Framework for diabetes in Canada
Download in PDF format
(2.37 KB, 46 pages)
Organization: Public Health Agency of Canada
Date published: 2022-10-05
Table of contents
- Minister's message
- Executive summary
- Introduction
- Diabetes in Canada
- Context: Momentum on diabetes
- Framework: An approach to address diabetes in Canada
- Cross-cutting principles
- Framework components
- Moving forward
- Appendices
- Appendix A: National Framework for Diabetes Act
- Appendix B: Engagement process
- Appendix C: Roles and responsibilities in Canada to address diabetes
- Appendix D: Strategies and frameworks addressing diabetes and chronic disease
- Appendix E: Glossary
- Appendix F: Visual of the Framework for diabetes in Canada
- References
Minister's message

I am privileged to share the Framework for Diabetes in Canada (Framework). Diabetes is one of the most common chronic diseases affecting people living in Canada, and continues to be on the rise. The COVID-19 pandemic has also disproportionately impacted Canadians living with diabetes, given their increased risk for severe disease or outcomes, compounded by health inequities. The release of the Framework marks an important milestone in our efforts to better recognize, collaborate with, and support those impacted by diabetes in Canada.
The Framework was informed by a phased engagement process, including key informant interviews, dialogues, and an online feedback tool involving diverse stakeholders and partners, including people with lived experience. Perspectives of provincial and territorial governments were also sought through existing federal, provincial and territorial mechanisms.
Indigenous Peoples in Canada carry a disproportionate burden of diabetes. Although the Framework includes the perspectives of several Indigenous stakeholders, in keeping with the Government of Canada's commitment to reconciliation and the right of Indigenous Peoples to self-determination, a nation-wide Indigenous-led engagement process on diabetes is underway to ensure that the unique rights, interests and circumstances of the First Nations, Inuit, and Métis are acknowledged, affirmed, and reflected in the supports available for Indigenous Peoples and communities affected by diabetes.
We are hopeful that many of the relationships built during the development of the Framework will continue to grow and support multi-sectoral efforts to address diabetes across Canada.
The Government of Canada recognizes the importance of helping Canadians reduce their risk of chronic diseases, and is taking action on many fronts. For example, the Government is supporting community-based initiatives that address common risk factors for chronic diseases, including diabetes, by promoting physical activity, healthy eating, and tobacco prevention and cessation. In addition, the Government is supporting research to addresses causes, prevention, screening, diagnosis, and treatment of chronic diseases, including all forms of diabetes.
While important efforts are underway by all levels of government, stakeholders and partners, more needs to be done to prevent diabetes and support those currently living with the condition in Canada. This includes taking action to address the underlying social, economic and environmental determinants that contribute to health inequities and increase the risk of developing chronic disease; improve our understanding of the different types of diabetes and how best to address them; share best practices; and tailor interventions to meet the diverse needs of key population groups.
I am grateful to those who have shared their experiences, advice, hopes and priorities for the Framework. It is my sincere hope that the Framework will guide our efforts to move the needle on diabetes in Canada by supporting environments and systems that reduce inequities and promote healthier living. The Framework provides a common direction to help align efforts across stakeholders and sectors, and to build on the many important initiatives and investments that are already in place to make a meaningful difference in the lives of those affected by diabetes.
The Honourable Jean-Yves Duclos, P.C., M.P.
Minister of Health
Executive summary
Diabetes is one of the most common chronic diseases affecting people living in Canada. There are three main types of diabetes in Canada: type 2 (90% of cases), followed by type 1 (9%) and gestational diabetes (less than 1%). Other types are uncommon. Although in all types of diabetes, the body does not produce enough insulin or use the insulin it produces effectively, each type may differ with respect to its potential causes, prognosis, and treatment. Over 3 million Canadians, or 8.9% of the population, have diagnosed diabetes and, after adjusting for the aging population over time, the prevalence has been increasing at an average rate of 3.3% per year. In addition, 6.1% of Canadian adults have prediabetes, putting them at high risk of developing type 2 diabetes.
