A Dementia Strategy for Canada: Together We Achieve - 2020 Annual Report

Download the alternative format
(PDF format, 4.3 MB, 64 pages)
Organization: Public Health Agency of Canada
Date published: 2020-12-07
Table of contents
- Minister’s message
- Introduction
- Annual spotlight: Highlights of Canada’s dementia research
- Working together towards the three national objectives
- National objective: Prevent dementia
- National objective: Advance therapies and find a cure
- National objective: Improve the quality of life of people living with dementia and caregivers
- Cross-cutting efforts
- Conclusion
- Appendix A: Aspirations for Canada’s efforts on dementia
- Appendix B: Efforts across Canada
- Bibliography
- Endnotes
Minister’s message
I am pleased to share the second annual Report to Parliament on Canada’s national dementia strategy, A Dementia Strategy for Canada: Together We Aspire. The strategy was written to inspire all Canadians and relies on our collective efforts to move forward on its three national objectives. We know that dementia impacts the lives of many Canadians. Three-quarters of those responding to the Public Health Agency of Canada’s 2020 baseline survey say they have known someone living with dementia, while about one-third have provided care or assistance within the last five years to someone living with dementia, often a close family member or friend.
Recent months have brought the unprecedented challenge of COVID-19 into the lives of all Canadians, creating worry and sorrow for many Canadian families. For people living with dementia and their caregivers, we know that it has been especially difficult. The Government of Canada has sought to provide help to Canadian families, seniors, and the health care system, adjusting our efforts as we learn more about COVID-19 and how best to support Canadians. One example is the $350M in funding announced in April 2020 that recognizes the disproportionate impact of COVID-19 on more Canadians. The Emergency Community Support Fund, delivered by national charitable and non-profit organizations is intended to assist, for example, with home deliveries of groceries and medications, providing transport services and help with accessing government benefits. Going forward, the Government will continue to assess how federal initiatives, including those focused on dementia, can best support Canadians in managing the risks of COVID-19 and recover from its impact.
In 2019, the Government of Canada announced more than $81 million over 5 years to fund dementia awareness, surveillance, guidance on diagnosis and treatment, and research. This is in addition to over $200 million already invested in the last five years to advance research on dementia and support community-based projects. The Government will also continue to support collaboration including the sharing of information and best practices that is critical to our collective progress toward achieving our shared vision of a Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated.
At the Public Health Agency of Canada, efforts in the first year of the national dementia strategy focused on laying a strong foundation for its implementation. This ongoing work includes investing in new dementia initiatives on awareness raising, guidance, and data gathering. For example, later this year, we expect to launch several projects with partners on awareness raising. As well, to guide the focus of investment going forward, public opinion research was conducted in early 2020 to better understand the views and level of knowledge of Canadians about dementia with a focus on prevention and stigma reduction. We also have invested in community-based dementia initiatives.
This annual report provides examples of the work done every day by many organizations and dedicated individuals across Canada that support the strategy’s three national objectives: improving the quality of life of people living with dementia and dementia caregivers, advancing therapies and finding a cure, and supporting the ultimate goal of preventing dementia. Thank you to all those across Canada who are advancing the important work on dementia including provincial and territorial governments, advocacy organizations, care providers, academics and researchers, and community organizations. These collective efforts put us on the right track in moving ahead on the strategy’s national objectives while we continue to identify gaps and set priorities for future work. Over time, as the strategy continues to guide these efforts, its contribution will grow.
The Honourable Patty Hajdu
Minister of Health
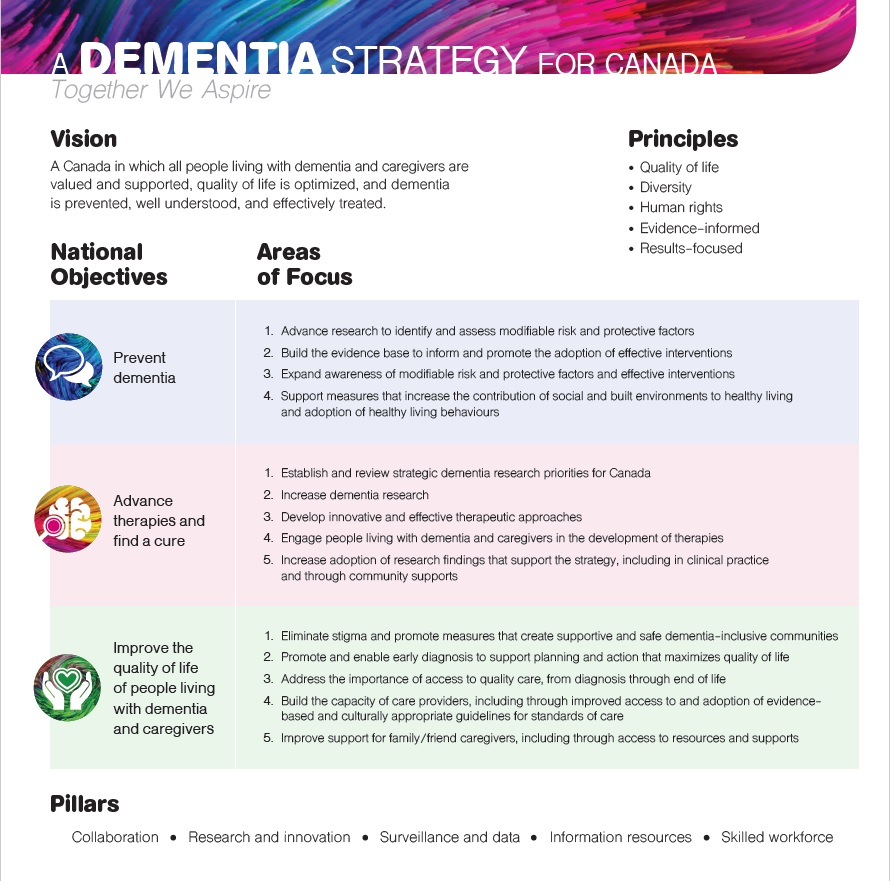
Figure 1 - Text Equivalent
This image is a visual depiction of the core elements of the strategy.
The title of the strategy appears at the top "A dementia strategy for Canada: Together we aspire".
Below this the Vision is stated which is "A Canada in which all people living with dementia and caregivers are valued and supported, quality of life is optimized, and dementia is prevented, well understood, and effectively treated".
Next to the vision, the principles are displayed in a bulleted list: Quality of life, Diversity, Human rights, Evidence-informed, and Results-focused.
Below the principles are a table with a row for each of the National Objectives and their corresponding Areas of Focus.
In the second row is the objective of "Advance therapies and find a cure".
- Advance research to identify and assess modifiable risk and protective factors,
- Build the evidence base to inform and promote the adoption of effective interventions,
- Expand awareness of modifiable risk and protective factors and effective interventions,
- Support measures that increase the contribution of social and built environments to healthy living and adoption of healthy living behaviours.
In the second row is the objective of "Advance therapies and find a cure".
The corresponding Areas of Focus are:
- Establish and review strategic dementia research priorities for Canada,
- Increase dementia research,
- Develop innovative and effective therapeutic approaches,
- Engage people living with dementia and dementia caregivers in the development of therapies,
- Increase adoption of research findings that support the strategy, including in clinical practice and through community supports.
In the third row is the objective of "Improve the quality of life of people living with dementia and caregivers". The corresponding Areas of Focus are:
- Eliminate stigma and promote measures that create supportive and safe dementia-inclusive communities,
- Promote and enable early diagnosis to support planning and action that maximizes quality of life,
- Address the importance of access to quality care, from diagnosis through end of life,
- Build the capacity of care providers, including through improved access to and adoption of evidence-based and culturally appropriate guidelines for standards of care,
- Improve support for family/friend caregivers, including through access to resources and supports.
At the bottom of the image (underneath the National Objectives/Areas of Focus table), the Pillars of the strategy are listed in one line separated by dots. The pillars are:
- Collaboration
- Research
- Innovation
- Surveillance and data
- Information resources
- Skilled workforce
Introduction
Reporting on dementia in Canada
Canada’s first national dementia strategy launched in June 2019, A Dementia Strategy for Canada: Together We Aspire, sets out ambitious aspirations for the future of dementia in Canada. Footnote 1 Its broad scope reflects and encompasses the many priorities heard during consultations. The degree of its impact relies on our collective efforts, making it important to call on all Canadians and organizations to contribute towards its three national objectives focused on preventing dementia, advancing therapies and finding a cure, and improving quality of life for people living with dementia and caregivers. It recognizes five essential and cross-cutting pillars that support all work on dementia and sets out principles to guide our collective efforts.
The strategy places a strong emphasis on furthering our national effort to understand how best to prevent dementia including taking action on reducing risks, while also placing effective treatments and improved quality of life for people living with dementia at its centre. It calls attention to the importance of supporting and protecting the health and quality of life of the family and friends who often bear the primary responsibility for providing care for people living with dementia. These caregivers are too often experiencing distress and jeopardizing their own wellbeing as a result of their commitment to the quality of life of their loved ones. Footnote 2 It also notes the importance of understanding the needs of populations and individuals at higher risk and/or facing barriers to care and ensuring our efforts are tailored in ways that best support them.
The principles included in the strategy encourage Canadians to work together to achieve progress on dementia while learning from and building on collective efforts. They remind us that human rights are at the core of the strategy, and that actions in support of the strategy must reflect the diversity within Canada, be informed by evidence and be designed to support and measure the intended results.
Text box 1: What is dementia?
Dementia is a term used to describe symptoms affecting brain function. It may be characterized by a decline in cognitive abilities such as: memory; planning; judgement; basic math skills; and awareness of person, place and time. Dementia can also affect language, mood and behaviour, and the ability to maintain activities of daily living (PDF).
Dementia may be caused by neurodegenerative diseases (affecting nerve cells in the brain), vascular diseases (affecting blood vessels like arteries and veins) and injuries. Types of dementia include vascular, Lewy body, frontotemporal, Alzheimer’s disease and mixed. In rare instances, dementia may be linked to infectious diseases, including Creutzfeldt-Jakob disease, or caused by injuries.
This definition of dementia is based on a combination of commonly used sources.
This 2020 annual report to Parliament on the national dementia strategy is the first report sharing a Canada-wide overview of some of the efforts underway. Footnote 3 This report provides a few highlights of how many different organizations, including the federal government, are supporting the strategy’s national objectives and reflects the variety of those efforts. Footnote 4 The Public Health Agency of Canada (PHAC) continues to gather information on dementia-related activities across the country as effective implementation requires a thorough understanding of Canada’s collective efforts on dementia. Information gathering will help to better understand the impact of efforts over time that are aligned with the strategy’s national objectives and to identify where greater efforts are needed.
The report sets out data points to provide a snapshot of some aspects of the state of dementia in Canada. Tracking data points over time will help our efforts to assess how we are doing as a country in making progress on the national objectives and in moving closer to the aspirations set out in the national dementia strategy. To improve the data available about dementia in Canada, PHAC commissioned a national public opinion survey of about 4,200 Canadians in early 2020. Footnote 5 This survey measured general awareness as well as knowledge about risk reduction, attitudes about seeking and sharing information about a dementia diagnosis, views on the abilities of people living with dementia, and experiences with providing care. It also provides insights into differences in knowledge and attitudes across regions and within different demographic groups. It found that 83% of respondents believe dementia is having a moderate to significant impact in Canada today. About half of respondents worry about developing dementia themselves (49%) and almost two-thirds worry that someone close to them will develop dementia (64%).
While there are several existing data sources for dementia in Canada, gaps remain in certain areas making it a priority to improve data. As the dementia strategy is implemented, PHAC will continue to work with key stakeholders and partners to build on and develop new data that will help to shed further light on who is most impacted and most at risk of developing dementia. For example, to inform future priorities for dementia research in Canada, it is important to have more comprehensive data on the full scope of current dementia research efforts and how research is being translated into practice. Improving the ability to assess the quality of life of people living with dementia in Canada as well as caregivers is also a priority and is likely to require data from a variety of sources. Quality of life includes access to a variety of treatments, reducing stigma and taking steps for communities to be more welcoming and inclusive of those living with dementia. Priorities for data gaps going forward will also include identifying and pursuing ways to improve what we know about populations at higher risk of developing dementia and those facing barriers to care.
The Public Health Agency of Canada is collaborating with the provinces, territories and other stakeholders to explore new approaches to collecting data on topics such as undiagnosed dementia, dementia comorbidities, and dementia in long-term care settings. PHAC’s partners will implement these projects over the next four years using existing provincial datasets or by conducting new data collections. New investments in dementia surveillance will also help all stakeholders better understand the scope of dementia in Canada and will inform work related to policies, programs and services.
Text box 2: Dementia by the numbers
- As of 2016-17, more than 432,000 Canadians aged 65 years and older—or 6.9%—were living with diagnosed dementia
- Two-thirds of those diagnosed with dementia are women.
