending release)
- Two-thirds of people diagnosed with dementia are women
- About 1 in 4 Canadians age 85+ are living with diagnosed dementia
- Approximately 3% of Canadians living with dementia are younger than age 65
- 9 Canadians age 65+ are diagnosed with dementia every hour
- About 61% of Canadians age 65+ with dementia live outside of publicly funded long-term care and nursing homes
- The all-cause mortality rate (the rate of death due to any cause) in Canadians age 65+ with diagnosed dementia is 4.4 times higher than that of those without diagnosed dementia
Canada's COVID-19 response and dementia
Statistics Canada reported that between January 2020 and February 2021, dementia was listed as a pre-existing condition on the death certificate of 41% of the women and 31% of the men who died due to COVID-19, higher than any other pre-existing condition.Footnote 5 Based on available evidence, it appears that people living with dementia face a higher risk of severe symptoms and outcomes as a result of a COVID-19 infection. A possible link between having had a COVID-19 infection and neurological issues is being explored.
Among the many efforts undertaken across Canada to reduce the impacts of the pandemic, some are particularly relevant to people living with dementia and caregivers. Several of the responses highlighted here focus on long-term care where unprecedented challenges were experienced. These challenges drew national attention to the need to improve the ability to provide a safe environment in a pandemic situation while finding a way to limit isolation and separation from loved ones, which has its own negative effects. Other measures include additional financial and other supports and pivoting to alternate ways to continue initiatives.
"The COVID-19 pandemic has strongly impacted those living with dementia, as well as their families and caregivers. It has exposed critical gaps in dementia care across our health and long-term care systems. At the same time, it has also prompted some inspiring examples of organizations and individuals who have successfully navigated pandemic-related challenges by exploring innovative approaches and adapting existing dementia care programs and services. We must continue to work together to enable sustainable and adaptable solutions that support the health and wellbeing of people living with dementia and their families and caregivers" – Theresa Tam, Chief Public Health Officer of Canada
Supporting those living in long-term care
As the COVID-19 pandemic continued into 2021, it became increasingly clear that people living with dementia and those who care for them have been disproportionately affected. Up until the end of May 2020, 80% of COVID-19 related deaths took place in long-term care facilities and retirement homes, where the majority of residents (69% as of 2015-16) are those living with dementia.Footnote 3,Footnote 6 The pandemic has also highlighted challenges faced by care providers. For example, personal support workers in long-term care homes have been identified as facing economic and employment insecurity, a lack of paid sick leave, and the need to work multiple jobs to make ends meet. These challenges may have contributed to increased virus transmission during the pandemic while jeopardizing the health of these workers.
A McMaster University research team has developed a new long-term care palliative toolkit to address immediate needs within long-term care homes in response to COVID-19, helping to support those living with dementia and their families who are seeking palliative resources. The toolkit includes online instructional videos as guides, as well as advance care planning and bereavement pamphlets, and a booklet on comfort care at end of life. In the absence of palliative supports, individuals and families may need to make critical and emotional end-of-life decisions without prior discussions, which can result in additional stress and conflict.
Given the impact of COVID-19 on those living and working in long-term care settings, PHAC worked with subject matter experts to develop recommendations to better protect Canadians. Guidance on infection prevention and control for COVID-19 for long-term care homes, released in April 2020, updated in February 2021 and again in May 2021, includes infection prevention and control to minimize COVID-19 infections in staff and residents of long term care. Guidance is reviewed as new evidence becomes available, and advice is updated where relevant.
Interim guidance on the care of residents in long-term care homes during the COVID-19 pandemic was released in July 2020 and in place until April 2021 to support the timely, safe and supportive care of residents with suspected or confirmed COVID-19. Reflecting the fact that in many long-term care homes, the majority of residents are living with dementia and the elevated risk of COVID-19 related deaths linked to people living with dementia, some of the recommendations were specific to dementia. For example, the guidelines recommended updating resident care plans to identify residents with more advanced dementia and/or responsive behaviours who may need a more tailored approach to care. The guidance also included advice for managing responsive behaviours that may occur among people living with dementia when faced with changes to their routine and environment that they do not understand. The document has been archived as of April 2021, as there are professional societies, long-term care homes and provincial bodies posting more up-to-date clinical guidance.
The National Advisory Committee on Immunization (NACI) is an external committee that provides independent advice to PHAC on the optimal use of vaccines authorized for use in Canada. In NACI's Guidance on the prioritization of key populations for COVID-19 immunization, key populations were sequenced in three stages corresponding to increasing vaccine availability in each quarter of 2021. Stage 1 prioritized residents and staff of congregate living settings that provide care for seniors, adults 70 years of age and older, beginning with adults 80 years of age and older, as well as health care workers (all who work in health care settings and personal support workers whose work involves direct contact with patients). Stage 2 prioritized those aged 60+, and Stage 3 those aged 16-59 at high risk of severe illness and death from COVID-19. Dementia is also listed among the chronic medical conditions that place people at risk of more severe disease or outcomes from COVID-19.
Simple, evidence-based strategies can be used to avoid vaccine experiences that are stressful, uncomfortable, and sometimes painful. To help long-term care homes and retirement homes roll out COVID-19 vaccines to residents, immunization experts from across the country have made vaccine tools and instructions readily available, such as Resources to Assess Pain and Support a Positive Vaccine Experience in Older Adults with Cognitive Impairments During COVID-19 Vaccination.
Looking longer term, significant efforts are being made to ensure that seniors and those in care live in safe and dignified conditions. Budget 2021 announced a $3 billion investment to Health Canada to support provinces and territories in ensuring standards for long-term care are applied and permanent changes are made. To keep seniors safe and improve their quality of life, the federal government will work collaboratively with provinces and territories, while respecting their jurisdiction over health care, including long-term care. Recognizing the need to ensure relevant guidance is available to support people living with dementia during emergency situations such as pandemics, PHAC has included this topic in its review of the availability and use of dementia guidance. Public opinion research projects related to dementia conducted over the last year have also included questions about the impact of COVID-19 on people living with dementia and care providers. The insights gleaned from this information gathering and analysis will help to advance future efforts.
Pivoting to continue programs and services
Organizations delivering programs and services to people living with dementia faced significant challenges during the pandemic, having to adapt quickly to physical distancing measures and other local COVID-19 public health requirements and restrictions. In some cases, programs and services had to be postponed or cancelled, causing disruption to routines, while some organizations found new ways to continue their work and deliver programming and services. The loss of in-person day programs and respite care, among other supports and activities, also created increased stress and exhaustion among both people living with dementia and caregivers.
A research team at the University of Saskatchewan has created virtual socialization hubs through videoconferencing software that are inclusive and accessible. These hubs act as a safe spot for older adults, including those living with dementia and caregivers, to create friendships and minimize feelings of isolation. While these hubs have reduced isolation through the use of remote training, barriers to technology adoption encountered are being further explored.
The team is using this technology to help community partners such as the Saskatoon Council on Aging and the Alzheimer Society of Saskatchewan maintain programming and social activities. The mental health of older adults across the province is also being monitored regularly. The aim is to recruit participants who would not otherwise reach out for help, and to be able to provide interventions earlier to those who need them.
Prolonged periods spent at home can contribute to mental health issues and caregiver stress. According to the 2020 Global Carer Wellbeing Index, 70% of caregivers in Canada say the pandemic has worsened their emotional/mental health, compared with an average of 61% in 12 other countries.Footnote 7 In addition, an Alberta study examining the impact of the COVID-19 pandemic suggests that caregivers feel overburdened, are struggling with isolation, need greater support, and are experiencing a significant increase in caregiving responsibility, while people living with dementia are showing an increased decline in wellness and function as a result of pandemic-related public health measures.Footnote 8,Footnote 9
In 2021, PHAC conducted public opinion research on the quality of life of people living with dementia where all respondents were people living with dementia or caregivers. Preliminary results indicate that, with the exception of the disruption of certain services (see below), the perceived impact of the COVID-19 pandemic on the lives of people living with dementia was found to be much the same as anyone else in Canada.Footnote 10 For caregivers who experienced restrictions on visits (54%) and the loss of activities for people living with dementia such as adult day programs (49%), isolation, sadness, and anxiety were often reported as the most challenging of pandemic effects. Other challenges included cancellation or reduction of support services, such as home care (39%) and wearing personal protective equipment while interacting with people living with dementia (24%).
In PHAC's 2021 public opinion research, care providers (i.e. health care professionals, caregivers, developmental service workers, personal support workers, first responders) were asked to identify the challenges they faced while providing care to people living with dementia during the pandemic.Footnote 11 The preliminary results indicate the following key challenges: lack of staff; migration of services to virtual care platforms; lack of information, guidance and training on how to safely perform care duties; crowded and shared spaces, which can occur in group or assisted living; staff working in multiple settings; infection control; and the availability of personal protective equipment. Suggested solutions include: adding more front line staff; increasing pay to attract and retain staff; reducing work in multiple locations; maintaining access to referrals, experts, and programs and better planning to ensure these supports remain available; access to more and better personal protective equipment; and access to clear and consistent information about safety protocols and management of the crisis. Some respondents highlighted the need for dementia guidance, tools and other resources related to emergency preparedness and response.
To help Canadians cope with changes resulting from pandemic-related public health measures, the Government of Canada's $350 million Emergency Community Support Fund supports community organizations to expand home deliveries of groceries or medication, transport seniors or people with disabilities to appointments, and replace in-person, one-on-one contact with contact through phone calls, texts or the Internet. As well, through Budget 2021, $90 million over three years, will support a new Age Well at Home initiative that will help community-based organizations support low-income and otherwise at-risk seniors age in place by, for example, matching seniors with volunteers who can help with meal preparation, home maintenance, daily errands, yard work, and transportation. Budget 2021 also announced funding of $100 million over three years, starting in 2021-22, for innovative mental health interventions for populations disproportionately impacted by COVID-19, including health care workers, front-line workers, youth, seniors, Indigenous peoples, and racialized and Black Canadians.
Other measures were put in place by the Government of Canada are available to help Canadians who needed to stay home from work as a result of COVID-19 to provide caregiving, such as care for those living with dementia. The Canada Recovery Caregiving Benefit provides $500 a week for up to 42 weeks to employed and self-employed individuals who have been unable to work due to COVID-19 because they must care for a child under 12 years old or a family member who needs supervised care.
The My Parkgate BREAK program, offered by the Parkgate Community Services Society in British Columbia, provides activities to encourage social interaction, respite and exercise for members living with dementia and their families. As one example of the many programs adjusting to public health guidance, the program moved from three weekly in-person programs to virtual programming supported primarily by YouTube content, with added telephone support and a weekly Zoom call for members, caregivers and volunteers to maintain social connectedness. My Parkgate BREAK was able to add an outdoor in-person program in summer 2020 and moved the program indoors with additional safety precautions in the fall. The organization closed temporarily in winter to reconfirm safety protocols with Vancouver Coastal Health and was able to resume a longer, twice weekly indoor in-person program with additional members.
Some organizations were able to embrace technology to deliver programming in new ways, adapting quickly to online platforms and adjusting activities as restrictions lifted. Use of newer technologies mixed with more traditional methods (such as telephone support) helped to reduce social isolation for people living with dementia and caregivers, offering respite and opportunities for physical activity.
Music Share is a non-profit organization incubated at Ryerson University's Social Ventures Zone. The flagship program connects youth volunteers with isolated seniors living in long-term care communities for one-to-one music listening experiences, helping to stimulate the brain, trigger memories, and form new meaningful connections. In response to the pandemic, Music Share developed a variety of socially distanced programs for long-term care communities in the GTA. This included delivering iPads loaded with personalized playlists to residents of long-term care homes, as well as connecting residents with program facilitators for one-to-one music listening sessions via Zoom video calls. The focus on familiar music, personalization, and face-to-face social interaction sets Music Share apart from other programs currently offered. Similarly, the Alzheimer Society of Thunder Bay is providing iPads to people living with dementia and caregivers to support social inclusion through an arts-based program that encourages participants to explore their creative voice and share observations with others.
Other organizations offered new content during the pandemic, such as the "What Connects Us" project in partnership with the Alzheimer Society of Montreal, which provides opportunities for people with Alzheimer's disease and other forms of neurocognitive conditions and caregivers to participate in activities via Zoom. People living with these conditions and caregivers were able to explore new and exciting activities, helping them to maintain their wellbeing while remaining active and engaged.