Evidence shows that type 2 and gestational diabetes are more prevalent in certain populations, including racialized communities and communities facing marginalization. People living with all types of diabetes may experience various forms of discrimination and stigma associated with their condition, as well as intersectional factors like race, living situation, weight, and age. These experiences can lead to adverse mental and physical health outcomes.
Rates of diabetes are rising around the world, resulting in increased human and economic costs that affect individuals, communities, healthcare systems and societies. The World Health Organization (WHO) has identified diabetes as one of the major public health challenges of this century.
In Canada, there is an increased risk of severe disease or outcomes from COVID-19 for people with type 1 or type 2 diabetes. The COVID-19 pandemic is also having a disproportionate impact on Canadians facing marginalization, many of whom are at a greater risk of being impacted by the adverse health, social and economic effects of the pandemic. Further, COVID-19 public health measures such as physical distancing and self-isolation restrictions have delayed diagnosis, management and treatment, as well as exacerbated the prevalence of physical inactivity and other risk factors associated with chronic diseases, including diabetes. These risk factors are expected to remain an issue following the pandemic, and may lead to an even greater increase in rates of diabetes over time.
The year 2021 was an important year for diabetes. It marked the 100-year anniversary of the discovery of insulin by scientists at the University of Toronto. Many stakeholders organized or took part in activities to celebrate this important discovery, which has saved millions of lives worldwide.
Also in 2021, the Government of Canada announced $35 million for investments in diabetes, specifically, $25 million for diabetes research, surveillance, and prevention, as well as the development of a national framework for diabetes. This includes a recommitment to the Juvenile Diabetes Research Foundation (JDRF) and the Canadian Institutes of Health Research (CIHR) Partnership to Defeat Diabetes, by investing up to $15 million to be matched by JDRF Canada and its donors for type 1 diabetes research. Budget 2021 also announced $10 million for a new Diabetes Challenge Prize to help surface novel approaches to diabetes prevention.
The National Framework for Diabetes Act (the Act) passed in June 2021. The Act requires the federal Minister of Health to prepare a report setting out a national framework designed to support improved access to diabetes prevention and treatment to ensure better health outcomes for Canadians, in consultation with the representatives of the provincial and territorial governmentsFootnote * responsible for health, Indigenous groups and with other relevant stakeholders.
The Public Health Agency of Canada (PHAC), with the assistance of the Morris J. Wosk Centre for Dialogue based at Simon Fraser University, undertook a virtual engagement process (February to May 2022) to support the development of the Framework. A range of key stakeholders from diverse sectors had an opportunity to share their views, experiences and perspectives to help identify priorities for advancing efforts on diabetes in Canada, and to inform the development of a framework for diabetes. Existing strategies, frameworks and best practices in Canada and abroad were also considered in the development of the Framework. Input from provincial and territorial governments was obtained through three federal, provincial and territorial (FPT) mechanisms: FPT Group on Nutrition; FPT Sport, Physical Activity and Recreation; as well as the FPT Health Support Committee which reports to the FPT Deputy Ministers of Health.
Framework for diabetes in Canada
Several cross-cutting principles have been identified that are foundational to success in addressing the components of the Framework. The cross-cutting principles emphasize the importance of: addressing health equity; applying a person-centred approach; differentiating between types of diabetes; supporting innovation; as well as promoting leadership, collaboration and information exchange.
The Framework is comprised of six interdependent and interconnected components that represent the range of areas where opportunities to advance efforts on diabetes could be beneficial. The components include the following: prevention; management, treatment and care; research; surveillance and data collection; learning and knowledge sharing; as well as access to diabetes devices, medicines, and financial supports.
The principles and the components form a complex environment within which to create change in Canada. They were derived from and build on what was heard from people in Canada throughout the engagement process on diabetes.