- The risk of being diagnosed with dementia doubles with every 5-year increase in age between 65 and 84 years.
- The annual health care cost for Canadians affected by dementia was $8.3 billion in 2011. It was projected in 2016 that this cost would double to $16.6 billion by 2031.
Text box 3: The impact of COVID-19 on people living with dementia and caregivers
COVID-19 has created new challenges for people living with dementia and caregivers and requires tailoring of responses to address those needs. Some of the early challenges identified for people living with dementia and caregivers include:
- Physical distancing may disproportionately affect people living with dementia because they depend primarily on in-person support, are extremely sensitive to disruptions to their daily routines, and may have very low technological literacy to stay connected with friends and family.
- Some people living with dementia may have difficulties remembering safeguard procedures such as regularly and thoroughly handwashing or understanding public health information and guidance, which could expose them to higher risk of infection.
- Given the recent occurrence of COVID-19, there has not been adequate opportunity to assess impacts of COVID-19 on people living with dementia. However, 90 percent of those living with this condition have at least one other chronic condition and nearly 20 percent have five or more health conditions, which may increase their risk for severe symptoms and death.
- COVID-19 is placing enormous additional pressure on family/friend caregivers who may already be feeling stretched and stressed. Key caregiver challenges include:
- Lack of respite care and closures of day programs;
- Concerns about loved ones living in long-term care facilities;
- Restrictions on being able to see their loved ones who are living in facilities;
- Moving their loved ones temporarily back home to reduce the risk of transmission; and,
- Juggling children and work at home at the same time as continuing or increasing caregiver responsibilities.
Annual spotlight: Highlights of Canada’s dementia research
Canadian researchers have been at the forefront of efforts to find effective ways to prevent and treat dementia and to improve the quality of life of people living with dementia and caregivers. Through the Canadian Institutes of Health Research (CIHR), the federal government has invested over $200M over the last 5 years (2014-15 to 2018-19) to support dementia research in Canada, some of which is described below. CIHR collaborates with partners across the country who are helping to put Canada at the forefront of dementia research. Many of these partners are also supporting research projects outside of what is highlighted here.
In June 2019, the Canadian Consortium on Neurodegeneration in Aging (CCNA) entered Phase II of its work with a renewed investment over five years. A major strategic initiative of the Canadian Institutes of Health Research (CIHR) since 2014, this pan-Canadian research network brings together more than 300 researchers and clinicians to advance an ambitious program of research that aligns with the national dementia strategy’s objectives of prevention, treatment, and quality of life. Through its research activities, the CCNA has made a commitment to meaningfully engage people living with dementia, support research on dementia care for Indigenous people, and conduct work in priority areas such as women and dementia. CCNA researchers continue to work on research ideas across each objective of the national dementia strategy such as those highlighted below.
Preventing dementia
CAN-THUMBS UP is a national platform being created during Phase II of the CCNA that will study new approaches to dementia prevention. There are at least 20 prevention interventions and/or combinations of interventions such as diet, physical exercise and brain training currently known that have the potential to slow cognitive decline and prevent some forms of dementia. This new platform will enable researchers to test the effectiveness of combining specific actions, expected to reduce the risk of dementia, on individuals who are at higher risk of developing dementia as they age.
Advancing therapies and finding a cure
Scientists across Canada continue to investigate potential cures for dementia. For example, Peter St. George-Hyslop at the University of Toronto is undertaking research to better understand the root causes of dementia and to identify specific factors that could be used to target treatments for dementia at the molecular level. As well, Sandra Black and her team at the Sunnybrook Research Institute are investigating new avenues for dementia treatment, such as the re-purposing of blood pressure lowering drugs for delaying dementia, the role of sleep problems in clearing brain waste products such as amyloid, and the potential use of focused ultrasound to deliver novel drug therapies to the brain.
A dedicated CCNA team led by Jennifer Walker at Laurentian University is continuing to advance research on issues related to dementia care for Indigenous populations. Team members from across Canada are working with communities: to improve ways to detect and diagnose dementia; to understand the connection among trauma, culture and dementia; and to develop culturally safe, trauma-informed approaches to addressing dementia. In 2019, a team of researchers led by Kristen Jacklin launched a Canadian Indigenous Cognitive Assessment (CICA) tool, which provides a culturally appropriate and safe tool for older Indigenous people. The tool is expected to improve diagnosis and care for Indigenous populations that are aging. The CICA has been validated with the Anishinaabe on Manitoulin Island, Ontario, and will be adapted for other communities across Canada, including the File Hills Qu’appelle Tribal Council in Saskatchewan and the diverse urban Indigenous community in Calgary.
Canadian researchers are also part of a three-year (2018-2021) Joint Programme on Neurodegenerative Disease Research (JPND) international project with Australia, the Netherlands, the United Kingdom and Poland to develop a new internationally adaptable set of recommendations and toolkits for people living with dementia, care partners, and health care practitioners on how to improve the diagnostic process and post-diagnostic care.
Improving the quality of life of people living with dementia and caregivers
Research is underway at the University of British Columbia to learn how communities can reduce stigma and promote social inclusion of people living with dementia with support from CIHR. A team of academic researchers, people with dementia, and community partners are working together to develop practical guidelines to provide direction for communities to reduce stigma and promote social inclusion of people living with dementia.
Text box 4: Connecting the national dementia strategy to the dementia research effort
Dementia research in Canada and globally continues to inform activities being undertaken in support of implementing the national dementia strategy. These efforts include sharing research findings with the general population and at-risk populations, including through knowledge translation. A priority is placed on ensuring information is up to date and accurate, including on the Government of Canada dementia website, and presented in language that is accessible for the general population.
PHAC also requires initiatives by partners that we fund to demonstrate the evidence base that informs the design of their project. For example, applicants for funding under the Dementia Strategic Fund: Awareness Raising Initiatives must provide evidence to support why the proposed plan and key activities are expected to enable and result in changed behaviours and attitudes about dementia, and/or encourage or promote dementia-inclusive communities. This includes a summary of the scientific, behavioural and/or social evidence specific to the initiative and a description of how the initiative complements or differs from other approaches, to add to our knowledge.
Federal departments and agencies, including PHAC and CIHR, maintain close collaboration to ensure that policy makers are informed of federally funded research activities. Members of the Ministerial Advisory Board on Dementia who are researchers or who have a strong connection to dementia research also share information with PHAC on research developments.
In addition, CIHR promotes open access to the results of the research it funds for Canadians and decision makers across the country. For example, CIHR funded researchers are required to ensure their publications are freely available within 12 months of publication. This open access makes it possible for research results to have a greater impact – making it easier for decision makers to access the evidence they need.
Working together towards the three national objectives
Dementia-related work in Canada is taking place across a variety of sectors including all levels of government, the health system, non-government organizations, researchers and academics, involving countless individuals. While some initiatives aligned with the national dementia strategy focus specifically on dementia, many other initiatives and programs are accurately described as dementia-related because they address challenges such as encouraging healthy lifestyles that can reduce the risk of developing dementia, investing in an educational infrastructure that supports the next generation of dementia researchers, and providing broad access to quality health and home care. This report focuses mainly on highlighting initiatives that are dementia-specific; however, the Government of Canada also recognizes the fundamental role of the many other activities and investments taking place across the country that are essential in supporting the strategy’s objectives. Several of these broader related efforts are noted in the national dementia strategy.
In developing Canada’s first national dementia strategy and committing to its implementation, the federal government is currently leading efforts focused on investing in research, increasing awareness, enabling partners to deliver community-based initiatives, improving access to and the use of dementia guidance (such as guidelines and best practices) and collecting and sharing surveillance data. Recent federal investments will support greater awareness in the coming years about dementia, including reaching out to more Canadians to share what is known about risk reduction, to highlight the importance of stigma reduction, and to provide information on ways to make our communities more inclusive for people living with dementia. These investments will also improve access to evidence-based guidance related to dementia to ensure information is more widely available. Federal investments in community-based projects will provide for the development and sharing of evidence-based tools and resources that support the wellbeing of people living with dementia and family/friend caregivers living in the community.
Some of the initiatives in Canada that support the national dementia strategy are clearly aligned with only one of the three national objectives; however, many of them support more than one objective and some support all three objectives. This section of the report provides an overview of just a few of the current activities underway in Canada which are contributing to the national dementia strategy’s objectives.
Text box 5: Key federal public health investments
The Public Health Agency of Canada is supporting the implementation of key elements of A Dementia Strategy for Canada: Together We Aspire.
Dementia Community Investment (DCI)
This initiative funds community-based projects that aim to optimize the wellbeing of people living with dementia and family/friend caregivers and/or increase knowledge of dementia and its risk factors by developing, testing, disseminating and scaling up initiatives, knowledge and tools to support these groups. The second invitation for proposals is expected to be launched in fall 2020.
The DCI will also fund a Knowledge Hub to facilitate a community of practice to allow DCI projects to build capacity, learn from each other and collaborate where possible. The Knowledge Hub will also be responsible for developing and sharing lessons learned and best practices from the DCI to help inform dementia policy and program decision-makers across Canada.
Dementia Strategic Fund
This initiative supports a variety of activities focused on awareness and providing reliable and evidence-based information, including access to and use of dementia guidance. Initiatives include a national public education campaign, targeted awareness-raising initiatives delivered by partners, and work to improve dementia guidance. The first projects for targeted awareness raising initiatives being delivered by partners are expected to begin in fall 2020. Efforts to raise awareness of dementia will focus on how to prevent dementia, reduce stigma, and encourage communities to be more dementia-inclusive.
Enhanced Dementia Surveillance Program
Through collaboration with the provinces/territories and other stakeholders, new approaches are being explored and designed to collect data on topics such as undiagnosed dementia, other chronic conditions and diseases experienced at the same time as dementia, and dementia in long-term care settings. These efforts will result in a better understanding of how dementia impacts Canadians, supporting the surveillance and data pillar of the national dementia strategy.
Healthy Living and Chronic Disease Prevention—Multi-sectoral Partnerships (MSP) Program
The MSP Program aims to promote healthy living and prevent chronic disease, by addressing the common risk factors that underlie major chronic diseases, including diabetes, cardiovascular disease and cancer. Several of these risk factors are also risk factors for developing dementia and include: physical inactivity and/or sedentary behaviour; unhealthy eating; tobacco use; and harmful use of alcohol.
Text box 6: Engaging people living with dementia and caregivers
It is important for the lived experience of people living with dementia and caregivers to inform the design and delivery of initiatives related to dementia.
For example, the Dementia Strategic Fund and the Dementia Community Investment, two programs run by the Public Health Agency of Canada, require that applicants demonstrate in their proposals for awareness raising and community-based projects how people living with dementia and/or caregivers will be engaged in the development and implementation of initiatives.
National objective: Prevent dementia
To support the national dementia strategy’s objective of preventing dementia in Canada, areas of focus prioritized under this national objective emphasize the need to advance our understanding about which actions (or interventions) are most effective in reducing risk, broaden awareness among Canadians about actions they can take to reduce their risk, and reduce barriers. Through these actions, the aspiration is that Canada will move towards a complete understanding of the factors that are linked to the risk of developing dementia, and that individuals are aware and are supported in taking measures to reduce their risk through access to built and social environments that enable healthy living.
Initiatives that move us closer to our aspirations include those with the goal of preventing dementia altogether as well as those that may slow the onset of symptoms. They include basic research that furthers our understanding of risk factors, efforts that help those working in the health care sector learn more about dementia prevention, and programs to encourage Canadians to take actions to reduce their risk of developing dementia such as being more physically active and managing other health conditions. Beyond reducing the risk of developing dementia, these actions are known to have additional benefits for the overall health of Canadians.
Initiatives related to dementia prevention highlighted in this year’s report demonstrate the efforts underway across Canada to encourage and enable Canadians to take action that may reduce their risk of developing dementia along with research efforts to better understand why dementia develops and what actions are effective in reducing risk. As well, the 2020 public opinion research funded by the Public Health Agency of Canada is helping set priorities for future awareness-raising efforts through its identification of knowledge gaps. Footnote 5 Examples of efforts on prevention summarized below are funded through a variety of organizations including PHAC’s Multi-sectoral Partnerships Program and CIHR. For further details on each of these initiatives, see Appendix B.
Text box 7: Factors affecting the risk of dementia
There is growing persuasive scientific evidence that healthy living throughout a lifetime may prevent or delay the onset of dementia. Along with having healthy environments to live in, there are individual health behaviours and other factors that can affect the chance of developing dementia. This list outlines several of the factors identified. Research is underway to further explore the links between the risk of developing dementia, individual actions, and environmental surroundings.