"What Connects Us" activities introduced in 2020 included:
- Revisiting Expo 67, a multi-sensory approach to relive Expo 67 including sound, images, and discussion
- Creative dance with Les Grands Ballets Canadiens, a creative dance and movement workshop for people living with mild Alzheimer's disease and other neurocognitive conditions and caregivers
- A weekly hour of Laughter Yoga via Zoom
"The adapted creative dance workshop is always an experience that is greatly appreciated by all participants: caregivers and people living with dementia alike. Fun, spontaneity, laughter, a child's heart, and joy are ever-present during the classes!!" – Generosa De Cubellis, Counsellor, Counselling Network – East of Montreal, Alzheimer Society of Montreal [Translation]
In Alberta, 14 projects to build innovative approaches to person-centred dementia services under the Alberta Health Services' Community-based Innovations for Dementia Care initiative have been able to creatively overcome obstacles presented by the COVID-19 pandemic. Community and health service providers leading these projects have adapted their work to changing restrictions, leveraging virtual technology to hold focus groups, education sessions and support groups. The ability to respond quickly to adapt and develop innovative approaches has meant that needs related to social isolation, food security, loneliness, grief, transportation and information-sharing are able to be addressed for Albertans affected by dementia.
Arts-based programs can provide cognitive stimulation for people living with dementia, helping to promote and maintain creativity and self-expression, as well as offering purpose and a sense of connection through meaningful activities that offer opportunities to socialize. Sometimes these activities connect seniors with youth to encourage conversation and relationship-building, which can also help to combat ageism and stigma. Organizations have adapted in-person programming during the pandemic to offer a wide variety of creative activities (such as drawing, painting, colouring, woodwork, ceramics, and music appreciation) on virtual platforms, with material downloaded onto mobile devices or delivered through Zoom, art kits delivered by mail to individuals, and in some cases engaging staff working in long-term care and retirement homes to help facilitate activities.
In another form of pivoting, the COVID pandemic has accelerated the clinical adoption of virtual care software across Canada. Research on the barriers and effectiveness of virtual approaches to care is increasing. While initial findings published in the Canadian Medical Association Journal suggest that cognitive assessment tools administered virtually are generally reliable, implementing a system for assessing and managing dementia is feasible, and virtual care platforms have been generally well accepted, there are still some unanswered questions about the appropriateness of virtual care as dementia progresses and the impact on health outcomes.Footnote 12 Important accessibility barriers resulting from virtual care are also being identified for those with cognitive impairment, as well as the elderly, and other vulnerable populations. As a result, when possible, virtual visits are suggested as a supplement to in-person encounters instead of a replacement.
The National Research Council of Canada is working with the Ontario College of Art & Design (OCAD) University's Inclusive Design Research Centre to develop a guide for reducing barriers to virtual health care that includes exploring how software can allow the same personal preferences to be captured and applied across different virtual health care systems, such as preferred timing for appointments and font sizes. This will help support efforts to ensure that virtual healthcare is able to meet the diverse needs of those who may be overlooked in standard design practices, including people living with dementia.
The COVID-19 pandemic has created transportation challenges for Canadians, particularly those with disabilities. Transport Canada is working with the National Research Council and the Canadian Transportation Agency to produce a research report on the impacts of COVID-19 on persons living with disabilities, including those with dementia, when using the federal Canadian transportation system. This collaboration has resulted in expert guidance released in February 2021 that sets out best practices for transportation service providers, as well as travel tips for persons with disabilities during COVID-19, such as bringing your own hand sanitizer and making sure the transportation service provider is aware of your needs.
Government of Canada efforts to support people living with dementia and caregivers during COVID-19 will continue. PHAC is monitoring where the disease is most active, where it is spreading and how it is impacting the health of Canadians to help inform future action.
Health impacts of COVID-19 and dementia
Dementia has been identified as one of several risk factors for susceptibility to COVID-19 infection and more serious symptoms and outcomes, though the reason for the association with increased risk is not yet clear. Some suggest that the higher risk of infection with COVID-19 among people living with dementia may be related to advanced age and frequent exposure to care providers (such as personal support workers), as well as the high proportion of people living with dementia in congregate living situations such as long-term care. People living with dementia may experience greater challenges that increase risk for COVID infections, such as those related to maintaining hygiene and other preventative health measures. Research also suggests that having dementia may be a more predominant risk factor than advanced age for developing severe COVID-19 and/or death. As well, researchers are exploring a possible link between infection with COVID-19 and subsequent cognitive impairment, as well as the impacts of physical distancing and other public health measures on the rate of cognitive decline in those with existing cognitive impairment.
The Centre de formation médicale du Nouveau-Brunswick in Moncton is researching long-term cognitive consequences after infection with COVID-19. This national and international 12-month project began in November 2020. Neuropsychological assessment and general health questionnaires provided to more than 150 people infected more than three months prior will enable efforts to set up screening and rehabilitation strategies intended to reduce the long-term cognitive consequences of COVID-19.
Recognizing the significant impact of the pandemic on those living with dementia and those supporting them, the Alzheimer Society of Canada, in collaboration with the Canadian Consortium on Neurodegeneration in Aging, the College of Family Physicians of Canada, the Canadian Geriatrics Society and others, worked quickly to convene a COVID-19 and Dementia Task Force in May 2020. The task force examined key gaps exposed by the pandemic impacting people living with dementia and how to improve care in the context of a pandemic including: reducing stigma and discrimination against people living with dementia; identifying the health system changes experienced; evaluating the delivery of virtual care; understanding the impact of the pandemic on people with dementia in long-term care; and promoting quality of life for long-term care residents through a health crisis.
The Alzheimer Society of Canada COVID-19 and Dementia Task Force developed several resources for health professionals, as well as policy and decision makers, including:
- Guidelines for acute care on allocating scarce resources to people with dementia during a pandemic
- Recommendations for family physicians providing remote cognitive and behavioral assessments
- Recommendations for improving end of life care for people with dementia in long-term care homes during the pandemic
- Information about research that is being undertaken to understand gaps in the use of the health care system for people with dementia during the pandemic and the number of people with dementia who died due to COVID-19
- An article that explores the devaluation of nursing home staff during COVID-19 and potential implications for the next health care crisis
- A commentary on social connection as essential in long-term care homes, including guiding principles to enable social connection and promote health and quality of life for long-term care residents during COVID-19 and beyond
"People living with dementia have been impacted immensely by the COVID-19 pandemic. The work of the Alzheimer Society of Canada's COVID-19 and Dementia Task Force is dedicated to improving care and protections for people living with dementia now, while creating sustainable health system change that will take us well beyond the COVID-19 context." – Saskia Sivananthan, Chief Science Officer, Alzheimer Society of Canada
Spotlight: Highlights of Canada's dementia-related research response to the COVID-19 pandemic
The Canadian research community has mobilized to respond rapidly to the COVID-19 pandemic across all health research areas, including dementia-related research. Recognizing the unprecedented challenges experienced by Canadians living with dementia and caregivers during the pandemic, the Government of Canada, through the Canadian Institutes of Health Research (CIHR), continues to support innovative dementia research in Canada, including emergent research priorities associated with COVID-19. Highlights include:
Understanding the short- and long-term impact of COVID-19 on brain health using the CLSA
The Canadian Longitudinal Study on Aging (CLSA) is a large, national, long-term study that collects a range of health-related data on approximately 50,000 individuals over approximately 20 years; individuals were between the ages of 45 and 85 years when recruited into the study in 2009. This existing research platform was leveraged to address evidence needs presented by the COVID-19 pandemic.
As severe illness due to COVID-19 most often occurs in older adults, with about 18% of the Canadian population aged 65 years or older, understanding the long-term impacts of COVID-19 on older adults is critical. To address this research evidence gap, PHAC, in close collaboration with CIHR, supported the creation of a COVID-19 Data Module within the CLSA to collect COVID-19-specific data from participants. Researchers will use these data to assess the acute issues and the long-term impacts of the pandemic on older Canadians, including on some key health indicators, such as mental health and chronic disease risks. With these data, Canadian researchers will be better positioned to provide the evidence required to inform public health strategies to mitigate the short- and longer-term health impacts of COVID-19.
Further, there is evidence that COVID-19 can affect the brain and central nervous system in the short term; however, further research is needed to understand the longer-term implications of COVID-19 and its impact on brain health, including its potential to increase the risk of developing Alzheimer's disease and other types of dementia. CIHR is supporting the CLSA COVID-19 Study: Understanding the Impact of COVID-19 on Brain Health. During this 10-month study, Teresa Liu-Ambrose and her team at the University of British Columbia will measure the possible effects of COVID-19 on cognitive function and brain structure in individuals aged 55 to 70. These results will support the identification of preventive and therapeutic approaches to promote brain health in those who have had COVID-19.
Supporting Canadians living with dementia in long-term care during the COVID-19 pandemic
CIHR with national and provincial partners, including Healthcare Excellence Canada, launched the Strengthening Pandemic Preparedness in Long-Term Care Implementation Science Research Grants. Over 2020-2021, 22 research teams are collaborating with long-term care homes to evaluate the implementation and sustainability of promising practice interventions and policies designed to improve pandemic preparedness within these homes.
Through this initiative, Andrea Iaboni, Alisa Grigorovich, and Josephine McMurray received funding to further develop and implement the Dementia Isolation Toolkit. This Toolkit aims to support the compassionate, safe and effective quarantine of long-term care residents during the COVID-19 pandemic and to address the moral distress of long-term care staff with implementing the quarantine. The project will evaluate and measure the effectiveness and impact of the Toolkit, and results of this research could support the development and spread of promising practices in person-centered isolation care and in supporting the mental wellbeing of long-term care staff during infectious disease outbreaks.
Additionally, with research funding through CIHR's COVID-19 May 2020 Rapid Research Response Funding Opportunity, Isabelle Vedel at McGill University is leading a study across Quebec, Ontario, Alberta, and Saskatchewan to measure and describe the real-life pandemic experiences of people living with dementia and their caregivers, including those living in a community setting or in long-term care homes using a human rights framework. Using health administrative data, the project is assessing the impact that the pandemic has had on health service use, infection rate, and mortality among individuals living with dementia. People living with dementia and their caregivers will also be interviewed to better understand how the pandemic has impacted their daily lives. This information will be used to develop evidence-based strategies to reduce the impact of unintended harms stemming from public health measures and to help people living with dementia stay safe and healthy throughout the pandemic.
Preventing dementia through risk reduction
Everyone can take action towards reducing the risk of developing dementia. Whether it is building understanding of individual risk factors and acting to reduce them or contributing to healthier social and built environments, every effort can bring Canada closer to the aspiration of the national dementia strategy to significantly reduce the rate of new cases of dementia on the path to prevention.
Dementia prevention: 2020 report of the Lancet Commission
While much remains unknown about what causes dementia, research continues to build understanding of several factors linked to an increased risk of developing dementia. This information in turn provides more insight into what actions and measures can be taken that could contribute to reducing how many Canadians develop dementia. The research also tells us that it is never too early or too late to take steps that may reduce the risk of developing dementia and delay onset and progression of symptoms.
In 2020, the medical journal The Lancet reported that 12 potentially modifiable risk factors account for approximately 40% of dementia cases worldwide. While this estimate is based on a global perspective, these 12 risk factors provide insight into how Canadians may be able to reduce their risk of developing dementia. The identification of these risk factors and the findings from several research studies make a strong case for the potential benefits of taking steps at all stages of life to reduce dementia risk. Several of these risk factors are already well-recognized as being important to overall health and the ability to avoid or manage other chronic conditions such as diabetes.
The table below describes the increased dementia risk associated with the 12 potentially modifiable risk factors from a global perspective. For example, someone who experiences hypertension in midlife could be 60% more likely to be diagnosed with dementia than someone who does not have hypertension. Limiting these risk factors may have a significant impact on reducing the risk overall of dementia and improving one's health.
| Risk factor | Relative increased risk of developing dementia compared to someone without this risk factor |
|---|---|
| Early life (under 45 years old) | |
| Lower levels of education | 60% |
| Midlife (45 to 65 years old) | |
| Hearing loss | 90% |
| Traumatic brain injury | 80% |
| Hypertension | 60% |
| Obesity | 60% |
| Alcohol use (over 21 units per week) | 20% |
| Later life (over 65 years of age) | |
| Depression | 90% |
| Smoking | 60% |
| Social isolation | 60% |
| Diabetes | 50% |
| Physical inactivity | 40% |
| Air pollution | 10% |
Advancing dementia prevention: Strengthening Canada's data
Surveillance and data are a pillar of the national dementia strategy, as this information is essential to informing efforts to reduce risk, and to provide supportive care and health care. New projects were launched in the past year under PHAC's Enhanced Dementia Surveillance Initiative to help collect data on dementia risk and protective factors. Three projects are highlighted below:
Consulting Indigenous stakeholders to improve Indigenous data on dementia
In close collaboration with national Inuit, First Nations, and Métis partner-organizations, a feasibility study led by Laurentian University is focused on identifying dementia information needs, including those related to prevention and risk factors. Based on community consultation with Indigenous organizations, a plan outlining an acceptable and appropriate method for improving dementia surveillance amongst Indigenous populations will be developed.