Cross-cutting principles:
- addressing health equity
- applying a person-centred approach
- differentiating between types of diabetes
- supporting innovation
- promoting leadership, collaboration and information exchange
Framework components:
- prevention
- management, treatment and care
- research
- surveillance and data collection
- learning and knowledge sharing
- access to diabetes devices, medicines and financial supports
Diabetes is a complex disease, and there is still significant work ahead to ensure better health outcomes for people living in Canada. Effectively addressing diabetes prevention, management and treatment calls for a sustained, multi-sectoral response involving many actors, including the public, private, health and non-governmental sectors. All sectors and levels are invited to use the Framework to guide action to address diabetes and advance opportunities in ways that meet their respective mandates and objectives, and that are adapted to their respective community contexts. An inclusive and broad social determinants of health perspective and person-centred approach must be applied to respectfully and meaningfully move forward in addressing diabetes in Canada.
Introduction
The Framework for Diabetes in Canada (Framework) has been developed in accordance with A National Framework for Diabetes Act (the Act). The Act (Appendix A) requires the Minister of Health, in consultation with the representatives of the provincial and territorial governmentsFootnote * responsible for health, Indigenous groups and with other relevant stakeholders, to develop a national framework designed to support improved access to type 2 diabetes prevention and treatment for all types of diabetes to ensure better health outcomes for people living in Canada. The Act also requires the Minister of Health to table a report in Parliament within five years on the effectiveness of the Framework for Diabetes in Canada, and on the current state of diabetes prevention and treatment. This report must also set out the Minister's conclusions and recommendations regarding the Framework.
The Framework aims to provide a common policy direction to address diabetes in Canada, including for populations at elevated risk of developing diabetes, people living with diabetes and their caregivers, Indigenous populations, non-governmental organizations, health care professionals, researchers, and all levels of government. It lays the foundation for collaborative and complementary action by all sectors of society to improve access to diabetes prevention and treatment, and ensure better health outcomes for people living in Canada.
Diabetes prevention, management, treatment and care are most effective when approached holistically, taking into consideration people's physical, social, emotional, mental, spiritual and cultural well-being, as well as a range of broader contextual factors like the social determinants of health. This person-centered approach to addressing diabetes will be considered throughout the Framework by taking into account the experiences and knowledge of individuals living with diabetes.
Diabetes in Canada
Diabetes is a serious chronic disease, and one of the most common chronic diseases affecting Canadians. It poses many challenges for those living with the disease, their families and communities, and has various implications for health systems. There are three main types of diabetes: type 1, type 2 and gestational diabetes. Other types are uncommon. It is estimated that approximately 90% of cases are type 2, 9% are type 1 and other types and gestational diabetes account for less than 1% of all cases.Footnote 1 In all types of diabetes, the body either does not produce enough insulin or is unable to use the insulin it produces effectively. Each type of diabetes may differ with respect to its potential causes, prognosis, and treatment.
Types of diabetes
Type 1 diabetes is an auto-immune disease characterized by the inability of the pancreas to produce insulin, a hormone which regulates blood sugar. Daily insulin injections are required. It most often begins in childhood. Neither the cause nor the means to reduce the risk of acquiring it are known.
Type 2 diabetes occurs when the pancreas does not produce enough insulin or when the body does not effectively use the insulin that is produced. It is driven by a complex mix of risk factors, such as unhealthy eating, physical inactivity and tobacco use, and determinants of health related to income, education, and the social and physical environment. Genetic predisposition and obesity are also important risk factors for type 2 diabetes. Daily insulin injections may be required.
Gestational diabetes is first diagnosed during pregnancy. While often this condition goes away after delivery, there is a high risk that people with gestational diabetes and their babies may develop type 2 diabetes later in life.
Prediabetes refers to blood sugar levels that are higher than normal, but not yet high enough to be diagnosed as type 2 diabetes. The condition is associated with an increased risk of developing type 2 diabetes.
Over 3 million people living in Canada, or 8.9% of the population, have diagnosed diabetes and after adjusting for the aging population, the prevalence is increasing at an average rate of 3.3% per year. Further, 6.1% of Canadian adults aged 20-79 have prediabetes, putting them at high risk of developing type 2 diabetes.Footnote 2 This upward trend is expected to continue in the coming decades with the aging of Canada's population leading to increasing comorbidities and complications, and greater demand for resources from economic and health care systems.