From unhealthy to healthy behaviours:
- Physical inactivity (be more active)
- Harmful alcohol use (reduce or quit alcohol use)
- Smoking in later life, over age 65 (reduce or quit smoking)
- Sleep disturbances, such as obstructive sleep apnea (taking steps towards sufficient and better quality sleep)
Management of these health conditions:
- High blood pressure (hypertension)
- Stroke, heart disease and other vascular diseases (affecting blood vessels like arteries and veins)
- Cholesterol levels
- Diabetes
- Obesity
Other factors:
- Social isolation (social engagement and inclusion)
- Lower levels of early life education (more years of childhood education)
Efforts across Canada
Encouraging physical activity
- The Sharing Dance initiative gets Canadians moving through dance (National Ballet School of Canada and Baycrest).
- The Hockey Fans In Training project keeps middle-aged men across Canada at risk of chronic disease active (Western University).
- The Let’s Get Moving Initiative encourages all Canadians to be more active (ParticipACTION).
Reducing the number of Canadians with chronic health conditions
- The Activate: Community Hypertension Prevention Initiative increases awareness of high blood pressure and cardiovascular disease risk and how to manage risk factors (Heart and Stroke Foundation, Ontario and British Columbia).
- The Canadian Diabetes Prevention Program focuses on physical activity and healthy eating to reduce the risk of type 2 diabetes (LMC Healthcare and Diabetes Canada).
- The Healthy Living in St. James Town project focuses primarily on South Asian and African populations who have a higher risk for diabetes and high blood pressure (St. James Town Family Literacy Services, Ontario).
Promoting healthy choices
- The Walk or Run to Quit initiative reduces tobacco use and increases physical activity (Canadian Cancer Society).
- The Activate Your Health project encourages employees in the workplace, particularly women aged 25 to 54, to improve eating habits and physical activity (Capsana, Québec).
- Picking up the PACE (Promoting and Accelerating Change through Empowerment) aims to help care providers address modifiable risk behaviours such as physical inactivity, excessive alcohol use and poor diet as a part of smoking cessation treatment (Centre for Addictions and Mental Health).
- Food Fit: Promoting Healthy Eating and Fitness in Low-Income Communities supports increased knowledge about nutritious foods, improves cooking/food preparation skills and encourages physical activity (Community Food Centres Canada).
Improving our understanding of what contributes to the risk of developing dementia
- The PURE-MIND study is investigating the link between covert (small) strokes and dementia (Heart and Stroke Foundation).
- The New Brunswick Brain Health Initiative: Preventing Alzheimer’s by Lessening Modifiable Risk offers participants support on reducing risk while evaluating risk factors (University of New Brunswick and Horizon Health Network).
- Efforts are being made to better understand how lifestyle and personality factors affect the risk of developing dementia (Sylvia Villeneuve from McGill University and CIUSSS de l’Ouest-de-l’Île-de- Montreal-Douglas Hospital, Montreal).
- Cognitive training programs are being used to learn more about how the brain’s resistance to damage and its ability to change is linked to age-related neurodegenerative diseases (Université de Montréal, Institut Universitaire de Gériatrie de Montréal, Baycrest, University of Toronto).
Improving the knowledge and skills of the health care workforce
- Online resources are available to ensure health care professionals, professors and students working in French have the opportunity to improve knowledge about neurocognitive disorders and to support safe and effective interventions (Le Consortium national de formation en santé – Volet, University of Ottawa).
Text box 8: Reducing the risk of dementia by supporting healthy aging
The environments we live in influence our health and wellbeing. Both the physical and social environments (e.g., buildings, green space, transportation systems, recreation and educational activities) can be designed to make it easier to adopt healthy living behaviours, which may reduce the risk of developing dementia.
Age-Friendly Communities are an example of intentional efforts to provide a healthier environment to live in. Within Age-Friendly Communities, the physical and social environments of a community are designed to improve the health and wellbeing of older adults to help individuals age actively, live safely, and stay involved. As of January 2020, more than 1,400 communities in ten provinces across Canada have taken steps to become more age-friendly.
The City of Ottawa, for example, continues to take action to becoming more age-friendly through its third Older Adult Plan 2020–2022. Among its 24 concrete actions, the plan aims to promote healthy aging behaviors, create supportive environments and influence healthy public policies to prevent and mitigate chronic disease, promote mental health and prevent injuries. The City works closely with Ottawa Public Health on its Aging Well Plan that envisions a city where all older adults and their caregivers are healthy, safe, valued and actively engaged in their wellbeing within a compassionate and inclusive environment.
Data points on preventing dementia
In this year’s report, the data points related to dementia prevention are focused on awareness of factors that influence the risk of developing dementia and on how many Canadians are affected by these factors. The report also includes data on the number of new cases of dementia, an annual statistic that over the longer term will help track progress on reducing the risk of developing dementia in Canada.
Awareness among Canadians about key factors linked to the risk of developing dementia
Evidence about factors that appear to be linked to the risk of developing dementia is growing. To make progress on preventing dementia, one key step is to expand awareness about these factors and the best ways to take action to reduce risk. The data below, gathered through a national public opinion survey in 2020, provides baseline information on how aware Canadians are of the factors associated with the risk of developing dementia. Footnote 5 Over time, the goal of awareness efforts is to increase the level of understanding among Canadians about how they can reduce their risk of developing dementia.
This survey data shows that most Canadians can name at least one risk factor but also that less than half of Canadians are aware of several risk factors linked to dementia including smoking, air pollution, high blood pressure (hypertension), diabetes, and high cholesterol.
| Overall awareness | Percentage (%) Canadians that are aware |
|---|---|
| Awareness of at least one factor affecting the risk of developing dementia | 89 |
| Awareness broken down by risk factor | |
| Loneliness/social isolation | 64 |
| Harmful alcohol use | 58 |
| Having had a stroke | 54 |
| Lack of physical activity | 54 |
| Diet lacking in nutrition | 53 |
| Sleep disruption (e.g., sleep apnea) | 50 |
| Hypertension/high blood pressure | 35 |
| Smoking | 32 |
| Diabetes | 27 |
| Air pollution | 21 |
| High cholesterol | 20 |
| Hearing loss | 16 |
| Fewer years of formal education | 13 |
Canadians and key factors linked to the risk of developing dementia
A reduction in the percentage of Canadians with key modifiable risk factors and an increase in Canadians with key protective factors can be expected to support a reduction in the rate of new cases of dementia as well as reduce the number of Canadians with other chronic health conditions. The information below provides information about some of the key risk factors related to dementia for which data is regularly collected. The goal of awareness efforts and programs that encourage and support healthier living is for these numbers to move in directions that support risk reduction.
| Dementia risk factor | Percentage (%) of Canadians with factor | Year | Source Footnote 6 |
|---|---|---|---|
| Behavioural risk and protective factors | |||
| % of population (aged 15+) that reports exceeding low risk alcohol drinking guidelines for chronic health effects | 16.1 | 2017 | Canadian Tobacco, Alcohol and Drugs Survey |
| % of population (aged 15+) that reports being current smokers (daily or occasional) | 15.1 | 2017 | Canadian Tobacco, Alcohol and Drugs Survey |
| % of adults (aged 18-79) who meet physical activity guidelines by accumulating at least 150 minutes of moderate-to-vigorous physical activity each week, in bouts of 10 minutes or more | 16.4 | 2016– 2017 | Canadian Health Measures Survey |
| % of population (aged 18-79) that reports obtaining the recommended amount of daily sleep | 64.5 | 2014– 2015 | Canadian Health Measures Survey |
| Chronic health conditions and risks | |||
| % of population (aged 20+) with diagnosed hypertension (high blood pressure) | 25.5 | 2016– 2017 | Canadian Chronic Disease Surveillance System |
| % of population (aged 20+) with diagnosed stroke | 2.9 | 2016– 2017 | Canadian Chronic Disease Surveillance System |
| % of population (aged 18-79) with elevated blood cholesterol | 15.1 | 2016– 2017 | Canadian Health Measures Survey |
| % of population (aged 20+) with diagnosed diabetes | 10.9 | 2016– 2017 | Canadian Chronic Disease Surveillance System |
| % of adults (aged 18-79) that are obese | 26.9 | 2016– 2017 | Canadian Health Measures Survey |
| Other factors | |||
| % of population (aged 20+) that reports having less than a high school education | 11.1 | 2017 | Canadian Community Health Survey |
| % of population (aged 12+) that reports a “very strong” or “somewhat strong” sense of belonging to their local community(social isolation) | 69.3 | 2017 | Canadian Community Health Survey |
Newly diagnosed cases of dementia
Progress on prevention should contribute to a reduction in new cases of dementia in Canada. This data point tells us the crude rate of newly diagnosed dementia cases (incidence), including Alzheimer’s disease, for those aged 65 years and over in 2016-2017. The number is higher for women than men. This data point also indicates that women are more likely to develop dementia than men.
In 2016–2017 there were 1,351 new cases per 100,000 Canadians aged 65+ years
- 1,489 per 100,000 Canadian women aged 65+ years
- 1,193 per 100,000 Canadian men aged 65+ years Footnote 6
National objective: Advance therapies and find a cure
The aspirations for the national objective of advancing therapies and finding a cure highlight the need to improve how therapies are developed and to broaden their availability, as well as to increase Canada’s dementia research effort. The national dementia strategy notes the importance of having research priorities informed by broad stakeholder input, including from people living with dementia and caregivers, as well as including them as active participants and partners in the research itself. It calls on researchers to include elements in their work that contribute to ensuring that findings can be quickly understood and put into practice, so that the benefits of these advances are realized sooner.
Activities in support of this national objective include efforts to develop and improve therapies that help to manage the symptoms of dementia and slow its progression. Research that supports this national objective ranges from exploration of the mechanisms that cause dementia, to development and testing of innovative therapies that address different aspects of dementia. Treatment of dementia in Canada also benefits from access to and use of expert guidance, such as evidenced-based guidelines and best practices that are periodically reviewed and updated.
In this year’s report, we note research on the links between other conditions, such as high blood pressure and frailty, and dementia, the work to identify biomarkers (indicators for dementia detection) and the mechanisms underlying dementia. A sampling of the diversity of approaches to therapies is also included, such as music therapy, lighting systems, focused ultrasound, sensor-based software and facial recognition technology.
As well, for the first time since 2012, dementia experts gathered in 2019 to review and renew guidance on dementia. Efforts continue to increase and improve the inclusion of people living with dementia and caregivers in the various stages of research. Many of the efforts highlighted in this report receive funding from the Canadian Institutes of Health Research, AGE-WELL and/or the Weston Brain Institute. For further details on each of these initiatives, see Appendix B.
Efforts across Canada
Understanding dementia better
- An examination of the impact of high blood pressure on brain health using live imaging techniques has resulted in a recommendation to combine treatments targeting both hypertension and amyloid for better results (University of Toronto).
- COMPASS-ND is a large-scale clinical study designed to learn about who is at risk of developing dementia, determine how early dementia can be detected, and find out what tests are most effective at detecting dementia. COMPASS-ND data was used to support research, published in 2019, that concluded that guidelines for screening for frailty need to be improved for people living with dementia.
- A research project investigating the role of genetic signals in the brain using brain imaging in people diagnosed with pre-dementia due to Alzheimer’s disease is focused on revealing new treatments for dementia (Douglas Mental Health University Institute).
- Weihong Song, a Canada Research Chair in Alzheimer’s Disease, is working on new disease- modifying treatments and identifying molecular mechanisms that lead to dementia, biomarkers (indicators) and drug targets (University of British Columbia).
Innovative therapies
- A French Music Therapy Program offers free loans of headphones, speakers and digital music players containing personalized playlists to help French-speaking Yukoners retain language abilities and promote memory (Yukon Francophone Health Network and Department of Health and Social Services).
- Adaptive Lighting for Alzheimer and Dementia INtervention (ALADIN) is a smart light system used to promote better sleep and subsequently improve cognitive and emotional wellbeing of people living with dementia (University of Toronto).
- Sensor-based software platforms have been developed to track and improve the physical and cognitive health of people living with dementia at home and provide engaging cognitive and physical training (University of Alberta).
- A low-cost and portable focused ultrasound technology has been developed to improve the diagnosis and treatment of neurodegenerative diseases, using sound waves for therapy (Sunnybrook Research Institute and University of Toronto).
- Affordable solutions are being developed to improve pain management for people with dementia who reside in long-term care facilities including an automated system that uses facial recognition technology and artificial intelligence (University of Regina and Toronto Rehab Institute).
Inclusive dementia research
- The Canadian Consortium on Neurodegeneration and Aging’s program, Engagement of People with Lived Experience of Dementia, enables individuals to be meaningfully and actively involved in the research process, including program direction, priority setting, conducting research and moving results into action.
- Researchers are working with people living with dementia through participatory action research to learn how communities can “turn stigma on its ear” and promote active social participation of people living with dementia (University of British Columbia, Simon Fraser University and Lakehead University).