Ascertaining and exploring dementia risk factors in the Canadian Longitudinal Study of Aging (CLSA)
A new project adds to the work being pursued through the Canadian Longitudinal Study of Aging and will support the early identification of people living with dementia and those at risk of developing dementia. Findings are expected to be used to advance dementia risk reduction and care, as well as dementia surveillance and policy development. The project also aims to establish a comprehensive understanding of dementia risk factors and how common they are in this large cohort of older adults.
Developing a comprehensive and holistic approach to track dementia in Canada
A project led by the Schlegel-University of Waterloo Research Institute for Aging will develop a comprehensive and holistic person-centered model for dementia surveillance that includes social, demographic and economic characteristics of people living with dementia. It also aims to map available data against this model to identify gaps and make recommendations on how to close them.
Advancing on dementia prevention through risk reduction: Initiatives across Canada
Efforts across Canada that can contribute to reducing the risk of dementia come in many forms. Much of what is known about providing healthy environments and adopting a healthy lifestyle is also relevant for reducing the risk of dementia. As well, initiatives that support healthy aging align well with what we currently know about dementia prevention. Individual actions are important measures but research also indicates that the environments around us can have a significant impact.
Improving our built environments
The Housing for Health project focused on the built environment will result in two new pilot development locations in Edmonton region and Whitecourt, Alberta with a focus on older individuals. Health promotion programming and design features aimed to increase physical activity, healthy eating and a sense of community belonging will be integrated based on community consultations. Examples of design features could include the creation of green spaces and paths around the housing developments and community gardens. The project brings together academics, health care providers, housing developers, and multiple government and community partners to collaborate in the planning and design of the developments over five years starting in 2019.
Staying healthy as we age
Support for healthy aging can take many different forms and happens across settings that include homes, communities and care facilities. In New Brunswick, initiatives that are part of the Healthy Seniors Pilot Project program are identifying and evaluating how best to promote healthy aging while supporting seniors living in a variety of settings. For example, PITCH is a new digital health platform available across the province, which assists New Brunswick seniors, including those living with dementia, to proactively monitor and assess their health status and risk factors in order to support their health and stay at home longer.
Other New Brunswick Healthy Seniors Pilot Project initiatives focus on social isolation, a dementia risk factor particularly for those older than 65 years of age. The Nursing Homes Without Walls initiative empowers the local community to become age-friendly by extending supports and services for seniors and caregivers living in rural New Brunswick to ensure that they can age in place while also addressing loneliness by offering regular home visits, which provide opportunities for socialization and health education. The Mobile Seniors' Wellness Network: Reaching Rural New Brunswickers has a multidisciplinary team that includes nurses and social workers which make home visits to provide foot care and social supports for seniors and caregivers in Fredericton and the surrounding region.
"Nursing Homes Without Walls support older adults with multiple health challenges such as hospital discharge, mobility issues and dementia while also addressing the contextual issues of appropriate housing and adequate income and opportunities for activities such as intergenerational initiatives to alleviate social isolation and loneliness. We also focus on health education and interventions to promote healthy aging." – Suzanne Dupuis-Blanchard, RN PhD, University of Moncton
Deepening understanding of the links between stroke, heart disease and dementia
Stroke, heart disease and dementia share similar risk factors (e.g. hypertension, physical inactivity and obesity), while also acting as risk factors for each other. By examining the relationship among these conditions, researchers may be able to identify interventions that can prevent stroke, heart disease and some dementias at the same time. Using newly available data and tools, the Dementia Prevention/Brain Health Initiative led by Vladimir Hachinski at Western University plans to comprehensively map population, environmental, socioeconomic and individual risk and protective factors. This mapping will be the first in Canada to identify geographic areas of high and low rates of brain health, dementia, stroke, and heart disease to better inform the development of cost-effective dementia prevention solutions. The initiative will be built on collaboration across British Columbia, Alberta, Ontario, Quebec and Nova Scotia as well as internationally with New Zealand, United Kingdom, and the United States.
"The Dementia Prevention/Brain Health Initiative is the first nation-wide study examining the interactions between stroke, heart disease and dementia. We hope that Canada will be the first country to demonstrate how to effectively and significantly reduce the risk of these three conditions by using a coordinated approach built on a deeper understanding." – Vladimir Hachinski, Distinguished University Professor, Western University
Data points on preventing dementia
The following data points on preventing dementia provide insight into Canadians' attitudes, levels of awareness around dementia, and whether they are taking steps to reduce their risk. The data points also show that trends for factors linked to the risk of developing dementia appear to be stable, while there is a decrease in the rate of new cases of dementia in Canada.
Taking steps to reduce the risk of dementia
Most Canadians recognize that dementia is not an inevitable part of aging and that actions can be taken to reduce the risk. In fact, approximately 9 in 10 people are aware of at least one risk or protective factor linked to developing dementia, although knowledge is less widespread about some risk factors such as smoking, hypertension and diabetes.Footnote 14
While many Canadians can correctly identify at least a few of the key dementia risk and protective factors, most of the respondents to PHAC's 2020 dementia public opinion survey indicated they had not taken steps in the past year to intentionally reduce their risk of developing dementia. Furthermore, only 37% of respondents knew that the risk of developing dementia is higher among people with chronic health conditions such as hypertension, heart disease and diabetes. This finding suggests that greater efforts are needed to increase awareness about actions that reduce the risk of developing dementia and to remove barriers to taking those actions.
| Data Point | Percentage (%) of Canadians |
|---|---|
| % of Canadians who believe it is true that dementia is an inevitable part of aging. | 16% |
| % of Canadians who are aware of at least one risk factor | 89% |
| % of Canadians who had taken steps to reduce their risk of developing dementia in the last year | 22% |
Key factors linked to the risk of developing dementia
While it appears that many Canadians have not intentionally taken steps to reduce their risk of developing dementia, it is positive news when the rate of dementia risk factors among the general population appears to be moving in the right direction. As the rates for modifiable risk factors decrease and protective factors increase, we can expect that the rate of new cases of dementia in Canada may continue to decrease.
The age-standardized data below shows that the rate of newly diagnosed cases of dementia has decreased between 2008-09 and 2017-18.Footnote 16 Initiatives that raise awareness of risk and protective factors and result in higher adoption of healthy behaviours and better management of related chronic conditions throughout our lives can contribute to continuing to reduce the number of Canadians developing symptoms of dementia.
However, it is important to note that even while the rate of new cases is decreasing, the total number of Canadians living with dementia is expected to continue rising given the aging of Canada's population. As of 2017-18, almost 452,000 Canadians aged 65 years and older were living with diagnosed dementia (including Alzheimer's disease), an increase of almost 10,000 than in the previous year. The risk of developing dementia increases with age, doubling every 5 years between the age of 65 and 84. While less than 1 percent of Canadians between the ages of 65 and 69 are living with dementia, this number increases to around 25 percent for those aged 85 and over.Footnote 17
The table below reports the change in the percentage of Canadians with modifiable dementia risk and protective factors over time.
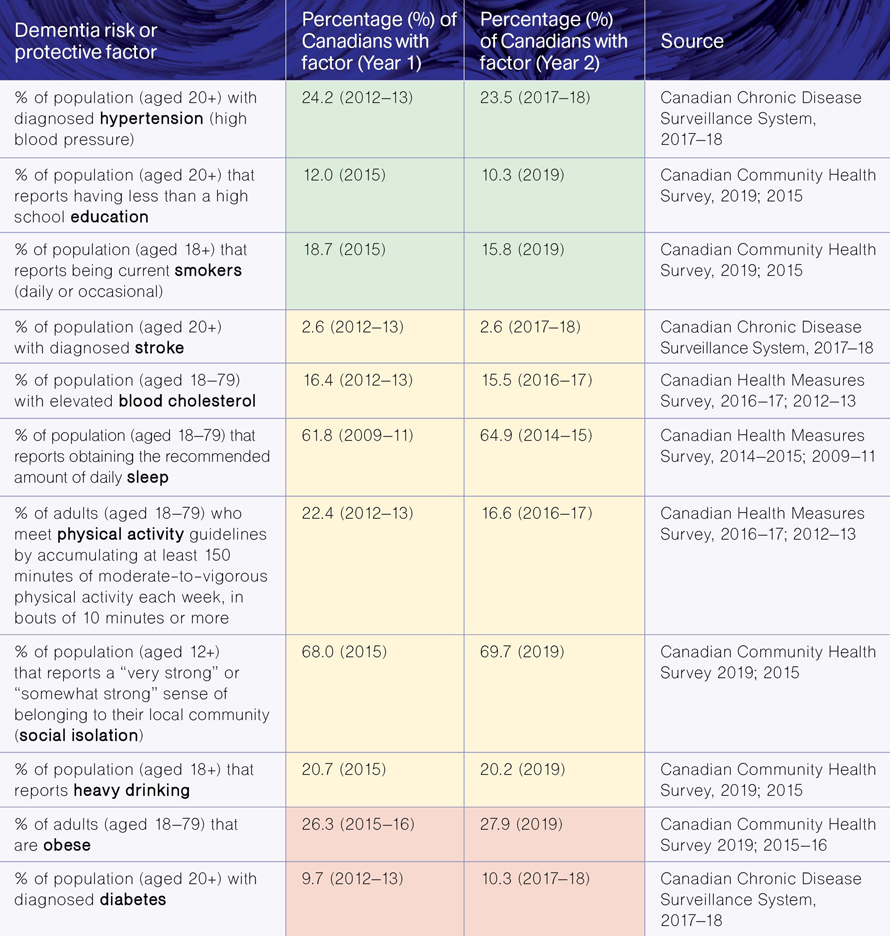
Figure 2: Text equivalent
| Dementia risk or protective factor | Percentage (%) of Canadians with factor (Year 1) | Percentage (%) of Canadians with factor (Year 2) | Trend | Source |
|---|---|---|---|---|
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | 24.2 (2012-13) | 23.5 (2017-18) | Positive | Canadian Chronic Disease Surveillance System, 2017-18 |
| % of population (aged 20+) that reports having less than a high school education | 12.0 (2015) | 10.3 (2019) | Positive | Canadian Community Health Survey, 2019; 2015 |
| % of population (aged 18+) that reports being current smokers (daily or occasional) | 18.7 (2015) | 15.8 (2019) | Positive | Canadian Community Health Survey, 2019; 2015 |
| % of population (aged 20+) with diagnosed stroke | 2.6 (2012-13) | 2.6 (2017-18) | Neutral/ not statistically significant | Canadian Chronic Disease Surveillance System, 2017-18 |
| % of population (aged 18-79) with elevated blood cholesterol | 16.4 (2012-13) | 15.5 (2016-17) | Neutral/ not statistically significant | Canadian Health Measures Survey, 2016-17; 2012-13 |
| % of population (aged 18-79) that reports obtaining the recommended amount of daily sleep | 61.8 (2009-11) | 64.9 (2014-15) | Neutral/ not statistically significant | Canadian Health Measures Survey, 2014-2015; 2009-11 |
| % of adults (aged 18-79) who meet physical activity guidelines by accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or more | 22.4 (2012-13) | 16.6 (2016-17) | Neutral/ not statistically significant | Canadian Health Measures Survey, 2016-17; 2012-13 |
| % of population (aged 12+) that reports a "very strong" or "somewhat strong" sense of belonging to their local community (social isolation) | 68.0 (2015) | 69.7 (2019) | Neutral/ not statistically significant | Canadian Community Health Survey 2019; 2015 |
| % of population (aged 18+) that reports heavy drinking | 20.7 (2015) | 20.2 (2019) | Neutral/ not statistically significant | Canadian Community Health Survey, 2019; 2015 |
| % of adults (aged 18-79) that are obese | 26.3 (2015-16) | 27.9 (2019) | Negative | Canadian Community Health Survey 2019; 2015-16 |
| % of population (aged 20+) with diagnosed diabetes | 9.7 (2012-13) | 10.3 (2017-18) | Negative | Canadian Chronic Disease Surveillance System, 2017-18 |
Newly diagnosed cases of dementia (incidence)
As efforts continue to advance dementia prevention, the hope is to continue to see the number of new cases (incidence) of dementia decrease in Canada. This data point shows the age-standardized rate of newly diagnosed cases of dementia for those aged 65 and over between the years 2008-09 and 2017-18, which has been decreasing over the past 10 years of available data in Canada.Footnote 16 This decreasing trend is similar for men and women.