Diabetes is a challenging health condition that disproportionately affects certain populations within Canada. Evidence shows that First Nations and Métis people, and people of African, East Asian and South Asian ethnic backgrounds have higher rates of type 2 diabetes compared to the general population. Inequities in the social determinants of health (e.g., income, education, housing), resulting from the impacts of systemic racism, intergenerational trauma and colonization, are associated with higher rates of type 2 and gestational diabetes in priority populations.Footnote 3 Similarly, socioeconomic factors influence the ability for individuals with diabetes to effectively manage their condition, and thus their risk of diabetes-related complications.
Diabetes is one of the most common chronic diseases among children and youth. Type 1 diabetes remains the main form of the disease in this population. While type 2 diabetes has historically been viewed as an adult disease, it has been on the rise globally in children and youth for the last two decades due to the rise in childhood obesity.Footnote 4 Footnote 5 According to national data from 2017–2018, just over 25,000 (0.33%) children and youth were living with diagnosed diabetes (type 1 and type 2 diabetes combined) in Canada. Each year, more than 3,000 individuals aged 1 to 19 years are newly diagnosed with diabetes. Further, the incidence of both type 1 and type 2 diabetes is expected to rise (by 3-fold and by 4-fold, respectively) in youth in the coming decades.Footnote 6 Footnote 7It has been observed that in Indigenous youth, type 2 diabetes progresses very rapidly and is more likely to result in serious complications, such as chronic kidney disease, at an earlier age and that both type 1 and type 2 diabetes have psychosocial impacts on individuals. One study noted that First Nations adolescents with a diagnosis of type 2 diabetes experience stigma and shame, which are substantial barriers to effective self-management of diabetes and seeking support and care for their condition.Footnote 8
Many people living with diabetes experience stigma associated with their condition, which can lead to adverse mental and physical health outcomes. Stigma often occurs when individuals are often blamed for their diagnosis of type 2 or gestational diabetes due to associations with certain biological or lifestyle factors, such as weight or eating patterns. People living with type 1 diabetes experience stigma associated with the intensive management of their condition, including dietary management, and hypoglycemic events. In both type 1 and type 2 diabetes, other people's perceptions of diabetes can lead to experiences of guilt, shame, embarrassment or isolation.Footnote 9 Footnote 10
The Chief Public Health Officer of Canada's 2019 Report on the State of Public Health prioritized understanding and acting on stigma across health systems, and recognized that systemic racism can have an impact on people affected by certain chronic diseases, such as diabetes. The Report noted that stigma in health systems can lead to non-disclosure of health conditions, delayed or decreased use of health services and poorer quality of health services received by those from stigmatized groups who do seek care.Footnote 11 Furthermore, some racialized groups, particularly Indigenous Peoples, may be further challenged by experiences of systemic racism and discrimination by some health care providers. Such experiences can be a significant barrier to health care access and also compromise the quality of care individuals receive when seeking health services and supports.
Diabetes exacts considerable physical, emotional and economic challenges to affected individuals and families. Effective management of blood glucose levels can reduce the risk of diabetes complications such as retinopathy, neuropathy, sight loss, heart disease, stroke, kidney disease and lower limb amputation.Footnote 12 In Canada, evidence shows that there is an increased risk of more severe illness or outcomes from COVID-19 for people with type 1 or type 2 diabetes.Footnote 13
Diabetes is the leading cause of non-traumatic lower limb amputations in Canadian adults, associated with 20 times the risk of being hospitalized with non-traumatic lower limb amputations.
Diabetes retinopathy is a leading cause of sight loss and disability. More than 60% of individuals with type 2 diabetes develop some form of retinopathy.Footnote 15
The social, political, health and environmental conditions that created differential risks for COVID-19 overlap with factors that drive inequities in chronic diseases, particularly for people living in Canada facing marginalization. Public health measures related to COVID-19, such as physical distancing and self-isolation restrictions, have had unintended negative consequences, including delayed diagnosis and treatment of diabetes and other health conditions. The pandemic context has also exacerbated physical inactivity, sedentary behaviours and other risk factors associated with chronic diseases, including diabetes.Footnote 14 Further, the pandemic highlighted challenges in health system capacity, food security and limitations in access to supports, programming and services. These risk factors are expected to remain an issue following the pandemic and may lead to an even greater increase in rates of diabetes over time.