Text box 9: Canadian consensus conferences on the diagnosis and treatment of dementia
Since 1989, clinicians treating people with cognitive decline associated with aging have been meeting periodically to review the information available in the medical literature and publish recommendations for better management of people at risk of cognitive decline, with mild symptoms, or who have dementia. These conferences bring together all health disciplines involved in the diagnosis and treatment of dementia, in partnership with the Alzheimer Society of Canada. Over the years (1998, 2006, 2012, 2019), updates and new themes have been added, such as early detection of cognitive decline, reduction of the risk of progression, and psychosocial and non-pharmacological interventions.
Themes for the 5th Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD5) in 2019, were as follows: (1) biological diagnostic criteria for Alzheimer’s disease; (2) diagnostic criteria for vascular cognitive impairment; (3) detection of dementia; (4) imaging and other biomarkers; (5) non-cognitive markers of dementia; (6) risk reduction; (7) psychosocial and non-pharmacological interventions; and (8) deprescription of dementia medications.
Data points on advancing therapies and finding a cure
Data points for this national objective provide information on the federal research investment in dementia research available from the Canadian Institutes of Health Research, the primary federal health research funding agency in Canada. PHAC will continue to gather additional data in this area for future reports to ensure that we have a complete picture of Canada’s broader dementia research effort.
CIHR funding for dementia research in Canada
Dementia research spending by CIHR in 2018-19: approximately $40.8 million Footnote 7 .
Training the next generation of dementia researchers
Building on Canada’s internationally recognized contribution to dementia research, efforts are needed to support the next generation of researchers. This data point reports on the number of students/trainees engaged in dementia research as a result of CIHR funding. This includes students and fellows who either received a training award (direct trainees), or received a stipend paid through researcher grants (indirect trainees).
Number of direct and indirect trainees supported through new and ongoing CIHR-funded dementia research projects in 2018–19: 359 Footnote 8 .
Text box 10: Estimating the future burden of dementia
The Public Health Agency of Canada and Statistics Canada are developing a Population Health Microsimulation model for dementia (POHEM-Dementia). This complex tool uses existing national statistics on dementia and its associated risk factors to estimate how many cases of dementia may develop in the future under normal circumstances (status quo). It can also estimate how many cases could be prevented with the implementation of policies and programs that affect important risk factors for dementia, compared to the status quo. POHEM has the potential to help researchers and policy makers assess the health and economic impacts of promising prevention strategies, before their implementation.
National objective: Improve the quality of life of people living with dementia and caregivers
There are many aspects to improving quality of life for people living with dementia and caregivers. Aspirations for this objective include: eliminating stigma; timely and compassionate diagnosis that comes with access to supports; care that is tailored to the needs of each individual; care providers that are well-trained and have access to the resources they need to provide quality care; and resources for caregivers to help protect their own wellbeing and to provide them with supports that will assist their efforts to care for those living with dementia.
Initiatives that support this broad objective touch on areas such as: access to diagnostic tools and quality health care provided by a skilled and knowledgeable workforce, community-based services and supports, actions to reduce stigma, and work to share and scale up efforts to make communities more dementia- inclusive. These are activities that make a significant difference every day in the lives of people living with dementia and caregivers. Whether it is improving the experiences in the health care system of people living with dementia, supporting life at home or making it easier to stay engaged, active and express preferences, these initiatives support living in a way that creates quality of life.
The 2020 public opinion survey found that about one-fifth of respondents did not know enough to share their views when it comes to access to health care and the quality of health care in their communities, perhaps due to a lack of experience. The majority of respondents (70%) rated access to care for people living with dementia as moderate to excellent in their communities, with 66% rating the quality of that care from moderate to excellent. Footnote 5 There are countless other efforts being made across Canada to improve the quality of life of people living with dementia and caregivers by a wide cross section of organizations. While many of these initiatives are funded and/or delivered by provincial and territorial governments, others are based at academic institutions, or provided by community organizations and health care institutions. For further details on each of these initiatives, see Appendix B.
Efforts across Canada
Staying active and engaged and supporting inclusion
- The Dementia-Inclusive Choices for Exercise initiative aims to increase accessible exercise opportunities by developing dementia-specific evidence based tools and training for exercise providers (pilots in Kitchener-Waterloo, Halifax and northern British Columbia).
- Voices in Motion and NoteWorthy Singers are intergenerational choirs for people living with dementia, caregivers, friends and students in Victoria and Vancouver, helping to create a more dementia-inclusive community.
- Research is using the lenses of shared decision-making, feminist care ethics and social citizenship to look at how people living with dementia could become more active collaborators in shaping end-of-life decision-making (University of British Columbia).
- The Volunteer Companion Program in Prince Edward Island is a one-on-one home visiting program for people living with dementia and their caregivers who are at risk of social isolation.
- Cracked: new light on dementia is a research-informed theatre production and film seen across and outside Canada that is focused on the challenges of stigma; work is underway to develop an interactive web-based learning platform.
- The Supporting Inclusion through Intergenerational Partnerships Collective Impact initiative promotes the social inclusion of seniors with mild to moderate dementia and caregivers by creating opportunities to engage with youth (Waterloo, Ontario).
- The Alzheimer Society of Canada’s nationwide anti-stigma campaign, “Yes. I live with dementia. Let me help you understand”. highlights the diverse lived experience of Canadians living with Alzheimer’s disease and other forms of dementia to address misconceptions and reduce stigma.
Text box 11: Dementia-inclusive communities
In a dementia-inclusive community, people living with dementia feel respected, safe and supported to live well, interact comfortably with community members and participate in community activities. Community members are aware of and understand dementia, and the care and support provided within the community is culturally safe and culturally appropriate, and mindful of diversity. Dementia-inclusive communities help to reduce and eliminate barriers, including those resulting from stigma.
The Alzheimer Society of Canada, supported by PHAC’s Dementia Community Investment, is engaging people living with dementia, caregivers and key sector groups to build on the work of the Alzheimer Societies in British Columbia, Manitoba, Ontario and Saskatchewan towards a Dementia-Friendly Canada (DFC). The Dementia Friendly Canada (DFC) project will develop and refine a national DFC vision through the development of training tools, the expansion to new geographic communities, and the development of an evaluation structure and indicators of success. A national DFC toolkit will also be developed to help guide the creation of dementia-friendly communities across Canada. This includes the development and testing of guides and tools to educate and train professionals in housing, legal, finance, recreation, libraries, transportation, retail, restaurants and emergency response sectors. As well, a general dementia-friendly public module will be developed, which will build on tips and strategies for the service industry and the public.
Other organizations have also created resources to help communities become more dementia-friendly. For example, the Brenda Strafford Foundation published A Guide for Creating Dementia Friendly Communities in Alberta which outlines the steps and lessons learned from its Dementia Friendly Communities pilot project.
Increasing access to dementia care
- Dementia Assessment Units assess the needs of individuals with home care support and those living in publicly funded Special Care Homes to stabilize individuals and develop a personalized care plan (Saskatchewan Health Authority).
- Manitoba’s My Health Teams plan and deliver coordinated, comprehensive primary care focused on geographic areas or specific communities to ensure that people living with dementia and their families have access to care built around their health needs.
- The summer school at Glendon College in Ontario brings together health stakeholders working in Francophone university and community sectors to improve day-to-day practices and share best practices in cognitive health and dementia.
- The Home Dementia Care Program in Newfoundland and Labrador helps people with moderate to advanced dementia live well at home by increasing access to medical care.
- Across Ontario, Multispecialty Interprofessional Team (MINT) Memory Clinics provide dementia care in primary care settings within communities. In addition to primary care memory clinics, the central-eastern region has developed the Geriatric Assessment and Intervention Network (GAIN), a coordinated network of interprofessional teams who support high-risk seniors and their families with comprehensive, specialized assessments and targeted interventions in their own homes.
Person-centred care
- Upon admission to a long-term care home in Yukon, the Continuing Care Therapy Services program offers individualized assessments by an occupational therapist, physiotherapist, recreation therapist and/or speech-language pathologist.
- In the Northwest Territories, the Supportive Pathways model of care uses a person-centered approach that fosters respectful, compassionate dementia care and trains care providers in delivering care that is responsive to individuals in a home-like supportive environment.
- Co-designing Dementia Care in New Brunswick: Building the Future Together aims to improve the knowledge of primary care providers around diagnosis and delivery of dementia care, as well as awareness of services among seniors at-risk for dementia and care partners (UNB Saint John and Horizon Health Network).
Behavioural symptoms
- Behavioural Supports Ontario provides comprehensive behavioural assessments and person- centred support plans focused on responsive behaviours/personal expressions (e.g., repetitive questions, apathy, pacing, screaming, grabbing) associated with dementia and other neurological conditions.
- In Montreal, a specialized interprofessional team has been set up to assist in complex situations involving people living with Alzheimer’s disease and other neurocognitive conditions to reduce problematic behaviours and find strategies to improve the quality of life of those living with these conditions and of caregivers (Centre intégré universitaire de santé et de services sociaux du Centre-Sud-de-l’Île-de-Montréal).
- The Behavioural and Psychological Symptoms of Dementia (BPSD) Algorithm is available to all care providers in British Columbia—it is an electronic interactive tool that supports interdisciplinary, evidence-based and person-centred clinical assessment and care decisions with a specific focus on non-pharmacological interventions and the appropriate use of antipsychotic drugs in long-term care settings.
- The Appropriate Use of Antipsychotics approach, used in more than 300 long-term care homes across Canada, engages people living with dementia, families and staff to understand underlying causes of behaviours and consider safely reducing or discontinuing medication (Canadian Foundation for Healthcare Improvement).
Skills, training and tools for care providers
- Alberta’s Health Care Aide (HCA) curriculum, updated in 2019, describes required skills, knowledge, behaviours and attitudes to help HCAs better understand and support the needs of people living with dementia (Alberta Health).
- The Dementia Care Pilot Project is evaluating an online dementia education program and screening tools for primary care providers to use in family practice (Nova Scotia).
Support for caregivers
Caregivers for people living with dementia face unique challenges and may jeopardize their own health while trying to provide the best support they can to their loved ones. Improving support for caregivers is an area of focus of the national dementia strategy. The 2020 public opinion research survey found that almost two out of five Canadians (36%) had provided assistance to someone living with dementia within the last five years. Of those caregivers, only 57% agreed that they were able to provide the care needed, suggesting that more can be done to support caregivers. Footnote 5 This year’s report shares some examples of initiatives underway across Canada that support dementia caregivers.
Building knowledge
- Introducing Gentle Persuasive Approaches in Dementia Care is an initiative that aims to strengthen the knowledge of formal (paid) and informal (unpaid and often family/friend) caregivers (Alzheimer Society of New Brunswick and Horizon Health).
- The Community Dementia Ambassador Training pilot program provides resources and in-person supports to partners and caregivers of people living with dementia in remote communities in the Northwest Territories (Alzheimer Society of Alberta and the Northwest Territories).
- In Yukon, the Shine a Light on Dementia: Caregiver Training Program aims to equip caregivers with knowledge and skills, while sharing experiences and resources (Yukon Department of Health and Social Services).
- My Tools 4 Care-In Care is a web-based platform that provides interactive activities, resources and guidelines to support caregivers to improve mental wellbeing by fostering social inclusion and to building skills and knowledge in working with long-term care providers (University of Alberta).
Financial support
- The Government of Nova Scotia Caregiver Benefit Program provides funding to eligible caregivers who are providing assistance to qualified care recipients, including those with moderate cognitive and high physical impairment residing in the community (Nova Scotia Health Authority).
- Federal personal income tax assistance is provided in recognition of the fact that people living with dementia and those who care for them may have a reduced ability to pay tax.
Community-based services
- The Community-based Innovations for Dementia Care initiative provides funding to 14 local community and health service providers to implement projects that build innovative approaches in person-centred dementia services (Alberta).
- The Home and Community Care Program provides home and community care services in all communities, such as home support and respite care for caregivers as well as for Nunavummiut diagnosed with dementia-related illness who are able to be supported at home. A new 24-bed long-term care facility will provide around-the-clock nursing care to support the medical and cultural needs of a growing population of Nunavut seniors (Nunavut).
Data points on improving the quality of life of people living with dementia and caregivers
The data points for this national objective focus on the stigma that is sometimes associated with a diagnosis of dementia as well as aspects that address the quality of life of people living with dementia, and the wellbeing of caregivers.
Stigma: Comfort with sharing a diagnosis of dementia
Reducing and ultimately eliminating the stigma (negative stereotypes and resulting behaviours) associated with dementia is essential to improving the quality of life of those living with dementia and dementia caregivers. One effect of stigma can be a reluctance to seek information about dementia, have discussions with care providers that could lead to a diagnosis, and to share information about a diagnosis with family members, friends, employers and neighbours. However, receiving a timely and compassionate diagnosis along with access to resources and supports can improve quality of life and enable advance care planning.