2008-2009
There were 1,576 new cases per 100,000 Canadians aged 65+ years
- 1,619 per 100,000 Canadian women aged 65+ years
- 1,500 per 100,000 Canadian men aged 65+ years
2017-2018
There were 1,418 new cases per 100,000 Canadians aged 65+ years
- 1,445 per 100,000 Canadian women aged 65+ years
- 1,374 per 100,000 Canadian men aged 65+ yearsFootnote 21
Spotlight: Canadian 24-Hour Movement Guidelines
Maintaining a healthy balance of physical activity and rest is important to brain health. Statistics suggest, however, that Canadians of all ages are becoming less physically active. While some may find it challenging to be more active, especially when pandemic restrictions reduce options, it is important to remember that all types of movement contribute to improving brain health and some activity is better than none. Activities of daily living, including neighbourhood walks, gardening, grocery shopping and household chores are all types of movement that contribute towards a healthy 24 hours.
In 2020, the Canadian Society for Exercise Physiology released the world's first Canadian 24-Hour Movement Guidelines for adults (ages 18-64 years) and adults (ages 65 years or older), which are designed to accommodate all genders, cultural backgrounds, and varying socio-economic status. These guidelines reflect emerging research and evidence of the important relationship between sleep, physical activity and sedentary behaviour in chronic disease prevention and improved mental and physical health. Beyond reducing the risk of developing dementia, there are other expected health benefits for adults following the movement guidelines such as a lower risk of cardiovascular disease, high blood pressure, type 2 diabetes, several cancers and high cholesterol. For adults 65 years and older, following these guidelines is also expected to lower the risk of falls and fall-related injuries. Tailored guidelines are available for Canadians of all ages, including early years (ages 0-4 years) and children and youth (ages 5-17 years).
The Canadian 24-Hour Movement Guidelines focus on three core recommendations for adults:
- Move More: Perform a variety of types and intensities of physical activity throughout your day.
- At least 150 minutes per week of moderate to vigorous aerobic physical activity. Moderate-intensity physical activities include brisk walking and bicycling, while vigorous-intensity physical activities can include cross-country skiing, swimming and jogging.
- Aim for several hours of light physical activity every day, including standing.
- Those aged 65+ should also include physical activities that challenge balance.
- At least twice a week of muscle strengthening activities using major muscle groups such as strength training, resistance training and heavy gardening involving digging or shovelling.
- Reduce Sedentary Time: Limit time awake spent sitting or lying down to 8 hours or less per day, including no more than 3 hours of recreational screen time and breaking up long periods of sitting when possible.
- Sleep Well: For those aged 18-64, 7 to 9 hours of good quality sleep on a regular basis is recommended, and 7 to 8 hours for those 65+ years. Keeping consistent times for getting up and going to bed is also recommended.
Applying research and innovation to dementia challenges
Across Canada, hundreds of researchers are focused on addressing dementia-related challenges including improving and evaluating the therapies available to people living with the condition. Conducting research, exploring the potential of innovative technologies and gathering evidence are fundamental activities that support progress across all three national objectives of the strategy. This chapter highlights efforts underway across Canada which focus on advancing therapies and working towards a cure as well as projects that apply innovative technologies to challenging dementia-related issues.
Applying research and innovation to dementia challenges: Initiatives across Canada
Advancing therapies
Work on advancing therapies for dementia takes many different forms, including better understanding factors that affect the progression of the condition as well as improving the ability to support risk identification and diagnosis so that therapy can begin earlier and potentially make a greater contribution to quality of life. This work also covers the growing use of non-drug (non-pharmacological) therapies that studies increasingly suggest can help to maintain physical and mental health, possibly slowing the progression of symptoms.
Supporting diagnosis and brain health
Antibody-based therapeutics
At the National Research Council (NRC) of Canada, the Multi-functional Antibody-based Therapeutics Research program focuses on designing and evaluating new therapies to slow the progression of symptoms for individuals with early stage dementia. In collaboration with a pharmaceutical company, the program is moving an NRC-developed treatment through pre-clinical steps and into planned clinical trials. To support efforts to identify people with dementia and monitor the effectiveness of treatments, the program also supports research and development regarding biomarkers. Effective biomarkers are expected to make it easier to diagnose dementia earlier.
Biomarker Research
Biomarkers are measurable indicators that enable the detection and tracking of health conditions through different laboratory and imaging tests. Although some biomarkers for various types of dementia have been identified, such as markers seen through positron emission tomography (PET) scanning and cerebral spinal fluid (CSF) testing, work continues to identify accessible, reliable, and specific biomarkers for use in clinical and research settings.
Recently, biomarkers of dementia that can be measured in the blood (blood-based biomarkers) have been a major focus as these types of tests are generally cost-effective, less invasive, and simple to use. For example, some blood-based biomarkers aimed at detecting Alzheimer's disease have shown promise in measuring amyloid, tau, and neurodegeneration in general. Blood-based biomarkers for dementia subtypes are expected to accelerate research for new therapies by enabling researchers to quickly identify participants for enrollment in studies and better analyze the results to determine if some treatments are more effective for people with specific characteristics. In the clinic, blood-based biomarkers could possibly improve dementia prevention, by allowing for early identification of those at risk for dementia, and improve quality of life, by making it easier to diagnose dementia earlier, identify those who may benefit from specific treatments, and monitor the effectiveness of the treatments and progression of disease.
Investigating links between sleep and dementia
There is a growing focus on the connection between the quality of sleep and dementia. Andrew Lim at the Sunnybrook Research Institute in Toronto is leading a study of 3000 Ontario adults to fill important gaps in our knowledge about the impact of sleep and the disruption of circadian rhythms (the natural sleep-wake cycle) on dementia, and associated changes to the brain. By using wearable technology to assess sleep and circadian rhythms, and combining this information with brain imaging and genetic testing, this study is expected to make it easier to identify adults at high risk for dementia, support clinical trials of existing and emerging dementia interventions, and may lead to targeted therapies that improve brain health for those who experience sleep and circadian rhythm disruption.
Alternative therapies
Across Canada, many different types of non-drug therapies are being applied and evaluated for their contribution to the quality of life of people living with dementia. The Continuing Care Speech Language Pathologist (SLP) Team with Yukon Health and Social Services provides support to long-term care staff and families to improve communication skills and approaches with people living with dementia who may have communication difficulties. The approaches used by the SLP Team aim to enhance information sharing, support social closeness and reduce frequency and severity of responsive behaviors. For example, the team promotes the use of memory books to enhance conversation between residents, and staff and family members. The memory books are created with the residents and include life reflections, family and home life, how to help them in everyday life, and what they look forward to.
Applying innovative technologies to promote wellbeing and quality of life
Using digital tools to support diagnosis and improve care
State-of-the-art digital tools for early diagnosis of dementia are being developed through a five-year partnership between the Vancouver Island Health Authority, the University of Victoria, and the University of British Columbia. The Neil and Susan Manning Cognitive Health Initiative (CHI), established in 2017, enables greater collaboration between clinicians, researchers, and health care educators and has resulted in tools such as the MyCogHealth mobile app, which allows for remote monitoring of cognition over time. This app is expected to be available nationwide once it is released, anticipated in 2021. Future phases of this initiative will provide a scalable, remotely-administered cognitive assessment platform to support dementia prevention efforts. The CHI has also created a learning health system for dementia care on Vancouver Island, the Dementia Guidance System database, which tracks and clusters symptoms, treatment plans, and outcomes in real time to continually adapt and improve care. The system allows care providers to create tailored, yet standardized information and resources. Care providers are able to apply best practice guidelines for dementia care quickly and easily while connecting individuals with local resources and supports.
Using innovative technologies to understand and reduce the risks of wandering
Wandering is a common concern for people living with dementia. A project to better understand, predict and reduce wandering risks through the use of technologies, such as mobile apps, is underway at the University of Waterloo, led by Lili Liu. This AGE-WELL-supported project is also expected to help locate those who have gone missing when wandering by developing algorithm-informed drones. The first version of a scale to assess the usability of locator device technologies, such as how well it performs, the ease of use, and how likely it is to be used, was completed in June 2021.
"People living with dementia have the right to participate in their communities in meaningful ways. AgeTech and dementia-capable communities can mitigate the risks of going missing, help manage a person's safety and enhance one's quality of life." – Lili Liu, PhD, AGE-WELL Researcher
Exploring how automated vehicles may support the independence of people living with dementia
The potential of automated vehicles (AVs) to provide an acceptable way to extend the safe driving period of people living with dementia is being investigated through a project led by Jennifer Campos from the University Health Network's KITE -Toronto Rehabilitation Institute. The project includes discussions with caregivers and people living with dementia across Canada to gather their perceptions on the use of AVs. In addition, through the use of DriverLab, Canada's most advanced driving simulator, people living with dementia are able to experience operating an AV and provide feedback on the use of this technology.
Using technology to support care at home
Reg Urbanowski is leading a research team at the University of Manitoba that is developing robots to help care for persons living with dementia at home. Through the use of cameras, speakers, microphones and a display monitor, telepresence robots will allow caregivers to see how the person they are caring for is doing while they are home alone. This application of robots, if proven effective, is expected to help people living with dementia maintain a higher level of independence and reduce loneliness, while also helping caregivers balance work and family life.
Another group of researchers led by Nathalie Bier at the University of Montreal is working to develop a technology called COOK (Cognitive Orthosis for Cooking) to assist older adults living with cognitive impairment, including dementia, to plan and independently prepare meals safely at home. The technology would support meal preparation through meal planning and step-by-step guidance in the preparation of a simple meal. In addition, a security system would monitor various factors, such as the stove top temperature, opening of the oven door, proximity of the person to the stove, and could automatically turn off the stove and call for assistance if a dangerous situation is detected. The researchers are engaging people living with dementia, caregivers and health care professionals to test COOK and provide feedback.
The Government of Canada's commitment to dementia-related research
Through the Canadian Institutes of Health Research (CIHR), the Government of Canada continues to invest in research to reduce the risk of dementia, delay the clinical progression of symptoms, and improve the quality of life of people living with dementia.
Between 2015-16 and 2019-20, CIHR invested over $203 million in dementia research. The Canadian Consortium on Neurodegeneration in Aging (CCNA) is at the centre of the Government of Canada's investment in dementia-related research. The CCNA, which brings together over 300 researchers and partners from across Canada, is Canada's research hub on neurodegenerative diseases that affect cognition in aging, including dementia. In June 2019, the CCNA entered Phase II of its work with a renewed federal investment of $31.6 million and an additional $14 million from partners, for a total of $46 million over five years to help accelerate dementia research, including on prevention, detection and treatment of dementia, and improving the quality of life for those living with dementia and their caregivers.
Federal investment on dementia-related issues extends beyond CIHR's funding programs and the CCNA. For example, in 2021, the National Research Council of Canada launched its new Aging in Place Challenge Program. By 2031, this seven-year program aims to reduce by 20% the number of older adults (65+) who will require facility-based care. This new program intends to improve the quality of life of people living with dementia and support caregivers by developing technologies that support independence in activities of daily living and maintain social connections. The program will investigate the use of digital interventions, such as virtual reality, to improve or maintain cognitive abilities for both prevention of dementia and for use by people living with dementia. It will also support the development of new methods for the early diagnosis of cognitive decline, including molecular and functional biomarkers. The program team is committed to engaging older adults, people living with dementia, and caregivers through various ways, such as an 'Experts by Experience' community, who will be involved in the research projects as advisors and participants.
Data points for advancing therapies and finding a cure
Data points related to the strategy's national objective focused on advancing therapies and finding a cure provide information about CIHR's annual investment in dementia-related research and its support of the next generation of researchers. This year's report also shares the total number of federally-approved drug-based therapies for dementia.
Federal investment in dementia research
The federal research investment in dementia by CIHR reflects investments across many dementia topics beyond therapies to include efforts related to prevention and quality of life, supporting all three national objectives of the strategy. This investment includes investigator-initiated research (e.g., funded through the Project Grant competition), research in priority areas (including the Canadian Consortium on Neurodegeneration in Aging), and training and career support programs (e.g., Fellowships).
CIHR funding for dementia research in Canada
Dementia research spending by CIHR in 2019-20: approximately $42 millionFootnote 22
Dementia research spending by CIHR in 2018-19: approximately $40.8 millionFootnote 22
Training the next generation of dementia researchers
As Canada's population ages, research will provide essential evidence to inform dementia care and policies. Supporting the next generation of researchers is critical to ensuring that Canada continues to have the capacity to conduct dementia research that will improve the lives and care of individuals living with dementia and caregivers now and into the future. This data point reports on the approximate number of students/trainees engaged in dementia research through CIHR funding. This includes students and fellows who either received a training award (direct trainees), or received a stipend paid through researcher grants (indirect trainees).