Context: Momentum on diabetes
In Canada
A considerable amount of momentum has been building on type 2 diabetes prevention and management of all types of diabetes in recent years. The increasing prevalence of diabetes in Canada, and recent severe COVID-19 outcomes in people with diabetes, have activated Parliamentarians and stakeholders to call for a more coordinated and focused effort by the Government of Canada to prevent and manage diabetes.
The Standing Committee on Health (HESA) report entitled 'A Diabetes Strategy for Canada' was first tabled in April 2019 and re-tabled in April 2021. Over the course of six days, the committee heard from witnesses and received briefs from organizations representing diabetes such as Diabetes Canada, JDRF Canada, the National Aboriginal Diabetes Association, academics and health professionals. The report contains eleven recommendations to help provide more support to people living with diabetes and to prevent type 2 diabetes. One of the report's main recommendations was that the federal government work with the provinces and territories, and key stakeholders to create a national plan to help prevent and manage diabetes in Canada. The Government of Canada's response was tabled in Parliament on June 23, 2021. It highlighted the valuable perspectives included in the HESA report, as well as the federal government's commitment to the prevention of type 2 diabetes, the search for a cure for type 1 and type 2 diabetes, and the importance of the provision of treatment and support for people living with diabetes in Canada.
The year 2021 marked the 100-year anniversary of the discovery of insulin by scientists at the University of Toronto. Many stakeholders organized or took part in activities to celebrate this important discovery, which has saved millions of lives worldwide through the widespread use of insulin therapy for diabetes management. The Government of Canada worked with stakeholders to celebrate this remarkable Canadian discovery in various ways, including through the development of commemorative banners in collaboration with the University of Toronto.
Through Budget 2021, the Government of Canada demonstrated its commitment to addressing diabetes by providing $35 million over five years, starting in 2021-22. In particular, Budget 2021 announced $25 million for investments in research, surveillance, and prevention, and to work towards the development of a national framework for diabetes. As part of these investments, the Government of Canada, through the CIHR, recommitted to the JDRF Canada and CIHR Partnership to Defeat Diabetes (established in 2017), investing up to $15 million to be matched by JDRF Canada and its donors for type 1 diabetes research. Budget 2021 also announced $10 million over five years for a new Diabetes Challenge Prize to help surface novel approaches to diabetes prevention and promote the development and testing of new interventions to reduce the risks associated with type 2 diabetes.
Bill C-237, an Act to establish a national framework for diabetes, was introduced by Member of Parliament Sonia Sidhu (Brampton South, Liberal Party of Canada) on February 27, 2020. The Act received unanimous support in both houses of Parliament, and received Royal Assent on June 29, 2021. To advance components and activities prescribed by the Act, all levels of government and key stakeholders from diverse sectors were invited to participate in an engagement process (February to May 2022) to inform the development of the Framework. Organizations and individuals, including populations at elevated risk for developing diabetes, people living with diabetes and their caregivers, Indigenous groups, non-governmental organizations, health care professionals, researchers, and governments, were offered the opportunity to share their views on diabetes through various mechanisms (see Appendix B for details on the engagement process). Common challenges raised by provincial and territorial governments, stakeholders, and opportunities for moving forward, are outlined throughout the Framework.
A broad range of existing frameworks, strategies, and best practices related to the prevention, management and treatment of chronic diseases, including diabetes, have been considered in the development of this Framework. Some examples of these initiatives can be found in Appendix D, which covers initiatives at various levels, including those endorsed by Ministers of federal, provincial and territorial governments in Canada, those led by the Government of Canada, and other related international initiatives. Many other important initiatives developed by provincial and territorial governments, organizations and stakeholders across the country have also been considered in the development of the Framework.