The data point below focuses on the percentage of Canadians who report that they would feel uncomfortable disclosing symptoms and/or a diagnosis of dementia to others. While most respondents are comfortable talking to health care providers about a diagnosis of dementia, they become less comfortable when talking to friends, and particularly employers, neighbours and others on the community. This information was gathered through the baseline public opinion research survey conducted in early 2020 for the Public Health Agency of Canada. Footnote 5
| Situation | Percentage (%) Footnote 5 |
|---|---|
| Having a discussion with a health care provider about your personal risk of developing dementia | 8 |
| Asking a health care provider for information about symptoms which could lead to obtaining an assessment and diagnosis | 7 |
| Telling close family members about a dementia diagnosis | 14 |
| Telling friends about a dementia diagnosis | 20 |
| Telling an employer about a dementia diagnosis | 35 |
| Telling neighbours or others in the community about a dementia diagnosis | 36 |
Quality of life: depression, pain and social interaction
Quality of life for those living with dementia depends on many things and what determines that quality varies between individuals. This data point which covers some parts of Canada focuses on three aspects of quality of life for people living with dementia who are receiving home care: depression, daily pain, and social engagement. Footnote 9 It suggests that many have some social interaction, but one-quarter of them may have a potential or actual problem with depression and one third are experiencing daily pain in some form.
| Data point | Percentage (%) of Canadians in 2018–19 |
|---|---|
| People living with dementia receiving homecare with withdrawal from activities of interest and/or reduced social interaction | 18.3 |
| People living with dementia receiving homecare with a potential or actual problem with depression, based on a depression rating scale | 24 |
| People living with dementia receiving homecare with daily pain (severe and not severe) | 34.6 |
Caregivers experiencing distress
Caregivers often take on much of the responsibility of providing care for people living with dementia, particularly those living at home. This data point, which covers some parts of Canada, provides some insight into how caregivers of people living with dementia who receive home care are managing the challenges of supporting the quality of life of loved ones in comparison to caregivers of those without dementia receiving home care. Footnote 9 It suggests that caregivers of those with dementia are twice as likely to experience distress and/or find themselves unable to continue, compared to caregivers for those without dementia.
Percentage of people living with dementia receiving home care with caregivers who experience distress, compared to caregivers of those without dementia: 37.6% vs 18.6% in 2018-19.
This percentage includes those who experience distress, anger and/or depression as well as those who have been unable to continue as caregivers. Footnote 9
Cross-cutting efforts
Sharing information resources
Much of the activity in Canada expected to contribute to progress on the national dementia strategy aligns with all three objectives. Examples include efforts to make valuable information more widely available through awareness campaigns for the general public and resources tailored to the needs of people living with dementia and care providers. The initiatives below highlight some of the work taking place to provide this information. More details are provided in Appendix B.
- The P.I.E.C.E.S.™ Learning and Development Program delivers learning resources to those caring for older adults with complex physical and cognitive and mental health needs as well as behaviour changes in British Columbia, Nova Scotia, and the Yukon.
- U-First! Education offered by the Alzheimer Society of Nova Scotia, uses the P.I.E.C.E.S™ model to improve the quality of the interaction between care providers and people living with dementia.
- Provincial Alzheimer Societies in British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador are providing the First Link Program which offers services and support to people living with dementia and their families.
- The Dementia Association for Awareness and Support, developed in Edmonton, Alberta, provides people living with dementia and caregivers with access to educational resources and support tools.
Focusing on those at higher risk and facing barriers to equitable care
The national dementia strategy highlights the importance of considering populations and individuals who are at higher risk of developing dementia and/or who experience barriers to care including diagnosis and access to supports and services when designing and delivering dementia initiatives. These populations and individuals include Indigenous peoples, individuals with intellectual disabilities, individuals with existing health issues, older adults, women, ethnic and cultural minority communities, LGBTQ2 individuals, official language minority communities, rural and remote communities, and those with young onset dementia. Other populations may be identified as we learn more about dementia’s impact in Canada.
This year’s annual report provides examples of initiatives focusing on those individuals and populations, such as efforts to: provide quality dementia care and encourage dementia- inclusive communities in rural and remote communities; raise awareness within ethnic and cultural minorities; understand the experiences of official language minority individuals in the health care system; and improve access to French-language educational opportunities to support the ability to provide quality health care in both official languages across the country.
As well, applicants to PHAC’s funding programs Dementia Strategic Fund and Dementia Community Investment must demonstrate how equity, including consideration of culture, sex and other identity factors (such as LGBTQ2+ [lesbian, gay, bisexual, transgender, queen, two-spirit individuals], age, education, geography, and income) have been considered in the design, implementation and evaluation of the proposed project. Examples of projects underway to support these groups include the following (note further details can be found in Appendix B):
- The Rural Dementia Action Research (RaDAR) Team in Saskatchewan aims to improve access to appropriate care from early to late stage dementia, and from community to facility-based care. The Rural and Remote Memory Clinic (RRMC), developed alongside the RaDAR Team, increases the availability and accessibility of dementia care in rural and remote areas and focuses on the diagnosis and management of atypical and complex cases of suspected dementia.
- The Primary Health Care Integrated Geriatric Services Initiative supports increasing capacity across primary health care teams in predominantly rural communities in Alberta to provide support for people living in the community who are impacted by dementia.
- The University of Regina is leading the Interventions to Enhance Social Inclusion of Older Adults with Dementia in Saskatchewan Collective Impact project (2019–2024), to increase the social inclusion of people living with dementia and caregivers in small cities and rural or remote communities in Saskatchewan.
- The Alzheimer Society of Nova Scotia is working with the Health Association of African Canadians to facilitate dementia education in Black communities across Nova Scotia and adapt an education session to explore the needs of people of African ancestry living with dementia in Nova Scotia.
- Exploratory research in Ottawa by Corine Carbonneau and Marie Drolet highlights the role of navigators in securing access to quality care for people living with dementia in official language minority communities.
- Glendon College, the bilingual campus of York University, offers an online certificate in dementia and cognitive health to Francophone professionals across Canada. It has also developed a Cognitive Neuropsychology Stream available for its undergraduate students.
- Research at the University of Moncton aims to provide Francophone health professionals with a validated and culturally adapted tool that will support early diagnosis and reduce linguistic barriers to care.
Conclusion
The 2020 report to Parliament on A Dementia Strategy for Canada: Together We Aspire marks the first anniversary of the release of the strategy. This report, through the variety of initiatives selected this year as examples of our collective effort, underlines that progress on the strategy and its impact over time relies on the initiatives and investments of all levels of government and from many different organizations across Canada.
As Canada continues to implement the strategy and pursues its aspirations, the Public Health Agency of Canada (PHAC) will continue to gather information to increase our understanding of the initiatives and investments across Canada that are aligned with the strategy’s three national objectives: prevent dementia; advance therapies and find a cure; and improve the quality of life of people living with dementia and caregivers. This information gathering will help us to assess our national effort on dementia and determine where there are gaps and where further effort is required.
It is also clear that the impact of COVID-19 on Canadians, including people living with dementia and caregivers, will shape and inform federal and other efforts related to dementia as we move forward. The Government of Canada will continue to gather information on that impact and use it to inform how federal initiatives can best support Canadians in managing the risks of COVID-19 and recover from its impact, including those living with dementia.
The 2020 national public opinion research survey is part of the Government of Canada’s initial work on implementation and is helping us better understand the knowledge and perceptions of Canadians on key aspects of dementia, including risk reduction and stigma. It creates a baseline that will also help us measure progress on improving awareness and knowledge in Canada on dementia in the years ahead. It also provides many insights to help guide future priorities for initiatives and investments. The final results of this survey will be available later this year.
The 2020 survey revealed some key areas where awareness-raising efforts in the years ahead can be particularly important. For example, knowledge gaps are higher in some regions of the country and within some populations that are at higher risk. As well, about one-quarter of respondents were unaware that there are actions that can be taken to reduce the risk of dementia. There are also knowledge gaps regarding some risk factors linked to dementia, including existing health conditions such as high blood pressure (hypertension), heart disease and diabetes, and how certain behaviours or environmental factors such as smoking and air pollution can increase risk. Only one quarter of survey respondents reported taking steps specifically intended to reduce their risk for developing dementia.
The survey also confirms more work needs to be done to reduce and ultimately eliminate stigma and improve quality of life for people living with dementia. Survey findings suggest that more than two-thirds (68%) of Canadians believe that people have negative assumptions about the abilities of people living with dementia and face a lower quality of life than people without dementia (70%). Less than half (47%) of the survey respondents believe that people living with dementia may be able to continue working for years after the onset of symptoms.
There is good news in that only 12% of respondents reported that they would not be comfortable interacting with someone living with dementia, largely due to uncertainty or lack of knowledge about dementia which suggests there is potential to increase this comfort level among this small group. However, only 46% of respondents feel efforts to make the community safer for people living with dementia are moderate to excellent and only 51% rated opportunities for social engagement/social connection for this population at moderate to excellent. One-quarter of respondents felt that the level of support in their community for people living with dementia is poor while 25% did not know, suggesting that while there is room for awareness raising and improvement of support, there is also much happening that is making a difference and is recognized.
All organizations across Canada involved in dementia-related initiatives are encouraged to share information with PHAC about their work. This effort to create a more comprehensive understanding of our national effort will provide a more accurate portrait of the magnitude and scope of work underway in Canada, while identifying gaps in programs and services. This evergreen inventory will also be used to select initiatives for future reports to Parliament. If you would like to receive communications about the national dementia strategy and funding opportunities or provide information about your activities, please contact the PHAC Dementia Policy Secretariat. We thank all the organizations that contributed information to this year’s report.
Appendix A: Aspirations for Canada’s efforts on dementia

Figure 2 - Text Equivalent
This image is a visual depiction of the current statuses and aspirations of Canada’s efforts on dementia.
The title of the table appears at the top “Aspirations for Canada’s efforts on dementia”.
Below the title is a table with a column for each of the current statuses and their corresponding aspirations outlined for each national objective.
In the first row/section is the objective of “Prevent dementia”. The corresponding current statuses are:
- Incomplete understanding of risk and protective factors linked with dementia, with some factors not yet identified and insufficient evidence on the link between factors and dementia.
- Limited evidence about effective interventions to reduce risk for dementia and insufficient information resources.
- A lack of awareness among the general public and care providers about actions that may help prevent dementia.
- Barriers related to built and social environments limit the ability of individuals to pursue healthy living in ways that may reduce the risk of developing dementia.
In the next column, the aspirations for the objective “Prevent dementia” are:
- A complete understanding of the risk and protective factors linked to dementia, their impacts and interactions.
- Availability of effective prevention resources and interventions, supported by a strong evidence base.
- All people living in Canada are aware of actions that prevent dementia.
- All people living in Canada have access to built and social environments that support their ability to pursue healthy living in ways that may reduce their risk of developing dementia.
In the second row/section is the objective of “Advance therapies and find a cure”. The corresponding current statuses are:
- Limited broad stakeholder input when setting research priorities and insufficient engagement of people living with dementia and caregivers.
- Annual investment in dementia research in Canada is less than one percent of dementia care costs.
- Options for evidence-informed therapies remain limited and often are not person-centred.
- People living with dementia and caregivers are predominantly the subject of research to develop new therapies and find a cure.
- Research findings tend to stay within academic settings and journals and are not broadly known, accepted, or brought into clinical practice.
In the next column, the aspirations for the objective “Advance therapies and find a cure” are:
- Research priorities established in an inclusive manner with broad stakeholder input, with the participation of those living with dementia and caregivers.
- Annual investment in dementia research in Canada exceeds one percent of dementia care costs.
- New evidence-informed person-centred therapies are more readily available.
- People living with dementia and caregivers are active participants and partners in research to develop new therapies and find a cure.
- Research design always includes efforts that ensure findings can be understood, adopted and quickly put into practice.
In the third row/section is the objective of “Improve the quality of life of people living with dementia and caregivers”. The corresponding current statuses are:
- Widespread stigma within communities and a lack of understanding of dementia.
- Individuals are unable to receive an early or timely diagnosis, or feel unsupported when receiving a diagnosis.
- Lack of access to, awareness or understanding of health and social services that provide integrated and person-centred care.
- Lack of information and resources for care providers, reducing the capacity to provide quality care.
- Caregivers experiencing burnout, financial hardship, isolation and depression while caring for someone living with dementia.
In the next column, the aspirations for the objective “Improve the quality of life of people living with dementia and caregivers” are:
- All people living in Canada understand dementia and stigma no longer exists in Canada.
- A timely diagnosis, provided in a compassionate manner, is available to all people living in Canada, along with immediate availability of resources and supports.