Number of direct and indirect trainees supported through new and ongoing CIHR-funded dementia research projects in 2019-20: 375Footnote 23
Number of direct and indirect trainees supported through new and ongoing CIHR-funded dementia research projects in 2018-19: 359Footnote 23
Approved pharmaceutical therapies for the management of dementia symptoms
Some drug therapies for dementia have been approved that may improve memory and thinking. The third data point for this national objective shares the number of pharmaceutical therapies currently approved by Health Canada for the management of dementia symptoms.
Number of therapies (pharmaceutical drugs) approved by Health Canada for management of dementia symptoms as of March 2021: 4Footnote 24
Keeping quality of life at the forefront
Improving the quality of life for people living with dementia and caregivers is at the core of the national dementia strategy, and is one its key objectives. The aspirations of the strategy related to quality of life touch on how well people living with dementia are included and welcomed in all aspects of life, as well as the quality of care provided and the supports available to caregivers who make a tremendous contribution.
The impact of the COVID-19 pandemic has reduced quality of life for many Canadians living with dementia and caregivers, especially due to isolation from loved ones. Lessons learned during the pandemic from successful quality of life initiatives need to be kept in mind to ensure better preparations for possible similar events in the future. The pandemic has also drawn attention to the work that needs to be done to improve the care available to older Canadians, particularly in long-term care homes.
The negative assumptions and stereotypes associated with dementia can create barriers to the participation of people living with dementia in their communities and in activities that bring them joy and reduce isolation. This stigma can also discourage people from seeking health care advice that may result in a diagnosis of dementia; however delaying diagnosis can increase social isolation, delay important care, therapies and support, and make it more difficult to plan for the future. Making activities and communities more dementia-inclusive is one way to reduce stigma and support the quality of life of people living with dementia - this includes making it easier to participate in social activities and to move around safely in the community. Opportunities for social connection, including with younger people, creates more dementia-inclusive communities and helps to improve understanding that each individual's experience of dementia is different and that quality of life remains possible for many living with this condition.
The quality of care available and supports for caregivers are essential elements of quality of life and across Canada, efforts continue to improve many aspects of care. Federal commitments announced in Budget 2021 will contribute to these efforts and new funding will support: increasing accessibility in communities and workplaces, such as parks and public buildings that would benefit seniors with and without disabilities and help create age-friendly communities in Canada; strengthening long-term care and supportive care to ensure care standards are being applied; establishing national standards for mental health services and implementing mental health interventions for populations disproportionately impacted by COVID-19; and designing and delivering interventions to prevent elder abuse.
Keeping quality of life at the forefront: Initiatives across Canada
Reducing stigma and encouraging dementia-inclusive communities
Creating inclusive communities for people living with dementia does not always require major changes or large investments. Small efforts can create a safer and more welcoming environment. The availability of services, activities and places designed to enable people living with dementia to interact with others helps to create more inclusive communities. Some examples are shared below.
Designing community programs for seniors
The Seniors Network of Maple Ridge, Pitt Meadows, and Katzie First Nation is a community planning table in British Columbia led by seniors for seniors, whose goal is to strengthen the availability and quality of services, programs and resources for seniors. Among its many activities, this group has developed a guide on local dementia resources and produced a survey of people living with dementia and caregivers to assess the dementia-inclusiveness of the community. In addition, the Danser vers la santé exercise and dance program in New Brunswick is being expanded to integrate seniors who have mild cognitive impairment. It will evaluate physical and cognitive changes in participating seniors, improve the quality of life for participants and lay the groundwork to share findings across Canada.
Supporting intergenerational connections
There are many initiatives across Canada that recognize the value of establishing and nurturing social connections between generations as a way of reducing stigma and building dementia-inclusive communities. Learning Together: Bridging the Generation Gap is an intergenerational mentoring and learning initiative through Conestoga College in Kitchener/Waterloo. It supports senior volunteerism and fosters the appreciation and inclusion of seniors by providing opportunities for seniors, college students and faculty to interact. Activities include online mentoring and learning sessions to connect students and faculty with seniors (including those living with dementia) and caregivers across the country to speak about lived experiences, build relationships, and learn from one another.
The Victoria Memory Café is an intergenerational program for people living with dementia, care partners, and university students. The Café is reducing stigma and social isolation through joyful interactions that focus on imagination and participation. The program engages participants in creative activities such as poetry, art, story-creation, and music-making. University of Victoria researchers developed the program and are evaluating program outcomes.
"Memory Café Victoria made all the difference in reducing my stress and loneliness. The weekly gatherings offered the company of others without focusing on dementia. Our weekly gatherings online were full of laughter, conversation, and creative engagement. The focus on imagination allowed everyone to participate and made life seem normal. Each week was energizing, nurturing and joyful. I can't wait until our Café group can meet in person rather than online and hope the program will be offered again." – Caregiver, Victoria Memory café
Challenging stigma around dementia
Music Is Life is a documentary that follows people living with dementia at the Dotsa Bitove Wellness Academy and musician, Simon Law, as they compose a song about the meaning of music in their lives. This film challenges the stigma associated with dementia and conveys the power of music for connection, life enrichment, and creative self-expression. Evaluation of this initiative found that some care providers who watched this film took away new insights for compassionate care and changed how they practiced and engaged with people living with dementia.
"This documentary completely changed my practice. Before watching it, I never thought about how using music exclusively for clinical outcomes, such as managing challenging behaviours and improving functioning, stigmatizes people living with dementia. I now use music to cultivate meaningful relationships in long-term care and focus less on meeting functional goals." – Taylor Kurta, Music Therapist
Supporting healthy built environments
The Government of Canada's Enabling Accessibility Fund will invest $100 million over two years to support renovation, construction, and retrofit projects (such as building ramps, automatic door openers, and supports for the hearing impaired) to make communities and workplaces more accessible, starting in 2021-22.
Promoting early diagnosis to support care planning
Access to early diagnosis is an essential component of quality of life when it contributes to the ability to plan and access supports earlier. The Healthcare Excellence Canada webinar discussion series profiles innovations that aim to improve the capacity to provide early, competent and compassionate dementia diagnoses in primary care (including virtual care access) as well as post diagnostic support such as care coordination and navigation. Through the webinars, relevant innovations are shared, and participants can join a conversation to help inform the feasibility of adoption and spread.
"The Healthcare Excellence Canada webinars showcased impressive innovations to improve timely dementia diagnosis and to enhance access to community services and support. Its participants now need action and government investment to spread and scale." – Mary Beth Wighton, Co-Chair of Dementia Advocacy Canada
Improving the quality of dementia care
Improving navigation of the health care system
Health care patient navigation can help to remove barriers to care by coordinating care and transitions within the health care system and community-based supports. Based on the NaviCare Model (a previous pediatric patient navigation program in New Brunswick), Healthcare Excellence Canada has partnered with a research team from the University of New Brunswick to explore the feasibility of a navigation program for people living with dementia. This partnership aims to support navigation for people living with dementia, caregivers, and care teams in order to ensure that people living with dementia have access to health, social, and education services in a timely manner. The research team also created a toolkit to support the implementation of a navigation program in other jurisdictions to improve access to post-diagnostic supports.
Wayfinding tools
In addition to navigating the health care system, it is important for people living with dementia to be able to navigate their way around their physical environment. Wayfinding tools such as accessible signage support people living with dementia to access and fully participate in their environment independently and with confidence. Yukon is improving signage in all continuing care homes to make wayfinding more apparent and intuitive. This initiative was completed last year at Copper Ridge Place, one of the Yukon Continuing Care Homes in Whitehorse, and will be initiated in all other continuing care homes in Yukon by June 2021.
Research to enhance dementia care
Research is underway to examine ways to improve health care for people living with dementia, often exploring the potential of innovative technologies. For example, artificial intelligence tools are being investigated for their potential to improve care planning at the Bruyère Research Institute and the Ottawa Hospital Research Institute. Peter Tanuseputro is leading a team that will identify ways to predict the long-term outcomes of individuals living with dementia, which will then be developed into easy-to-navigate online tools for both clinicians and people living with dementia and their families. This project will look at the health trajectory of people living with dementia throughout their various interactions with the health care system, from diagnosis to assisted care. The team will focus in particular on the delivery of palliative care to identify gaps and assess the impact of palliative care on the dying experience at various points of progression. The work is expected to support better advanced care planning and delivery.
Supporting long-term care and improving palliative care
Budget 2021 announced a $3 billion investment to Health Canada to support provinces and territories in ensuring standards for long-term care are applied and permanent changes are made. Budget 2021 also announced $29.8 million over six years, starting in 2021-22, to advance the Action Plan on Palliative Care through initiatives such as improving palliative care skills and supports, enhancing data collection and research and improving access to culturally sensitive palliative and end-of-life care.
Improving the quality of life of people living with dementia and caregivers: Strengthening Canada's data
Surveillance data can provide the foundation for public health action aimed at improving the quality of life of people living with dementia and caregivers. New projects under PHAC's Enhanced Dementia Surveillance Initiative launched in the past year will help to inform future initiatives supporting quality of life:
Using health administrative data to describe other conditions people living with dementia face (comorbidities)
Building on the Canadian Chronic Disease Surveillance System, provincial partners are collaborating to collect data on other chronic conditions occurring among people living with dementia (comorbidities). Knowing more about the impacts of comorbidities on the health status of people living with dementia and how they use health care services can inform approaches and initiatives to improve quality of life.
Collecting data on where people with dementia are living
Provincial partners will use health administrative data to better understand the proportion of people with dementia living in the community versus in long-term care settings. Knowing where people with dementia live is essential when designing policies, programs, and initiatives aimed at improving quality of life for people living with dementia and caregivers.
Health surveillance of people living with dementia and caregivers dyads (pairs) living in the community
This LIFE Research Institute (University of Ottawa) project plans to follow people living with dementia and caregivers together using the Canadian Primary Care Sentinel Surveillance Network. Gathering data on their experiences and following their health journey can produce relevant information for the development of quality of life initiatives.
Building the capacity of care providers
Supporting training for care providers and building a skilled workforce
As the number of people living with dementia increases, so does the need for skilled care providers, including personal support workers. Conestoga's Personal Support Worker's Flexible, Accessible, Short, Training program (PSW-FAST) is an accelerated 21-week training program that took place in Spring 2021 to build capacity and increase the number of skilled personal support workers (PSWs), through online learning and lab training. To date, approximately 1,000 PSWs have participated in the program.
Enabling a skilled workforce continues throughout the career of care providers through professional development training. Dementia Passport is an evidence-based e-learning platform designed to support health care professionals in providing quality care. Developed by the Alzheimer Society of Newfoundland and Labrador, it is providing access to the e-learning platform for home and personal support workers. Learning modules include topics related to the types of dementia, transition to care options, and person-centered care, including a focus on the rights of people living with dementia.
Enabling person-centered language
Person-centred language is the practice of using respectful, life-affirming and inclusive language which is important for people who communicate through responsive behaviours and personal expressions associated with dementia, mental health, and other neurological conditions. The Ontario Centres for Learning, Research and Innovation in Long-Term Care, in collaboration with Behavioural Supports Ontario and MacHealth, have launched an e-learning course that aims to equip long-term care teams with practical knowledge of how to implement person-centred language. This interactive e-course will demonstrate how person-centered language can have a positive impact on communication and care, and help to reduce stigma and discrimination.
Promoting continuing education on palliative care for health and care providers
Palliative care focuses on pain management and can provide psychological, social, emotional, spiritual and practical support. The LEAP program through Pallium Canada provides home care and long-term care providers with palliative care education. LEAP courseware, tools and resources build the capacity of care teams to provide a palliative care approach, ensuring better care for individuals and their families. The Government of Nunavut partnered with Pallium Canada to deliver LEAP courses in English and Inuktitut to over 60 learners in Iqaluit, including nurses, physicians, personal support workers, and pharmacists since 2018.
Support for caregivers
Expanding supports for caregivers
Caregivers provide essential support to people living with dementia, but their needs can often be overlooked. Many initiatives across Canada focus on protecting the health of caregivers, including providing tools and resources. For example, Caregivers Alberta is expanding programs and resources for the almost one million Albertan caregivers. This expansion includes: developing a public awareness campaign; compiling an inventory of caregiver supports across the province; expanding the hours of the Caregiver Advisor phone line; establishing a referral system; updating and expanding support programs; providing employers with resources; and developing a coaching program for caregivers.
Promoting mental health and wellbeing of caregivers
Mindfulness-based interventions (MBIs) show promise in reducing stress-related ailments including depression and chronic pain. Alexandra Fiocco at Ryerson University is examining benefits associated with a tailored caregiver MBI program (C-MBI) and is working to determine whether C-MBI can enhance resilience, as shown by improvements in psychological wellbeing, cognitive health, and biological measurements of stress. This study, which started in 2021, aims to contribute to improving the wellbeing of caregivers and to the development of standardized programming to promote resilience.