Indigenous Peoples
The Indigenous populations in Canada are diverse and composed of individuals of First Nations, Inuit and Métis heritage. A range of socio-cultural, biological and environmental factors, have contributed to increased rates of diabetes and its complications among Indigenous Peoples in Canada.Footnote 3 Further, the legacy of colonial policies and practices have also contributed to inequities experienced by Indigenous Peoples, as well as systemic racism, intergenerational traumas, disruption of cultural identity and self-determination, and restricted access to resources.
The self-reported rate of diabetes among First Nations adults living off reserve and Métis adults is, respectively, 1.9 and 1.5 times that of non-Indigenous adults.Footnote 3
The self-reported age-standardized rate for diabetes in Inuit was 4.7%.Footnote 23
As a result of these factors, not only is the prevalence of diabetes particularly high in Indigenous communities, but cases of diabetes in Indigenous communities are often more severe than those in the general population.Footnote 16 A Canadian prospective national surveillance study found that from 2006–2008, the incidence of childhood-onset type 2 diabetes in Canada (per 100,000 per year) was 23.2 among Indigenous Peoples, 7.7 in Asian, 1.9 in African/Caribbean and 0.54 in Caucasian.Footnote 17 In addition, the prevalence of diabetes varies between and within each distinction (i.e., First Nations, Inuit and Métis), as communities have unique characteristics and experiences within the interplay of socio-cultural, biological, and environmental factors.
Indigenous Peoples and organizations were included in the broad engagement process designed to support this Framework. However, to address the unique needs and circumstances of diverse Indigenous communities, and to allow sufficient time for meaningful and ongoing engagement, a national Indigenous-led engagement process is being undertaken with Indigenous Peoples, communities, and organizations. This more extensive engagement approach will aim to capture the unique interests, circumstances and perspectives of First Nations, Inuit and Métis, while recognizing the principles of reconciliation and the right to self-determination.
International
The significant and widespread impacts of diabetes have been acknowledged at the global level. The World Health Organization (WHO) has identified diabetes as one of the major public health problems of the 21st century. The 2030 Agenda for Sustainable Development includes a target to reduce by one-third premature mortality from chronic diseases. In 2018, the United Nations General Assembly convened a high level meeting on Non-communicable Diseases (NCDs) to scale up action to achieve this target.
In 2013, the 66th World Health Assembly endorsed the WHO Global Action Plan for the Prevention and Control of NCDs (2013-2020) to strengthen efforts to address the global burden of NCDs. In 2021, the 74th WHA adopted a landmark resolution to reduce the burden of NCDs through strengthening the prevention and control of diabetes. The 75th World Health Assembly in 2022 adopted a resolution to strengthen and monitor diabetes responses within national non-communicable disease programs, including supporting the creation of global voluntary targets for addressing diabetes.
In April 2021, the Government of Canada and WHO co-hosted the Global Diabetes Summit to commemorate the 100-year anniversary of the discovery of insulin and bring high-level political attention to the public health burden of diabetes.
Framework: An approach to address diabetes in Canada
Purpose
The purpose of the Framework is to provide a common policy direction for multi-sectoral stakeholders to improve access to diabetes prevention and treatment to ensure better health outcomes for people living in Canada, and allow for the identification of gaps in current approaches, avoid duplication of effort, and provide an opportunity to monitor and report on progress.
Scope
The Framework lays the foundation for collaborative and complementary action to be taken by all sectors to reduce the impact of diabetes in Canada. The Framework was derived from and builds on what was heard from people in Canada during the engagement process on diabetes.
Cross-cutting principles
Several cross-cutting principles have been identified that are foundational in addressing the components of the Framework. The cross-cutting principles emphasize the importance of: addressing health equity; applying a person-centred approach; differentiating between types of diabetes; supporting innovation; as well as promoting leadership, collaboration and information exchange.
Addressing health equity
The risk for type 2 diabetes across Canada is influenced by social determinants of health, including income, education level, employment and working conditions, food security, early childhood development, social support and connectedness, the built environment, as well as access to the internet, diabetes supports, prevention, and care services.