- Integrated, person-centered quality care based on evidence-informed best practices across all settings and that people feel welcomed and well-cared for when hospitalization or admission to long-term care is necessary.
- Care providers have access to the resources and training needed to deliver quality care.
- All caregivers have access to the resources and supports required to protect their own wellbeing and to care for someone living with dementia, including being equipped to navigate health care and other support systems.
Appendix B: Efforts across Canada
Further information on the initiatives highlighted in this year’s report is provided below. These initiatives were chosen to showcase a variety of efforts underway across Canada by different types of organizations; some are national or regional in scope, while others are focused on certain communities. All of them contribute to reaching our shared goals on dementia and can inspire further action.
National objective: Prevent dementia
Encouraging physical activity
The National Ballet School of Canada’s (NBS) Sharing Dance initiative engages all ages, including children and older adults, in quality-of-life enhancing dance activities. Engaging more than 50,000 Canadians annually, programs build physical literacy among children, focus on injury prevention and improving quality of life for seniors, and celebrate the joy of movement through hundreds of community-led Sharing Dance Day events. Jointly developed with Baycrest, the Baycrest NBS Sharing Dance Seniors suite of programs includes in-person and video-streamed classes and training opportunities. NBS and Baycrest also plan to train more knowledge users across Canada, focusing on how and why dance can play a valuable role in the lives of people living with dementia and their communities.
Western University’s Hockey Fans in Training project aims to increase physical activity and healthy living behaviours among middle-aged (35-65 years old) overweight and obese men at risk of chronic disease through their common love of Canadian hockey. This national project has enrolled men from diverse backgrounds (including Indigenous men and newcomers to Canada) across the country in rural, suburban and urban centres. It is expected to reach 1,280 participants.
ParticipACTION’s Let’s Get Moving is a 5-year initiative that uses public education campaigns to encourage all Canadians to sit less and move more where they live, learn, work and play. The initiative includes a focus on those who face challenges and disadvantages that make it harder to adopt healthy behaviours, such as Indigenous peoples, people with disabilities, LGBTQ2+ individuals, and racialized minorities. The free ParticipACTION app and the Community Better Challenge are designed to raise public engagement in physical activity. To date, the app has supported over 100,000 users while the Challenge in search of Canada’s most active community has rallied over 1,000 communities and 11% of Canadians.
Reducing the number of Canadians with chronic health conditions
The Heart and Stroke Foundation’s Activate: Community Hypertension Prevention Initiative is a community-based program designed to increase awareness of high blood pressure and cardiovascular disease risk among participants 40 years and over. It aims to improve participants’ ability to effectively manage their modifiable risk factors for cardiovascular disease, stroke, and vascular cognitive impairment through online tools and referrals to community resources, helping to avoid high blood pressure. The initiative uses a Social Impact Bond model, an innovative financing tool that makes government funding conditional on achieving outcomes. The project is being delivered in Ontario and British Columbia. It is expected to reach close to 5,000 participants.
LMC Healthcare’s Canadian Diabetes Prevention Program is delivering and evaluating an intensive lifestyle intervention program focusing on physical activity and healthy eating to reduce the risk of type 2 diabetes in Canada. LMC Healthcare is working with Diabetes Canada to target individuals at risk of developing diabetes and those diagnosed with prediabetes through this national project which is expected to reach 3,850 participants.
St. James Town Family Literacy Services’ Healthy Living in St. James Town project takes place in a culturally diverse neighbourhood that is comprised of many newcomers to Canada. It focuses primarily on the South Asian and African populations, who are two times more likely to have diabetes and high blood pressure. The project aims to create circles of care activities grounded in local resources that support established cultural practices, local nutrition initiatives and culturally appropriate physical activity. The project is being delivered in Toronto and is expected to reach 40,000 participants.
Promoting healthy choices
The Canadian Cancer Society’s Walk or Run to Quit (WRTQ) initiative focuses on reducing commercial tobacco use and increasing physical activity by combining an evidence-based 10-week smoking cessation curriculum with a coach-led run/walk program. In 2020, the Canadian Cancer Society and Running Room with evaluators from the University of British Columbia will pilot community-based and locally adapted WRTQ programs in 30 communities across Canada. The program will build community capacity by combining the accessibility of web-based tools with the proven benefits of in-person accountability and peer support to help participants quit smoking while improving their overall physical and mental health.
Capsana’s Activate Your Health project motivates and supports employees in the workplace, particularly women aged 25 to 54, to improve their eating habits and physical activity. Participants take part in an initial health assessment and various workplace activities and are encouraged to maintain a healthier lifestyle throughout the year with practical tools, aids and resources. Employers help by providing a workplace that facilitates the adoption of a healthy lifestyle. The project is being carried out mainly in Quebec and should reach up to 6,000 participants over a period of three years.
The Centre for Addictions and Mental Health’s Picking up the PACE (Promoting and Accelerating Change through Empowerment) aims to increase the capacity of care providers to address other modifiable risk behaviours (e.g., physical inactivity, excessive alcohol use and poor diet) as a part of smoking cessation treatment. This initiative includes developing an online training curriculum for care providers outlining strategies and techniques and designing a just-in-time clinical decision support system that will guide care providers. This project is expected to reach 350 care providers and 4,500 participants.
The Community Food Centres Canada’s Food Fit: Promoting Healthy Eating and Fitness in Low-Income Communities project works toward increasing knowledge about nutritious foods, cooking/food preparation skills and physical activity, with a focus on social supports and community connection. Food preparation sessions, healthy and affordable recipes, easy-to-understand nutrition information, walking and home fitness routines, physical activity in groups and shared meals support participants to make measurable changes in their overall health and fitness. This national project is expected to reach 3,000 participants.
Improving our understanding of what contributes to the risk of developing dementia
The PURE-MIND study funded by Heart & Stroke in Canada aims to study 1,500 people in midlife who have had covert strokes and determine their risk for memory/thinking problems or dementia later in life. Covert strokes are small strokes in the brain that cause only very subtle symptoms. About a third of all dementia is related to stroke, and the two share common risk factors.
The New Brunswick Brain Health Initiative: Preventing Alzheimer’s by Lessening Modifiable Risk will offer participants advice on lifestyle modification, cognitive training and exercise with the aim of reducing their risk of developing dementia. It will also evaluate risk factors for dementia in New Brunswick. People at high risk for developing dementia will be the focus of this effort. This work is being led by Chris McGibbon (University of New Brunswick) and Pamela Jarrett (Horizon Health Network) across 5 sites throughout New Brunswick in collaboration with the Canadian Consortium for Neurodegeneration and Aging.
The project Preventing the progression of Alzheimer’s disease pathology by targeting the effects of lifestyle factors and personality traits, led by Sylvia Villeneuve (McGill University, CIUSSS de l’Ouest-de-l’Île-de-Montréal-Douglas Hospital, Montreal), focuses on two key objectives. The first is to identify lifestyle and personality factors associated with protein build-up in the brains of healthy asymptomatic older adults at risk of developing dementia; the second is to determine if some lifestyle and personality factors can counteract the negative effects of having a genetic risk associated with developing dementia. It is expected that this multidisciplinary study will give insights about new, sex-specific prevention strategies for dementia.
A research team is focused on advancing knowledge about how the brain’s resistance to damage and its ability to change is linked to age-related neurodegenerative diseases. This team, led by Sylvie Belleville (Université de Montréal and Institut Universitaire de Gériatrie de Montréal) and Nicole Anderson (Baycrest and University of Toronto), has created a program that combines training in memory and attention strategies with stimulating leisure activities that include learning music or a second language, joining documentary film discussion groups, and playing video games. The team is also developing strategies to make cognitive training programs accessible to Canadians using new technologies, such as virtual reality and online learning platforms.
Improving the knowledge and skills of the health care workforce
To enable health care professionals, professors and students across Canada who are working and studying in French to provide quality care, the University of Ottawa has developed French-language resources to improve knowledge and encourage safe and effective intervention practices. An online workshop, Découvrir les troubles neurocognitifs afin d’optimiser mes interventions, provides information on neurocognitive disorders and modifiable risk and protective factors to improve assessment, intervention and management methods. This workshop, developed and maintained by the Consortium national de formation en santé (CNFS) – University of Ottawa Component, undergoes a major overhaul every five years to stay up to date. Evidence-based content related to the most common neurocognitive disorders is also being developed and provided online on the Atteintes et pathologies microsite.
National objective: Advance therapies and find a cure
Understanding dementia better
Determining the impact of high blood pressure on the blood vessels within the brain is important since these vessels are responsible for delivering oxygen and nutrients needed to maintain a healthy brain. Examining blood vessels in the brain using live imaging techniques, researchers have measured the impact of high blood pressure on perception, thinking, reasoning and memory. Findings from this research indicate that hypertension accelerates the progression of Alzheimer’s disease and that recovery is better when a combination of treatments targeting both hypertension and amyloid pathology in the brain is used. This work is led by JoAnne McLaurin, Clifford Librach, Bojana Stefanovic at the Sunnybrook Research Institute (University of Toronto).
COMPASS-ND is a large-scale clinical study designed to learn about who is at risk of developing dementia, determine how early dementia can be detected, and find out what tests are most effective at detecting dementia. A research paper using COMPASS-ND data, published in 2019, shared findings that current guidelines for screening for frailty in individuals over 70 years of age need to be improved for people living with dementia. The paper notes that gait speed can be used as a screening method to detect pre-frail individuals at risk of dementia and that addressing frailty may contribute to delaying the onset of dementia and slowing its progression.
Genetic information can be modified in the cell through a process called epigenetics, which involves modifying DNA but not its sequencing. A research project investigating the role of genetic signals in the brain using brain imaging in people diagnosed with pre-dementia due to Alzheimer’s disease is focused on revealing new treatments. It is suspected that protein masses that accumulate in the brain during the aging processes suppress genetic signals necessary to keep the brain healthy. Epigenetics is part of important mechanisms underlying dementia. This project is being led by Pedro Rosa-Neto, Serge Gauthier and Joseph Therriault at the Centres intégrés universitaires de santé et de services sociaux de l’Ouest-de-l’Ile-de-Montréal-Douglas Hospital, McGill University.
Weihong Song of the University of British Columbia, and a Canada Research Chair in Alzheimer’s Disease, is studying the causes of dementia and developing new disease-modifying treatments. He is conducting studies to identify the molecular mechanisms that underlie the pathology in the brain that leads to dementia. In addition, he is working to discover new biomarkers or indicators of diseases and drug targets for Alzheimer’s disease, one cause of dementia.
Innovative therapies
A French Music Therapy Program reflects the recognition of the positive effect of music on the quality of life of people living with dementia. Emerging research is showing how music can assist in stimulating memory and slowing down the progression of dementia. This program offers free loans of headphones, speakers and digital music players containing personalized playlists of French music that has been selected for each individual to help French-speaking Yukoners retain language and promote memory. Run by the Yukon Francophone Health Network and the Department of Health and Social Service, the service is available to French-speaking Yukoners living with dementia, whether they are in care, at a hospital or at home.
Disruption of sleep and awake cycles in people living with dementia worsens over time, leading to confusion, nocturnal wandering and daytime irritability, increasing the burden on care providers both in homes and in institutional facilities. A University of Toronto project led by M. Cynthia Goh and Venkat Venkataramanan has developed the Adaptive Lighting for Alzheimer and Dementia INtervention (ALADIN), a versatile light system that improves sleep quality. ALADIN works as a wake-up lamp and a daytime ambient light with auto colour tuning that mimics natural sunlight. It promotes better sleep and awake cycles and is expected to help improve cognitive and emotional wellbeing of people living with dementia
To track and improve the physical and cognitive health of people living with dementia at home, sensor-based software platforms can assist with managing and monitoring the physical and cognitive health of people living with dementia who live at home. Ambient sensors gauge the activities of daily living while 3D-vision sensors can observe postures and movements of a personalized exercise routine and can analyze flexibility, balance, and ability to follow instructions. Tablet-based games designed to produce and monitor changes in cognitive ability can test perceptual and cognitive skills, record performance on increasing levels of difficulty, and provide cognitive-status indicators. These types of software-based tools provide engaging and innovative cognitive and physical training and the information gathered can help health professionals better assess physical and cognitive health and capacity. This project is led by Eleni Stroulia at the University of Alberta.
Focused ultrasound is a noninvasive, breakthrough technology for the treatment of neuro-degenerative diseases including dementia that uses sound waves to exert a therapeutic effect on tissues and has been shown to be safe and feasible. Researchers have been able to quickly develop a fully controllable, low-cost, and portable method. The findings of this initial research may have a large impact on diagnosis and treatment of brain disease. The goal is to revolutionize the treatment of dementia by accelerating the development of ultrasound technology to enable personalized treatment. This work is led by Kullervo Hynynen in collaboration with Isabelle Aubert, Nir Lipsman and Sandra Black from the University of Toronto (Sunnybrook Research Institute and Sunnybrook Health Sciences Centre).