Creating resources for caregivers
iGeriCare is an Internet-based educational program for caregivers of people living with dementia. It was developed by experts in dementia, multimedia e-learning, and mental health from McMaster University, as well as caregivers. It is intended to improve knowledge and confidence, and to raise awareness of strategies and services to improve quality of life and promote risk reduction.
"The Centre for Aging and Brain Health Innovation (CABHI) supports, spreads, and scales innovations to help people with dementia live their best possible lives. For example, with CABHI's support, iGeriCare has reached over 150,000 dementia care partners to date, and has adapted the dementia e-learning resource for health care providers." – Anthony Levinson and Richard Sztramko – Co-founders of iGeriCare
The Dementia Community Investment (DCI): Optimizing the wellbeing of people living with dementia and family and friend caregivers
The Dementia Community Investment (DCI) seeks to improve the quality of life for people living with dementia and their family and friend caregivers and increase knowledge about dementia. DCI projects involve partnerships between community-based organizations and researchers to develop, test, scale-up and evaluate interventions. Below are three examples of current DCI funded projects that support the national objective of improving the quality of life of people living with dementia and caregivers.
The University of British Columbia and Lakehead University are working with the Westside Seniors Hub in Vancouver and the North West Dementia Working Group in Thunder Bay, to implement an asset based community development (ABCD) approach. The ABCD approach is founded on the idea that a community is best positioned to identify its own needs and address these based on its own strengths and is directed by people living with dementia. To date, Vancouver participants have focused on small group programs that increase social connectedness, including dementia cafes and outdoor walking groups. Thunder Bay participants have focused on advocating with local institutions, such as businesses and libraries, to increase access for people living with dementia and caregivers. It is anticipated that at the end of the project there will be a better understanding of how people living with dementia and caregivers can facilitate an enhanced quality of life for themselves. A guide will also be developed to support other communities in using an asset based approach to implement similar initiatives.
The Hamilton Council on Aging is working in both Hamilton and Haldimand to develop dementia friendly action plans. The project will explore how a community with an existing Age Friendly Plan (Hamilton) versus a community without one (Haldimand) can become a dementia-inclusive community. The project consulted over 300 people living with dementia and caregivers in Hamilton and Haldimand to determine the best way to support them in their communities. Five key themes emerged in both communities: empowering people living with dementia, challenging stigma and building understanding, fostering social inclusion and participation, creating dementia-inclusive built environments and transportation, and improving community responsiveness to crises and COVID-19. Next steps for this work include engaging people living with dementia to assist in creating action plans that address these themes in their communities. Working with community members and partners, including the GERAS Centre for Aging Research, the project will evaluate the process and outcomes of establishing dementia friendly communities in a number of settings, including rural versus urban, and how to best support long-term sustainability.
"As part of the Empowering Dementia Friendly Communities Project, I am an active member of the project team, informing decisions about the project and co-chairing the newly developed lived-experience leadership teams. I feel like I am thriving, learning new things and using my skills and knowledge to make meaningful change in my own community." – Debbie Keay, person living with dementia, EDFC
The British Columbia Centre for Palliative Care is developing a set of tools, resources and training materials to support community organizations across British Columbia in delivering Advance Care Planning (ACP) programs for people living with early stages of dementia and their family and friends. Due to COVID-19, the community-led model, interventions and toolkits have been adapted to support both in-person and remote delivery. Two community-led ACP programs, which include a guided group conversation and a two-part ACP information session, were developed as part of the project. The guided group conversation helps participants explore their values, wishes, and beliefs for future health and personal care. The ACP information sessions teach participants about the steps of ACP, and offer information and resources. The two programs were designed to complement each other and to be taken in sequence. From October 2020 to February 2021, the two programs were piloted in partnership with four community-based organizations in BC. The project is now implementing and evaluating the improved programs in partnership with ten community-based organizations.
Data points on improving the quality of life for people living with dementia and caregivers
Stigma
The strategy's aspiration of eliminating the stigma associated with dementia is vital to improving the quality of life of people living with dementia and caregivers. Stigma happens in many different ways such as assumptions that people living with dementia will inevitably experience a lower quality of life as well as feelings of discomfort when interacting with someone living with dementia. For those experiencing symptoms, stigma might contribute to a reluctance to have discussions with care providers that could lead to a diagnosis or to share information about a diagnosis with friends, neighbours and others in the community.
The following data point, gathered through 2020 baseline public opinion research, indicates that almost half of the general population feels uncomfortable interacting with someone who has dementia and two-thirds agree with the perception that people living with dementia face a lower quality of life than people without dementia (70%).
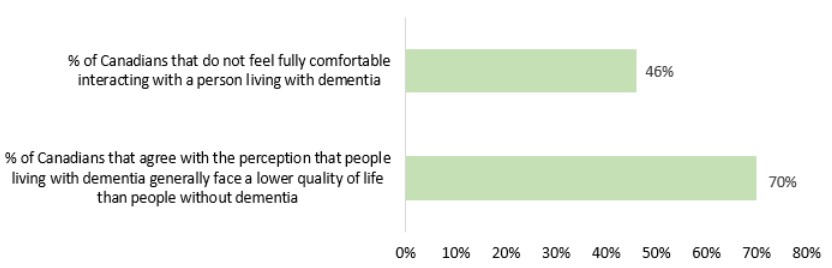
Figure 3: Text equivalent
| Data point | Percentage |
|---|---|
| Percentage of Canadians that do not feel fully comfortable interacting with a person living with dementia | 46 |
| Percentage of Canadians that agree with the perception that people living with dementia generally face a lower quality of life than people without dementia | 70 |
Quality of life: depression, pain, social interaction
Quality of life is a complex concept that is influenced by many different factors which differ from person to person. This remains true for people living with dementia. The data points below represent people living with dementia who are receiving home care in three provinces and one territory and focus on three components of quality of life: social interaction, depression and daily pain.Footnote 25 The findings suggest that most people living with dementia who are receiving home care engage in activities of interest and have social interactions, nearly 35% experience daily pain and nearly 25% show signs of depression. These statistics have stayed relatively stable across the last two years of data.Footnote 26
| Data point | Percentage (%) of Canadians in 2018-19 | Percentage (%) of Canadians in 2019-20 |
|---|---|---|
| People living with dementia receiving homecare with withdrawal from activities of interest and/or reduced social interaction | 18.3 | 19.1 |
| People living with dementia receiving homecare with a potential or actual problem with depression, based on a depression rating scale | 24 | 24.8 |
| People living with dementia receiving homecare with daily pain (severe and not severe) | 34.6 | 34.6 |
Caregivers experiencing distress
People living with dementia, particularly those who are still living at home, often have a caregiver living with them or who visits frequently to support activities of daily living. This data point measures distress encountered by caregivers to people living with dementia who receive home care in contrast to those who are providing care to people without dementia who receive home care, in three provinces and one territory.Footnote 25 For those receiving home care, findings show caregivers of people living with dementia are nearly twice as likely to indicate that they are distressed and/or unable to continue with their caregiving role as caregivers who are providing care to people with any other health condition.
Percentage of caregivers of people living with dementia experiencing distress, compared to caregivers of people with any other health condition experiencing distress: 37.1% vs. 18.9% in 2019-2020.
In 2018-19, the percentage of caregivers of people living with dementia experiencing distress, compared to caregivers of people without dementia was 37.6% vs 18.6%.
This percentage includes caregivers who experience distress, anger and/or depression as well as those who are unable to continue in their role as caregivers.
A second data point focused on caregivers, gathered through 2020 dementia baseline public opinion research, focuses on the reasons that family/friend caregivers felt unable to provide the care needed by someone living with dementia.
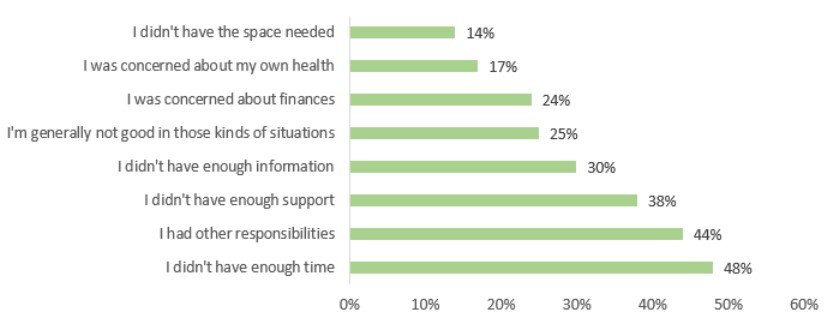
Figure 4: Text equivalent
| Reasons an unpaid caregiver to someone living with dementia felt unable to provide the care needed for someone living with dementia | Percentage |
|---|---|
| I didn't have the space needed | 14 |
| I was concerned about my own health | 17 |
| I was concerned about finances | 24 |
| I'm generally not good in those kinds of situations | 25 |
| I didn't have enough information | 30 |
| I didn't have enough support | 38 |
| I had other responsibilities | 44 |
| I didn't have enough time | 48 |
Quality of life in long-term care facilities
In some cases, as dementia progresses and care needs change, people living with dementia may move into long-term care facilities where around-the-clock support is provided. As shown in the table below, people living in long-term care facilities with dementia are five times more likely to wander and 24% more likely to exhibit responsive behaviours, such as agitation, than those without dementia. People living with dementia in long-term care facilities are also more likely to experience depression and require more assistance with their activities of daily living (such as personal hygiene, movement, eating) than those without dementia.
Canadians age 65+ living in long-term care facilities with dementia are also more likely to encounter potentially inappropriate use of antipsychotics (23% versus 10%) and daily physical restraint use (6% versus 2%) than people without dementia. Potentially inappropriate use of antipsychotics indicates how many long-term care residents are taking antipsychotic drugs without a diagnosis of psychosis. Restraints are sometimes used to manage behaviours or to prevent falls; the data points below measure the percentage of residents that are in daily physical restraints.Footnote 27
| Data point | Percentage (%) of Canadians age 65+ living with dementia in LTC in 2019-20 | Percentage (%) of Canadians age 65+ without dementia in LTC in 2019-20 |
|---|---|---|
| Signs of depression (Depression Rating Scale [DRS] ≥3) | 26% | 21% |
| Dependence in activities of daily living (Activities of Daily Living Hierarchy Scale ≥3) | 85% | 80% |
| Wandered at least once in the last 7 days | 20% | 4% |
| Any responsive behaviours (Aggressive Behaviour Scale [ABS] ≥1) | 48% | 24% |
| Potentially inappropriate antipsychotic use | 23% | 10% |
| Use of daily physical restraints | 6% | 2% |
Focusing on those at higher risk and facing barriers to equitable care
As work continues to address dementia-related challenges across Canada, there is growing attention and recognition that some populations are more likely to face a higher risk of developing dementia and / or face barriers to obtaining dementia care. Many organizations are focusing on these populations and more data is being gathered to better inform initiatives going forward. As research and evidence grows, it is likely that additional populations will be identified as needing prioritization.
This year's report shares information about a variety of initiatives that reach Indigenous peoples, transgender and non-binary individuals, official language minority communities, and rural and remote communities, as examples of efforts with a focus on those at greater risk. It also includes a spotlight on how the Dementia Community Investment is providing targeted funding to support these populations.
Populations identified as more likely to face barriers to equitable care and / or are at higher risk of developing dementia include:
- Women
- Indigenous peoples
- Ethnic and cultural minority communities
- LGBTQ2IS individuals
- Official language minority communities
- Individuals with intellectual disabilities
- Individuals with young onset dementia
- Rural and remote communities
- Individuals with existing health issues or health behaviours known to be risk factors for dementia
Focusing on individuals and communities at higher risk and facing barriers to equitable care: Initiatives across Canada
Exploring the experiences of transgender and non-binary adults living with dementia
Marjorie Silverman and Alexandre Baril, at the University of Ottawa, will be interviewing trans older adults and their caregivers across Canada, to understand the experiences of transgender and non-binary older adults who are living with dementia and will offer recommendations that will benefit trans communities, practitioners, policy makers, and community organizations.
Monitoring the health status of Indigenous older adults and Indigenous peoples
The Morning Star Lodge, in collaboration with the File Hills Qu'Appelle Tribal Council and AGE-WELL researcher Megan O'Connell from the University of Saskatchewan, is introducing three new technologies that can be used to monitor diabetes, blood pressure, and body composition of older adults in Indigenous communities. This research aims to monitor the health status of older adults living with multiple health conditions to promote healthy behaviours and lifestyles and prevent dementia.
Exploring dementia-related stigma in Indigenous communities
The Native Women's Association of Canada (NWAC) is building capacity to conduct an awareness initiative through the Stigma: An Exploration of Lived Experiences, Understandings and Behaviours of Dementia within Indigenous Communities project. NWAC's goal is to develop an understanding of the needs, attitudes, and behaviours of Indigenous communities surrounding stigma and dementia using an Indigenous-led approach. The project is designed to capture the distinct aspects of dementia among First Nations, Inuit and Métis communities across Canada to support future awareness work to reduce stigma and encourage dementia-inclusive communities.
"Indigenous people living with dementia may go undiagnosed due to stigma and a lack of knowledge and access to adequate health care, and culturally inclusive diagnosis methods. To achieve the greatest impact, community engagement and education efforts must target stigma, and be tailored to meet the distinct and diverse needs of First Nations, Inuit and Métis peoples." – First Nations participant in the capacity building project, NWAC, 2020
Supporting aging in northern and rural communities
The Centre for Technology Adoption for Aging in the North (CTAAN) supports aging in northern and rural communities by making technologies more available to older adults, caregivers, and the health care systems that support them. Built on a partnership between UNBC, Northern Health, and AGE-WELL, and led by Richard McAloney and Shannon Freeman, the program helps companies pilot, implement, and promote new and existing technology solutions to these communities. Through partnerships and collaborations with local residents, researchers, and companies, CTAAN is building a permanent, accessible bridge to span the gap between older persons in northern and rural communities and the technology that can support them.
"CTAAN aims to reduce the barriers to using and accessing technology for people living with dementia in rural and northern BC communities to enhance daily living, safety, and facilitate social connection." – Richard McAloney, Director, Centre for Technology Adoption for Aging in the North (CTAAN)
Providing training to care providers in rural and remote communities on person-centred approaches
Canadian Remote Access for Dementia Learning Experiences (CRADLE) is a free online course on dementia care for personal care workers (PCW) in rural and remote areas, working in long-term care, retirement, and home and community settings across Canada. Led by Veronique Boscart at Conestoga College, CRADLE examines the impact of various education delivery approaches on different demographic and sector needs, and explores how to maximize workplace engagement of equity-seeking groups (such as newcomers to Canada working as PCWs, PCWs aged 50+ years, and PCWs working in remote and rural communities) by offering CRADLE in four languages to support learning in one's first language, providing guidance on how to support dementia care in rural and remote areas, exploring cultural considerations for dementia care, and investigating future opportunities for support.
"Unregulated care workers who have completed the CRADLE course appreciated being able to build their expertise in their own time, using engaging content that immerses them in relatable scenarios that promote practical approaches to person-centred dementia care across care settings, including in rural and remote communities." – Veronique Boscart, Executive Dean for the School of Health & Life Sciences at Conestoga College
Enhancing the capacity of primary health care teams in rural communities
The Primary Health Care Integrated Geriatric Services Initiative in Alberta aims to increase the capacity of multi-sector community teams to provide care and support for those affected by dementia. During the demonstration phase (2017-2019), a series of educational workshops provided practical information on topics ranging from timely recognition of dementia to end-of-life care. The provincial team is now working with five rural communities to develop a Wellbeing Guide for community teamsto support monitoring wellbeing outcomes of people affected by dementia, and a Competency Framework to help identify the skills and knowledge needed within community teams to support people affected by dementia.
Supporting rural Francophone caregivers
A support system in the Chaleur Region of New Brunswick is being developed for caregivers of at risk seniors, including those living with dementia and includes research to identify needs and to help caregivers continue to provide care. This project will use a community-based and inclusive approach to address social inequalities and challenges faced by caregivers in rural Francophone settings supporting older Canadians living at home.
The Dementia Community Investment: Supporting individuals at higher risk and facing barriers to equitable care
Recognizing that there are populations within Canada that are more at risk of developing dementia and/or face barriers to care, the Government of Canada's Dementia Community Investment (DCI) seeks to identify projects that support such populations through the development of tools and resources that meet their specific needs. All DCI funded projects report on the impact of their work, including on these populations to help better understand the effectiveness of their interventions. Below are several examples of DCI projects with a focus on these populations.
The COSTI project is building on an existing day program in Toronto for people living with dementia and caregivers by including specialized activities and education programming that reflect their cultural heritage, beliefs and values. COSTI's project advisory committee guides its work involving diverse stakeholders, including community organizations that represent South Asian, Chinese and Italian populations in Toronto. The project has also completed a scan of resources and a curriculum of activities available for caregivers to determine what resources and services currently exist for these populations. Furthermore, in partnership with Centre for Addiction and Mental Health, COSTI is working on producing culturally relevant and language specific resources on mental health and addictions to support older adults with dementia.
"Having the opportunity to provide input into a program curriculum designed specifically for my language and culture made me feel that I could contribute to my dad's wellbeing. I want to continue the gains my dad made at his senior's day program at home, especially during COVID-19, and celebrate his heritage and have him tell me stories again." – Maria DiNardo, caregiver participant COSTI Seniors day program
Lakehead University's Dementia Dialogue Podcast Network showcases the diverse experiences of dementia through podcasts, from the perspectives of both people living with dementia and caregivers. To date, podcasts have helped to increase awareness, sensitivity and understanding of dementia and the lived experience. This project will also engage with different communities and populations (e.g., First Nations communities, linguistic minority communities, and LGBTQ2IS communities) to ensure that a diversity of experiences are developed and shared.
Research shows that LGBTQI2S seniors are at a greater risk than heterosexual peers of experiencing risk factors (e.g., social isolation) for developing dementia. Moreover, there is both a lack of knowledge and understanding about the specific experiences of this population with dementia and few tailored tools and resources to meet their needs. EGALE's dementia study, "The integration, optimization, and promotion of inclusive approaches to supporting LGBTQI2S people living with dementia and their unpaid primary carers", engages with members of the LGBTQ2S community to better understand their needs, develop and evaluate tools and resources, and undertake a national awareness campaign to share the experiences of this population and the tools developed.
Two projects are being led by the Inuvialuit Regional Corporation (IRC) and the Native Women's Association of Canada (NWAC) to address the needs of caregivers of Indigenous peoples living with dementia. NWAC is developing tailored, culturally safe and trauma informed resources and supports (e.g., fact sheets) for Indigenous women who are caring for individuals living with dementia in rural and remote communities in Nunavut, Saskatchewan, Ontario and the Maritimes. To date, despite the challenges of COVID-19, NWAC has interviewed Indigenous women caregivers (First Nations, Inuit and Métis) and found that there is a need to incorporate cultural practices into supports for Indigenous caregivers and into care provided to Indigenous people living with dementia, particularly in formal settings. Similarly, the IRC is working towards developing culturally sensitive educational resources for caregivers that will also be shared with health professionals caring for Inuit elders.
Three other projects also focus on addressing unique needs and developing culturally appropriate resources for Indigenous populations. The University of Manitoba is developing programming to: help informal caregivers and people living with dementia lead happy and fulfilling lives; mitigate risk factors related to dementia in the community; and mobilize knowledge by developing training materials that can be shared with other Indigenous communities. Saint Elizabeth Health is building on existing work to strengthen the partnership between the person living with dementia, caregiver and care provider. To date, co-design workshops with three Indigenous communities in Northern Ontario and one rural community in B.C. have taken place to produce culturally sensitive adaptations of a prototype tool in the form of a journal. The journal is being transformed into an app to increase access to the tool. The Centre de recherche sur le vieillissement de Sherbrooke is working to foster dementia inclusiveness in First Nations and non-First Nations communities in Quebec to enable people living with dementia to stay at home and continue to engage with their community. To date, the project has formed a local advisory committee in Sherbrooke and has established an agreement with Wendake Nation to begin similar work in this community.
Data points on those at higher risk and facing barriers to equitable care
This year's report shares public opinion research that increases our understanding about populations identified as being likely to be at a higher risk of developing dementia and / or facing barriers to dementia care, supports, and services. The data points below focus on responses from Indigenous individuals, ethnic and cultural minority communities and rural and remote populations.
Preventing dementia
The table below suggests that compared to the general population, the selected populations generally have a similar level of awareness of at least one risk factor linked to dementia. There are slightly larger differences across responses regarding views related to dementia as an inevitable part of aging and whether individuals had taken steps to intentionally reduce their risk of developing dementia.
| POR Data Point: Prevention | General population | First Nations | Métis | Inuit | South Americans | South Asians | East Asians | Black Canadians | Rural | Remote |
|---|---|---|---|---|---|---|---|---|---|---|
| % Canadians who felt that dementia is an inevitable part of aging. | 22 | 18 | 7 | 30 | 28 | 27 | 27 | 34 | 16 | 28 |
| % Canadians who are aware of at least one risk factor | 89 | 93 | 93 | 86 | 100 | 96 | 87 | 95 | 89 | 81 |
| % of Canadians who have taken steps to reduce their risk of developing dementia in the last year | 22 | 27 | 31 | 6 | 34 | 29 | 29 | 28 | 17 | 20 |
Note: Please use caution when interpreting Inuit data from the PHAC 2020 Baseline Public Opinion Research on dementia due to the small sample size. |
||||||||||
Improving the quality of life of people living with dementia and caregivers
Results from the 2020 baseline public opinion research on dementia suggest that, compared to the general population, some populations vary notably in their agreement that people living with dementia will experience a lower quality of life than people without dementia. As well, there is some variation on whether the respondent feels comfortable interacting with someone living with dementia.
| POR Data Point: Quality of life | General population | First Nations | Métis | Inuit | South Americans | South Asians | East Asians | Black Canadians | Rural | Remote |
|---|---|---|---|---|---|---|---|---|---|---|
| % of Canadians who agree with the perception that people living with dementia generally face a lower quality of life than people without dementia | 70 | 67 | 77 | 61 | 79 | 76 | 71 | 56 | 65 | 67 |
| % of Canadians who expressed not being fully comfortable interacting with someone with dementia | 46 | 42 | 38 | 59 | 46 | 49 | 62 | 46 | 42 | 37 |
Note: Please use caution when interpreting Inuit data from the PHAC 2020 Baseline Public Opinion Research on dementia due to the small sample size. |
||||||||||
Conclusion
The 2021 annual report to Parliament on the national dementia strategy highlights collective efforts underway across Canada towards addressing the many challenges of dementia, along with responses to the significant impact of COVID-19 that have helped to support people living with dementia and caregivers during this remarkable and difficult experience. Many heroic efforts have been made by organizations and individuals to help Canadians through this unique and challenging time. Looking ahead, it is clear that the pandemic will continue to shape many aspects of dementia-related work, including a sharpened focus on long-term care. The distressing situation encountered by older Canadians in many of Canada's long-term care facilities during the pandemic has drawn greater attention to the need for improvements in the care being provided across the country.
The efforts of organizations and individuals across Canada provide reason to be optimistic about the ability to continue to make a difference and advance progress on the strategy's national objectives and its aspirations. For example, a new collaborative research and development program from the National Research Council, the Aging in Place Challenge Program, which began in 2021, aims to reduce the number of older adults (65+) who require facility-based care by 20% by 2031. Over the next seven years, the program will focus on improving the quality of life of older adults, including people living with dementia, and support caregivers through innovation and technologies that will support safe and healthy aging. An initial group of projects has been identified and there will be future opportunities for potential collaborators. To move forward, it is also important to share results and lessons learned. One example of efforts to share valuable information is the new knowledge hub supported through PHAC's Dementia Community Investment (DCI). This hub will facilitate knowledge sharing and collaboration between the DCI's community-based projects and will identify and share resources, lessons learned and best practices to the broader dementia policy and program community so that people living with dementia and caregivers across Canada can benefit.
We thank all organizations across Canada that contributed information to this year's report and encourage them to keep us informed about their important dementia-related work, including significant updates. If you would like to receive communications about the national dementia strategy and funding opportunities, or provide information about relevant dementia activities, please contact the PHAC Dementia Policy Secretariat.