A research team is developing innovative and affordable solutions to improve pain management for people with dementia who reside in long-term care facilities. This includes work toward an automated system that uses facial recognition technology and artificial intelligence to monitor pain in people with severe dementia; the development and evaluation of an application to facilitate assessments by care providers; and online training for care providers in rural and remote long-term care facilities. Researchers are fast tracking the sharing of better pain care information through a social media campaign: #SeePainMoreClearly. This project is being led by Thomas Hadjistavropoulos (University of Regina) and Babak Taati (Toronto Rehab Institute/University of Toronto).
Inclusive dementia research
A program introduced in Phase II of the Canadian Consortium on Neurodegeneration and Aging (CCNA) is enabling people living with dementia and care partners (i.e., friends, family and caregivers) to actively participate in the research process, including priority setting. The Engagement of People with Lived Experience of Dementia program supports the involvement of people living with dementia in the entire research process, including working with research teams and crosscutting programs and partners. This collaboration advances methods of engagement, including for persons with dementia and care partners, by incorporating evaluation processes that will measure their impact. In spring 2020, the CCNA began recruiting Advisory Group members who will have the opportunity to share personal lived experiences as collaborators in planning, conducting and communicating CCNA research on dementia.
Researchers at the University of British Columbia (UBC) are working with people living with dementia through participatory action research. A team led by Alison Phinney and Deborah O’Connor of UBC and Jim Mann, a person living with dementia, is learning how communities can “turn stigma on its ear” and promote active social participation of people living with dementia. Researchers from UBC, Simon Fraser University and Lakehead University are working with a group of people living with dementia to gather in-depth information through focus groups, workshops, interviews and observation. They will develop a framework defining the concept of social citizenship and identify best practices for respecting citizenship.
National objective: Improve the quality of life of people living with dementia and caregivers
Staying active and engaged and supporting inclusion
The Dementia-Inclusive Choices for Exercise (DICE) initiative aims to increase accessible exercise opportunities for people living with dementia. Led by Laura Middleton (University of Waterloo), researchers, people living with dementia, care partners, and community organizations are equal partners. To support inclusion, evidence-based tools were co-developed to prepare exercise providers to accommodate people living with dementia. DICE tools are being piloted in the Kitchener-Waterloo region, in northern British Columbia (Prince George, Kitimat), and Halifax.
In January 2018, an interdisciplinary research team at the University of Victoria launched a community choir for people living with dementia. Voices in Motion is an intergenerational choir for adults with dementia, caregivers, friends and students. Research indicates that participation in the choir enhances quality of life for people with dementia and caregivers by reducing distress, anxiety, stigma and depression, while improving social connections. This initiative also increases intergenerational friendships and understanding of dementia among high school choir members. Currently, there are 5 Voices in Motion choirs in Victoria with over 250 choristers as well as NoteWorthy Singers in North Vancouver, which is inspired by Voices in Motion and the desire to create a more dementia-inclusive community.
A research project led by Susan Cox and postdoctoral researcher Gloria Puurveen (University of British Columbia) is using the lenses of shared decision-making, feminist care ethics and social citizenship to look at how people living with dementia could become active collaborators in shaping end-of-life decision-making. This work employs qualitative and arts-based methods to enhance understanding of the views of people living with dementia in discussions about living well to the end of life. This work also contributes to the development of practical and policy-oriented approaches that support communicating their preferences about health and social care priorities at a local and national level.
The Volunteer Companion Program delivered by the Alzheimer Society of Prince Edward Island is a one-on-one home visiting program for people living with dementia and their caregivers who are at risk of social isolation. Volunteer companions visit once a week to provide socialization, mentorship and meaningful activities. Weekly visits offer caregivers an opportunity for respite and assists them in keeping their loved ones at home longer. Volunteer companions also support healthy aging in the community by engaging people living with dementia in meaningful activity in the comfort of their own home.
Cracked: new light on dementia is an innovative research-informed theatre production and film that is focused on the challenges of stigma, which is socially isolating and threatens quality of life as well as dementia care practices and policies. Developed in Toronto by Sherry Dupuis, Pia Kontos, Christine Jonas-Simpson, and Gail Mitchell, with playwright/director Julia Gray, actors, people living with dementia, family members and professionals, Cracked has been seen across and outside Canada by professional and public audiences. The Cracked team is currently exploring how different audiences engage with Cracked messages and is developing an interactive web-based learning platform.
The aim of the Supporting Inclusion through Intergenerational Partnerships Collective Impact initiative led by the Schlegel-UW Research Institute for Aging Foundation is to develop intergenerational partnerships that promote the social inclusion of seniors with mild to moderate dementia and caregivers located in the Waterloo, Ontario region, by creating opportunities to engage with youth. This intergenerational project will bridge gaps between research, education and practice by bringing together students and educators with community agencies that support seniors, municipal service providers, researchers, people living with dementia, caregivers, policymakers, and other stakeholders to collaborate on initiatives, co-create new learning opportunities for secondary and post-secondary students, and develop a culture of shared learning among community partners.
The Alzheimer Society’s nationwide anti-stigma campaign, “Yes. I live with dementia. Let me help you understand.”, highlights the diverse lived experience of Canadians living with Alzheimer’s disease and other forms of dementia to address misconceptions and reduce stigma.
Increasing access to dementia care
Dementia Assessment Units (DAUs) in Saskatchewan aid in assessing the needs of individuals who live at home and/or with home care support and residents living in a publicly funded Special Care Home whose challenges are difficult to manage in the community or in long-term care. The goal of a DAU is to stabilize these individuals and develop a care plan in order to better manage their care in their own home. Resource teams in Regina and Saskatoon provide outreach support, assist in the admission approval process and provide transitional support for individuals who are admitted to the unit and then discharged back to their home environment (e.g., personal home or Special Care Home).
My Health Teams in Manitoba are teams of care providers that work together to plan and deliver coordinated, comprehensive and high-quality primary care focused on geographic areas or specific communities or populations. This initiative may assist people living with dementia in getting earlier access to diagnosis and treatment while promoting improved service coordination and outreach. My Health Teams are focused on ensuring that people living with dementia and their families have access to regular, efficient and ongoing care built around their health needs.
The summer school at Glendon College in Ontario brings together health stakeholders working in Francophone university and community sectors. The goal is to improve the day-to-day practice of professionals in the field of aging and cognitive health in support of Francophone minority communities; integrate and support caregivers in service programming and promote their participation in “citizen science” projects; and to promote the sharing of best practices in cognitive health and dementia.
The Home Dementia Care Program in Newfoundland and Labrador helps people with moderate to advanced dementia live well at home by increasing access to medical care. This program, led by physicians and nurse practitioners in regional health authorities, aims to decrease the number of falls, reduce the use of inappropriate medication and emergency department visits, and delay or prevent long-term care placement while also supporting caregivers. Currently, approximately 150 people in the Eastern Health region have benefited from the program and planning is underway to expand to other regions in 2020.
Primary care memory clinics in Ontario help meet diverse needs. The Multispecialty Interprofessional Team (MINT) Memory Clinics (formerly known as Primary Care Collaborative Memory Clinics) provide timely dementia care in primary care settings. Initially started by Linda Lee in 2006, there are now over 110 locations across Ontario, involving more than 1,200 trained healthcare professionals and family physicians, and more than 50 supporting specialists. In a recent independent evaluation commissioned by the Government of Ontario, MINT Memory Clinics were associated with positive outcomes such as lower healthcare system costs and delayed transition into long-term care. The Geriatric Assessment and Intervention Network (GAIN) teams are nurse practitioner-led and geriatric medicine-supported interprofessional teams who serve complex seniors with cognitive and physical decline. All referrals, including self-referrals, initiate comprehensive geriatric assessments. Treatment, care planning and education augmented with in-home evaluations, behavioural support clinicians and intensive care management can often change lives. The 11 GAIN teams of Central Eastern Ontario, unique in Canada, annually support over 9,000 individuals and families with dementia in urban, rural and remote communities. GAIN teams are a sustainable alternative for dementia diagnosis and care within the community.
Person-centred care
Upon admission to a long-term care home in Yukon, the Continuing Care Therapy Services program offers individualized assessment to everyone, including people living with dementia, by an occupational therapist, physiotherapist, recreation therapist and/or speech-language pathologist. Assessment may include cognitive screening and assessment of need for functional supports.
In the Northwest Territories, the Supportive Pathways model of care uses a person-centered approach that fosters respectful, compassionate dementia care. The approach teaches staff to deliver individualized care responsive to each resident in a home-like supportive environment. Training on Supportive Pathways is provided to Home Care and Long Term Care staff, clients and families across the Northwest Territories by the Northwest Territories Health and Social Services Authority, in collaboration with the Tlicho Community Services Agency and the Hay River Health and Social Services Authority.
Co-designing Dementia Care in New Brunswick: Building the Future Together aims to design, deliver, and evaluate the approach to dementia care. The goal is to improve the knowledge of primary care providers around diagnosis and delivery of dementia care, as well as awareness of services among seniors at risk for dementia and their care partners. This project is led by Shelley Doucet and Alison Luke (UNB Saint John) and Pamela Jarrett (Horizon Health Network) and is one part of a larger international project supported through the CCNA.
Behavioural supports
Behavioural Supports Ontario (BSO) provides behavioural health services for older adults with, or at risk of, responsive behaviours/personal expressions (e.g., repetitive questions, apathy, pacing, screaming, grabbing) associated with dementia and other neurological conditions. In addition to supporting the person, BSO teams support family care partners and healthcare providers in community, long-term care, acute care or wherever the person resides. BSO teams provide comprehensive behavioural assessments and collaboratively develop person-centred behavioural support plans. BSO Teams are available across Ontario, united by the leadership of the BSO Provincial Coordinating Office at the North Bay Regional Health Centre.
In Montreal, a specialized interprofessional team has been set up to assist in complex situations involving people living with Alzheimer’s disease and neurocognitive conditions. The goal is to reduce problematic behaviours and find strategies to improve the quality of life of those living with these conditions and of caregivers. Evidence-based methods are proposed to initiate non-pharmacological interventions, adapt the environment, reduce restraints, and avoid the use of emergency departments and early placement in a care home. The team contributes to knowledge transfer and research and offers telehealth activities that make its expertise accessible to care providers throughout Quebec (Centre intégré universitaire de santé et de services sociaux du Centre-Sud-de-l’Île-de-Montréal).
The Behavioural and Psychological Symptoms of Dementia (BPSD) Algorithm is available to all care providers in British Columbia—it is an electronic interactive tool that supports interdisciplinary, evidence-based and person-centred clinical assessment and care decisions for persons with BPSD. The BC BPSD Algorithm has a specific focus on non-pharmacological interventions and the appropriate use of antipsychotic drugs in long-term care settings. This project was a provincial collaborative effort led by Interior Health and is designed to be used in combination with the BPSD Best Practice Guideline. The guideline and algorithm offer evidence-based tips and tools to all care providers in the province to support the delivery of best practices in non-pharmacological approaches to person-centred dementia care.
Canadian Foundation for Healthcare Improvement (CFHI) has supported more than 300 long-term care homes across the country to provide more person-centred dementia care and ensure antipsychotic medications are used appropriately. The Appropriate Use of Antipsychotics approach engages people living with dementia, families and staff to understand underlying causes of behaviours and consider safely reducing or discontinuing medication. This decreases risks of negative health outcomes and improves their experience of life. Rates of potentially inappropriate antipsychotic use are declining in Canada: in 2013-14, about 1 in 3 long-term care residents without a psychosis diagnosis were prescribed an antipsychotic and in 2018-19, the rate was 1 in 5.
Skills, training and tools for care providers
Alberta’s Health Care Aide (HCA) curriculum, updated in 2019, describes required skills, knowledge, behaviours and attitudes to help HCAs. The 2018 HCA Competency Profile includes enhancements related to dementia, palliative and end-of-life care, and addiction and mental health. This new curriculum has more theory, applied labs, and clinical experiences so that HCAs can learn more interactively and apply what they learn so that they can better understand and support the needs of people living with dementia. Alberta Health will rescind the License Agreements with all post-secondary institutions delivering the Provincial Curriculum on July 1, 2020. Post-secondary institutions must apply for a new License Agreement to deliver the new Provincial Curriculum.
The Dementia Care Pilot Project in Nova Scotia is evaluating an online dementia education program and screening tools for primary care providers to use in family practice. This project aims to support primary care providers to earlier diagnose, treat and manage patients who have dementia-like symptoms. Two collaborative family practice teams (one urban, one rural) including general practitioners, nurse practitioners, licensed practical nurses, family practice nurses, and social workers are participating in the pilot project. Use of the screening tools is being tracked in clinicians’ practices and an evaluation is underway to assess the education program and screening tools for further expansion.