Appendix: Aspirations for Canada's efforts on dementia from the national dementia strategy
| Current status | Aspiration | |
|---|---|---|
| Prevent dementia | ||
| 1 | Incomplete understanding of risk and protective factors linked with dementia, with some factors not yet identified and insufficient evidence on the link between factors and dementia. | A complete understanding of the risk and protective factors linked to dementia, their impacts and interactions. |
| 2 | Limited evidence about effective interventions to reduce risk for dementia and insufficient information resources. | Availability of effective prevention resources and interventions, supported by a strong evidence base. |
| 3 | A lack of awareness among the general public and care providers about actions that may help prevent dementia. | All people living in Canada are aware of actions that prevent dementia. |
| 4 | Barriers related to built and social environments limit the ability of individuals to pursue healthy living in ways that may reduce the risk of developing dementia. | All people living in Canada have access to built and social environments that support their ability to pursue healthy living in ways that may reduce their risk of developing dementia. |
| Advance therapies and find a cure | ||
| 1 | Limited broad stakeholder input when setting research priorities and insufficient engagement of people living with dementia and caregivers. | Research priorities established in an inclusive manner with broad stakeholder input, with the participation of those living with dementia and caregivers. |
| 2 | Annual investment in dementia research in Canada is less than one percent of dementia care costs. | Annual investment in dementia research in Canada exceeds one percent of dementia care costs. |
| 3 | Options for evidence-informed therapies remain limited and often are not person-centred. | New evidence-informed person-centred therapies are more readily available. |
| 4 | People living with dementia and caregivers are predominantly the subject of research to develop new therapies and find a cure. | People living with dementia and caregivers are active participants and partners in research to develop new therapies and find a cure. |
| 5 | Research findings tend to stay within academic settings and journals and are not broadly known, accepted, or brought into clinical practice. | Research design always includes efforts that ensure findings can be understood, adopted and quickly put into practice. |
| Improve quality of life of people living with dementia and caregivers | ||
| 1 | Widespread stigma within communities and a lack of understanding of dementia. | All people living in Canada understand dementia and stigma no longer exists in Canada. |
| 2 | Individuals are unable to receive an early or timely diagnosis, or feel unsupported when receiving a diagnosis. | A timely diagnosis, provided in a compassionate manner, is available to all people living in Canada, along with immediate availability of resources and supports. |
| 3 | Lack of access to, awareness or understanding of health and social services that provide integrated and person-centred care. | Integrated, person-centered quality care based on evidence-informed best practices across all settings and that people feel welcomed and well-cared for when hospitalization or admission to long-term care is necessary. |
| 4 | Lack of information and resources for care providers, reducing the capacity to provide quality care. | Care providers have access to the resources and training needed to deliver quality care. |
| 5 | Caregivers experiencing burnout, financial hardship, isolation and depression while caring for someone living with dementia. | All caregivers have access to the resources and supports required to protect their own wellbeing and to care for someone living with dementia, including being equipped to navigate health care and other support systems. |
Bibliography
Batsis JA, Daniel K, Eckstrom E, et al. Promoting healthy aging during COVID‐19. Journal of the American Geriatrics Society. 2021; 69: 572-580.
Canadian Institute for Health Information. Dementia in Canada. Canadian Institute for Health Information. 2021.
Canadian Institutes of Health Research. COVID-19 and dementia: Research to improve care for older adults across Canada. Canadian Institutes of Health Research. 2020.
Canadian Society for Exercise Physiology. Canadian 24-hour movement guidelines for adults ages 65 years and older: An integration of physical activity, sedentary behaviour, and sleep. Canadian Society for Exercise Physiology. 2020.
Ekos Research Associates Inc. for the Public Health Agency of Canada. Dementia survey 2020. Government of Canada. 2020.
Embracing Carers. The Global Carer Well-Being Index: Who cares for carers? Perspectives on COVID-19 pressures and lack of support. Embracing Carers.
Gosse P, Kassardjian C, Masellis M, Mitchell S. Virtual care for patients with Alzheimer disease and related dementias during the COVID-19 era and beyond. CMAJ. 2021;193(11):E371-E377.
Government of Canada. People who are at risk of more severe disease or outcomes from COVID-19. Government of Canada. 2020.
Livingston G, Huntley J, Sommerlad, A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet. 2020;396(10248):413-446.
McGhan G, McCaughey D, Hindmarch W, Flemons K. Caring for caregivers - Data report for Calgary pilot study summer 2020: The impact of COVID-19 on family caregivers for persons living with dementia. The University of Calgary. 2020.
Numbers K, Brodaty H. The effects of the COVID-19 pandemic on people with dementia. Nature Reviews Neurology. 2021;17:69-70.
Preliminary data from Earnscliffe's Quality of Life and Dementia for the Public Health Agency of Canada.
Preliminary data from Ekos Research Associates Inc.'s Knowledge, Perspectives and Experience of Dementia Care Providers for the Public Health Agency of Canada.
Public Health Agency of Canada. A dementia strategy for Canada: Together we aspire. Government of Canada. 2019.
Public Health Agency of Canada. Dementia. Government of Canada. 2021.
Public Health Agency of Canada. Dementia in Canada. Government of Canada. 2019.
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017.
Public Health Agency of Canada. From risk to resilience: An equity approach to COVID-19. Government of Canada. 2020.
Public Health Infobase. Canadian Chronic Disease Surveillance System (CCDSS). Government of Canada. 2019.
Statistics Canada. Provisional death counts and excess mortality, January 2020 to February 2021. Government of Canada. 2021.
Tahira AC, Verjovski‐Almeida S, Ferreira ST. Dementia is an age‐independent risk factor for severity and death in COVID‐19 inpatients. Alzheimer's & Dementia. 2021;1‐ 14.
Taquet M, Geddes J, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021;8(5):416-427.
Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2021;8(2):130-140.
The Alzheimer Society of Canada. The COVID-19 and Dementia Task Force. The Alzheimer Society of Canada.
Webster P. COVID-19 highlights Canada's care home crisis. The Lancet. 2021;397(10270):183.
World Dementia Council. Global dialogue on biomarkers and treatments: Reflections. World Dementia Council. 2021.Endnotes
- Footnote 1
-
Between March 1, 2020, and February 15, 2021, more than 2,500 care homes across the country experienced a COVID-19 outbreak, resulting in the deaths of over 14,000 residents and close to 30 staff. This represents more than two-thirds of Canada's overall COVID-19 deaths.
- Footnote 2
-
Please note that some of the websites this report links to may not have content in both English and French.
- Footnote 3
-
Paul Webster, COVID-19 highlights Canada's care home crisis, The Lancet, Volume 397, Issue 10270, 2021, Page 183, ISSN 0140-6736, https://doi.org/10.1016/S0140-6736(21)00083-0. https://www.sciencedirect.com/science/article/pii/S0140673621000830
- Footnote 4
-
This definition of dementia is based on a combination of commonly used sources.
- Footnote 5
-
Provisional death counts and excess mortality, January 2020 to February 2021. Statistics Canada. February 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210514/dq210514c-eng.htm
- Footnote 6
-
Dementia in long term care. Canadian Institute for Health Information. June 2018. https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-long-term-care
- Footnote 7
-
The Global Carer Well-Being Index: Who Cares for Carers? Perspectives on COVID-19 Pressures and Lack of Support. https://www.embracingcarers.com/content/dam/web/healthcare/corporate/embracing-carers/research/global-carer-well-being-index/Global-Carer-Well-Being-Index-Report_FINAL_with-EMD-Serono-logo.pdf
- Footnote 8
-
COVID-19 and dementia: Research to improve care for older adults across Canada. Canadian Institutes of Health Research. https://cihr-irsc.gc.ca/e/52198.html
- Footnote 9
-
Caring for Caregivers - Data Report for Calgary Pilot Study Summer 2020: The Impact of COVID-19 on Family Caregivers for Persons Living with Dementia https://static1.squarespace.com/static/56f1ce474c2f85b03ad91d5c/t/5fb806ee0238471c6538b11e
/1605895944452/FCG+Pilot+Study+Report+FINAL.pdf - Footnote 10
-
Final results are anticipated in September 2021.
- Footnote 11
-
A care provider is a person who provides care and support to a person with dementia, in a paid or unpaid role. While a caregiver is defined as a person who provides care and support to a person with dementia, and who is not a paid care professional or personal care worker. A caregiver is likely to be a relative, close friend, neighbour or volunteer.
- Footnote 12
-
Virtual care for patients with Alzheimer disease and related dementias during the COVID-19 era and beyond. Paula J. Gosse, Charles D. Kassardjian, Mario Masellis, Sara B. Mitchell. CMAJ Mar 2021, 193 (11) E371-E377; DOI: 10.1503/cmaj.201938
- Footnote 13
-
Dementia prevention, intervention, and care: 2020 report of the Lancet Commission
- Footnote 14
-
Respondents were asked about their knowledge of risk factors linked to dementia. Many Canadians correctly believe that factors such as loneliness and social isolation (64%), harmful alcohol use (58%), lack of physical activity (54%), having had a stroke (54%), a diet lacking in nutrition (53%), and sleep disruption (50%) are linked to increased chances of developing dementia. Just under half (46%), however, also believe that exposure to toxic chemicals increases the propensity of developing dementia, which is not strongly substantiated by the evidence and is not commonly linked with dementia. About one-third of Canadians perceive correctly that hypertension or high blood pressure (35%) or smoking (32%) increases the chances of developing dementia. Slightly fewer say that diabetes (27%), air pollution (21%), or high cholesterol (20%) increases the likelihood. Just over one-tenth believe that hearing loss (16%) or fewer years of formal education (13%) can increase the risk of developing dementia. Eleven percent are unsure of any factors that increase the chances of developing dementia, meaning that 89% of Canadians can correctly identify at least one or more risk factors.
- Footnote 15
-
EKOS' Dementia Survey 2020 for the Public Health Agency of Canada
- Footnote 16
-
This data is age-standardized and reflects the differences in Canada's age structure between the two years.
- Footnote 17
-
Public Health Agency of Canada. Dementia in Canada, including Alzheimer's disease: Highlights from the Canadian Chronic Disease Surveillance System. Government of Canada. 2017; https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-highlights-canadian-chronic-disease-surveillance.html
- Footnote 18
-
Percentages in green indicate that Canadians are moving in the right direction, based on a statistically significant change in the percentage. Percentages in yellow indicate that the percentage has remained unchanged or the change is not statistically significant, while percentages in red indicates a move in a negative direction. These trends were tested for statistical significance.
- Footnote 19
-
Figure 2 uses the most recent data available and historical data approximately five years back, where available, to describe the prevalence of known dementia risk and protective factors over time. Data for risk and protective factors is collected on an annual, biennial, or ad hoc basis.
- Footnote 20
-
The risk and protective factors for dementia in Figure 2 are selected based on available evidence as of June 2021. Sleep disturbance is a known risk factor for dementia, and while it is not included in Table 1 as it is not one of the 12 factors highlighted by the Dementia prevention, intervention, and care: 2020 report of the Lancet Commission, it is mentioned as a risk factor in that publication.
- Footnote 21
-
Public Health Agency of Canada. Upcoming 2017-2018 estimates in Canadian Chronic Disease Surveillance System (CCDSS) Data Tool 2019. Canada.ca. https://health-infobase.canada.ca/ccdss/data-tool/. Upcoming.
- Footnote 22
-
Internal data from the Canadian Institutes of Health Research.
- Footnote 23
-
This number includes an estimate of indirect trainees for applications where number of trainees were not directly reported. The estimate is calculated based on the amount spent on students divided by average students salaries, based on recent Canadian Institutes of Health Research internal data.
- Footnote 24
-
Dementia prevention and treatment. https://www.cihi.ca/en/dementia-in-canada/spotlight-on-dementia-issues/dementia-prevention-and-treatment
- Footnote 25
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the RAI Home Care (RAI HC)-HCRS, fiscal year 2019-20. It is representative of people living with dementia receiving homecare in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.
- Footnote 26
-
There has not been a significant increase in people living with dementia receiving home care experiencing withdrawal from activities of interest and/or reduced social interaction or a potential or actual problem with depression between 2018-19 and 2019-20. Data was collected up to March 31, 2020.
- Footnote 27
-
The 2019-2020 data presented here was obtained from the Canadian Institute for Health Information Continuing Care Reporting System (CCRS) which includes continuing care facilities from Newfoundland and Labrador, Ontario, Manitoba, Alberta, British Columbia and Yukon.
- Footnote 28
-
Signs of depression measured using the Depression Rating scale (DRS). The DRS is a scale intended to screen for depression among residents of continuing care facilities and ranges from 0 to 14, with higher values indicating the resident has more, numerous and/or frequent symptoms.
Dependence in activities of daily living using the Activities of Daily Living (ADL) Hierarchy Scale: The ADL Hierarchy Scale groups activities of daily living according to the stage of the impairment process in which they occur. Early loss of ADLs (i.e. dressing) are given lower scores than late loss of ADLs (i.e. eating). The ADL Hierarchy ranges from 0 (no impairment) to 6 (total dependence).
Responsive behaviors measured using the Aggressive Behaviour Scale (ABS): The ABS is a measure of aggressive behaviour based on the occurrence of verbal abuse, physical abuse, socially disruptive behaviour and resistance of care. Scores range from 0-12 with higher scores indicating greater frequency and diversity of aggressive behaviour. Scores of 1 to 4 on the ABS indicates mild to moderate aggressive behaviour, whereas scores of 5 or more represent the presence of more severe aggression.