Support for caregivers
Caregivers for people living with dementia assist with activities of daily living and help with advance care planning, often their own health needs are not addressed. Improving support for caregivers is an area of focus of the national dementia strategy and examples of initiatives underway across Canada that support dementia caregivers include:
Building knowledge
Through the Healthy Seniors Pilot Project in New Brunswick, Introducing Gentle Persuasive Approaches in Dementia Care aims to strengthen the knowledge of formal (paid) and informal (unpaid and often family/friend) caregivers by implementing gentle persuasive approaches in homes of people living with dementia and Special Care Homes. Caregivers of people living with dementia often state there is little education on how to deal with responsive behaviours. This education program has been shown to be effective in meeting this need in acute care and long-term care settings. This project will evaluate the benefits of this approach for caregivers and people living with dementia, and it will be the first time this approach is implemented (e.g., GPA training program and additional education) and evaluated with informal caregivers. The Alzheimer Society of New Brunswick together with Horizon Health will pilot this project in Moncton with the potential to expand provincially and nationally once successful outcomes are demonstrated.
The Community Dementia Ambassador Training pilot program provides resources and in-person supports to partners and caregivers of people living with dementia in small remote communities in the Northwest Territories. The program, delivered by the Alzheimer Society of Alberta and the Northwest Territories, is active in three communities with four Dementia Ambassadors, two of whom are Indigenous language speakers. By building connections and relationships in their communities, Ambassadors can address cultural values about dementia and community norms at a local level.
In Yukon, the Shine a Light on Dementia: Caregiver Training Program aims to equip caregivers with knowledge and skills on dementia, including: general knowledge; approaches to care and strategies for caregivers; grief management and self-care for caregivers; legal and financial matters; and palliative care. This 6-week training program, delivered by the Yukon Department of Health and Social Services, brings care providers and caregivers together to share experiences, information and resources on dementia, to learn best practices, and support one another so they can provide quality care for people living with dementia.
The University of Alberta in partnership with caregivers, community organizations and researchers in Saskatchewan, Manitoba, Ontario and Quebec are developing and evaluating an online platform to support caregivers of people living with dementia who live in long-term care. Throughout 2019-20, focus groups with caregivers were held to inform My Tools 4 Care-In Care. A formal evaluation is now underway. This web-based platform will provide interactive activities, resources and guidelines to support caregivers to improve mental wellbeing by fostering social inclusion and to building skills and knowledge in working with long-term care providers.
Financial support
The Government of Nova Scotia Caregiver Benefit Program provides funding to eligible caregivers who are providing assistance to qualified care recipients residing in the community. The program, administered by the Nova Scotia Health Authority, is intended for caregivers of low-income adults with moderate cognitive and high physical impairment. The goal of the program is to recognize the important role of caregivers in their efforts to assist loved ones and friends while helping sustain the support they provide.
Federal personal income tax assistance is provided in recognition of the fact that people living with dementia and those who care for them may have a reduced ability to pay tax. Examples of such measures include the Medical Expense Tax Credit, Disability Tax Credit, and Canada Caregiver Credit.
Community-based services
The Community-based Innovations for Dementia Care initiative provides funding to 14 local community and health service providers in Alberta to implement projects that build innovative approaches in person-centred dementia services. These projects will support people living with dementia and caregivers to participate fully in their communities and work toward reducing stigma. Projects will aim to optimize independence, quality of life and wellbeing and will span the province in both urban and rural communities. Examples of projects include dementia-friendly programming at a public library and an integrated theatre project. This work follows Alberta’s 2016 community innovation grant initiative, which supported eight projects.
The Home and Community Care Program provides home and community care services in all communities throughout Nunavut, such as home support and respite care for caregivers as well as for Nunavummiut diagnosed with dementia-related illness who are able to be supported at home. A new 24-bed long-term care facility will provide around-the-clock nursing care and will be designed and programmed to support the medical and cultural needs of a growing population of Nunavut seniors. Construction is expected to be completed by fall 2023.
Cross-cutting efforts
Sharing information resources
The P.I.E.C.E.S.™ Learning and Development Program delivers learning resources to those caring for older adults with complex physical and cognitive and mental health needs as well as behaviour changes in British Columbia, Nova Scotia, and the Yukon. The P.I.E.C.E.S.™ model has been integrated into care provision and daily practices in various settings throughout all five of BC’s regional health authorities since 2013. Health authorities continue to regularly deliver training to care providers (regulated and unregulated) across the continuum of care in BC. Yukon continues to use P.I.E.C.E.S.™ resources in daily practice and in coaching with staff throughout Yukon long-term care homes.
U-First! Education, offered by the Alzheimer Society of Nova Scotia, uses the P.I.E.C.E.S.™ model to improve the quality of the interaction between care providers and people living with dementia. This program is a 6-hour workshop for unregulated health workers in home support and long-term care to better understand responsive behaviors. It aims to help develop a common knowledge base, language, values and approach to confidently care for people with dementia. The Alzheimer Society of Nova Scotia is also delivering U-First! for Care Partners to integrate families into the care system as valuable team members with the same shared understanding and approach to care.
Provincial Alzheimer Societies in British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador are providing the First Link Program, which offers services and support at the time of diagnosis and throughout the duration of the condition. People living with dementia and their families are linked to learning, services and support as early as possible upon diagnosis. First Link helps to bridge the gap between service providers within the circle of care.
The Dementia Association for Awareness and Support, developed in Edmonton, Alberta, provides people living with dementia and caregivers with access to educational resources and support tools. The podcast titled “Life with Dementia” shares educational resources on the latest tips, lifestyle adaptations and best practices for managing dementia and reducing emergency room visits. An online technology platform, Tusk, is also under development to assist caregivers with navigating the complex medical system. This tool matches the needs of people living with dementia and their caregivers with available resources and service providers in the local community.
Focusing on those at higher risk and facing barriers to equitable care
Rural and remote communities
The Rural Dementia Action Research (RaDAR) Team in Saskatchewan aims to improve access to appropriate care from early to late stage dementia, and from community to facility-based care. The RaDAR Team of researchers at the University of Saskatchewan, accomplishes its objectives through research, mentoring and knowledge exchange.
The Rural and Remote Memory Clinic (RRMC), developed alongside the RaDAR Team, increases the availability and accessibility of dementia care in rural and remote areas and focuses on the diagnosis and management of atypical and complex cases of suspected dementia. Individuals and families are provided with information about the probable diagnosis, feedback based on the clinical assessment and investigations, and recommendations for management and care.
The Primary Health Care Integrated Geriatric Services Initiative supports increasing capacity across primary health care teams in predominantly rural communities in Alberta to provide support for people living in the community impacted by dementia. Education and partnerships among local health, social, community, and municipal organizations support the development of measuring and monitoring for wellbeing at the individual and community level. This initiative also supports the development of a competency framework for teams working with people living with dementia.
The University of Regina is leading the Interventions to Enhance Social Inclusion of Older Adults with Dementia in Saskatchewan Collective Impact project (2019–2024), working with not-for-profit, profit and academic sectors. The project will aim to increase the social inclusion of people living with dementia over the age of 55 and caregivers in small cities and rural or remote communities in Saskatchewan. Participatory research will be used to develop, implement and assess initiatives that support social inclusion of people living with dementia.
Ethnic and cultural minorities
The Alzheimer Society of Nova Scotia is working with the Health Association of African Canadians (HAAC) to facilitate dementia education in Black communities across Nova Scotia. A Cultural Competence workshop held on September 16, 2019, at the Black Cultural Centre in Halifax brought together Alzheimer Society staff and HAAC volunteers to prepare the way for effective ongoing partnerships. An education session was adapted to explore the needs of people of African ancestry living with dementia in Nova Scotia including culturally specific content and information reflective of Nova Scotia’s Black communities. Working with regional staff and HAAC volunteers, 11 education sessions and facilitated community conversations were held across Nova Scotia. As a result, existing services such as the ASNS Infoline and adapted print materials are being accessed.
Official language minority communities
Exploratory research in Ottawa by Corine Carbonneau and Marie Drolet, La trajectoire des services sociaux et de santé d’aînés atteints d’une démence vivant en contexte francophone minoritaire: un engagement de multiples piliers durant une navigation complexe, highlights the role of navigators in securing access to quality care in official language minority communities. People with dementia and their caregivers need to be referred to existing services. In a minority language situation, this interaction with resources is even more crucial because of the scarcity of these resources, and the related limits to access to quality care and services. As a result, the navigator enhances the capacities of the care providers.
Few resources to train health professionals on dementia and cognitive health are available in French and there is a growing demand for bilingual health care in southern Ontario. This is particularly challenging for communities that are far from urban centres. Glendon College, the bilingual campus of York University, offers an online certificate in dementia and cognitive health. This training responds to the need for access to quality care in French that is evidence-based and delivered by health professionals with a good knowledge of the factors that can influence cognitive health. The College also offers a specialization stream in cognitive neuropsychology to its undergraduate students. These programs meet the needs of Francophone professionals and professionals-in-training across Canada who want to better serve their patients, especially seniors.
Work is underway at the University of Moncton to develop and assess a tool for care providers that is evidence-based and culturally and linguistically adapted to a Francophone population, using the Neurocognitive Frailty Index. This project, led by Professor Sarah Pakzad, is expected to promote and support the early diagnosis of dementia and reduce the potential for linguistic barriers to care. It is expected to be available to all Francophone health professionals in Canada, including those working in official language minority communities by 2021 or early 2022.
Bibliography
Alzheimer Society of Canada. Prevalence and monetary costs of dementia in Canada. Alzheimer Society of Canada. 2016.
Alzheimer Society of Ontario. Dementia friendly communities. Alzheimer Society of Ontario. 2019.
Canadian Chronic Disease Surveillance System 2016–2017, cited in: Center for Surveillance and Applied Research, Public Health Agency of Canada. Canadian Chronic Disease Indicators Data Tool, 2019 Edition. Public Health Infobase. 2019.
Griffith L, Gruneir A, Fisher K, et al. Patterns of health service use in community living older adults with dementia and comorbid conditions: a population based retrospective cohort study in Ontario, Canada. BMC Geriatrics. 2016; 16(177) 1-10.
Livingston G, et al. Dementia prevention, intervention, and care. The Lancet. 2017; 390: 2673–734.
Preliminary data from EKOS’ Dementia Survey 2020 for the Public Health Agency of Canada.
Public Health Agency of Canada. A dementia strategy for Canada: Together we aspire. Government of Canada. 2019.
Public Health Agency of Canada. Dementia in Canada. Government of Canada. 2019.
Public Health Infobase. Canadian chronic disease surveillance system (CCDSS). Government of Canada. 2019.
Shi L, Chen S, Ma M, et al. Sleep disturbances increase the risk of dementia: A systematic review and meta-analysis. Sleep Medicine Reviews. 2018; 40(1) 4-16.
World Health Organization. Risk reduction of cognitive decline and dementia : WHO guidelines. World Health Organization. 2019.
Endnotes
- Footnote 1
-
Please note that some of the websites this report links to may not have content in both English and French.
- Footnote 2
-
Throughout this document the term ‘caregivers’ will be used to refer to this group.
- Footnote 3
-
The delivery of some initiatives highlighted in this document may have been or are currently impacted by the COVID-19 pandemic.
- Footnote 4
-
Inclusion of initiatives in the annual Report to Parliament by the Public Health Agency of Canada does not constitute an endorsement. PHAC has worked with organizations whose initiatives are featured here to ensure descriptions are accurate but cannot guarantee it.
- Footnote 5
-
Preliminary data from EKOS’ Dementia Survey 2020 for the Public Health Agency of Canada.
- Footnote 6
-
Canadian Chronic Disease Surveillance System 2016–2017, cited in: Center for Surveillance and Applied Research, Public Health Agency of Canada. Canadian Chronic Disease Indicators Data Tool, 2019 Edition. Public Health Infobase. 2019. Available from: https://health-infobase.canada.ca/ccdi/data-tool/
- Footnote 7
-
Internal data from the Canadian Institutes of Health Research
- Footnote 8
-
Note: this number includes an estimate of indirect trainees for applications where number of trainees were not directly reported. The estimate is calculated based on the amount spent on students divided by average student salaries, based on recent Canadian Institutes of Health Research internal data.
- Footnote 9
-
Parts of these materials are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions and statements expressed herein are those of the author and not necessarily those of the Canadian Institute for Health Information. This data was drawn from the RAI Home Care (RAI HC)—HCRS, fiscal year 2018–2019. It is representative of people living with dementia receiving homecare in British Columbia (all regions except Northern Health), the Yukon, Alberta (except the Calgary Zone), and Newfoundland and Labrador.