In addition, the complex interactions between genetic, environmental, cultural and behavioural factors, and the social determinants of health result in inequities in the burden of type 2 diabetes for several population groups in Canada. The relationships between diabetes risk and social and economic exclusion are increasingly recognized as key to understanding and responding to the high prevalence of diabetes in Canada. These social inequities influence opportunities and access to healthy foods and physical activity. They also affect individuals' ability to effectively manage diabetes, with implications for disease progression, and mortality risk. To reduce the health impact of diabetes in Canada, it is critical to deliver the most effective interventions, tailored to the needs of people at greatest risk.
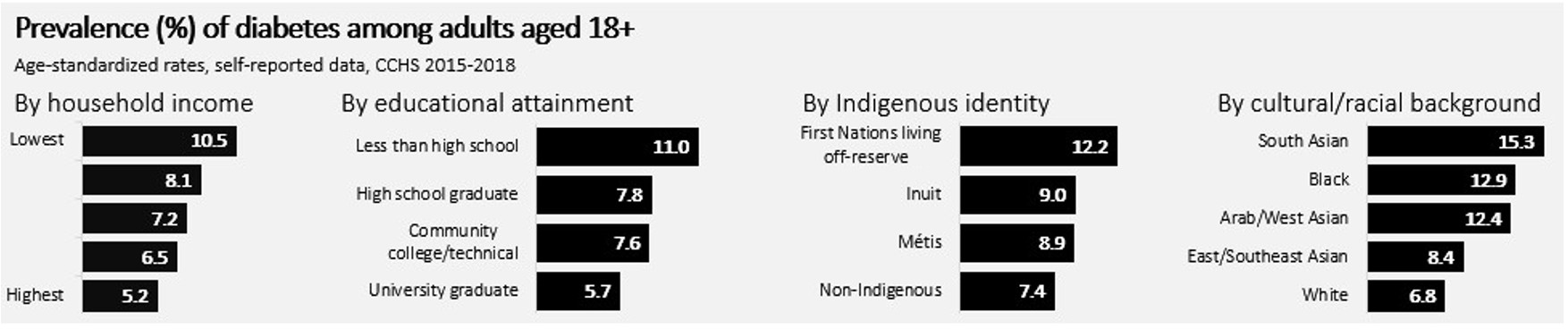
Figure 1 - Text description
Prevalence (%) of diabetes among adults aged 18+
Age-standardized rates, self-reported data, CCHS 2015-2018
By household income
Lowest: 10.5%
- 8.1%
- 7.2%
- 6.5%
Highest: 5.2%
By educational attainment
Less than high school: 11.0%
High school graduate: 7.8%
Community college/technical: 7.6%
University graduate: 5.7%
By Indigenous identity
First Nations living off-reserve: 12.2%
Inuit: 9.0%
Métis: 8.9%
Non-Indigenous: 7.4%
By cultural/racial background
South Asian: 15.3%
Black: 12.9%
Arab/West Asian: 12.4%
East/Southeast Asian: 8.4%
White: 6.8%
Applying a person-centred approach
This approach places people at the heart of activities, services and care to advance progress on diabetes and tailor activities to their needs by considering the influence of and access to physical and social environments on health outcomes. Person-centred approaches can help shift new and existing policies, programs, and operations to focus on what matters most to individuals, families and caregivers and to help them feel dignity and respect along the way.
Differentiating between types of diabetes
It is important to differentiate between the different types of diabetes as each type may differ with respect to its potential causes, prognosis, and treatment. While stigma affects people with different types of diabetes, the sources and impacts of stigma may differ as well. Effective type 2 diabetes prevention, and the management and care of all types of diabetes requires a well-organized system of programs and services that consider the intersections of both medical (e.g., mental health, other chronic or health conditions), biological (e.g., age, genetic predisposition) and social characteristics (e.g., race, immigration or refugee status, living situation) that are designed for and responsive to specific types of diabetes.
Supporting innovation
New perspectives, models, and ways of working are needed to make meaningful progress in the prevention and management of diabetes. This involves looking at things differently, in order to tackle persistent and complex social issues where results have been limited or have not previously been attempted.
Promoting leadership, collaboration and information exchange
Health is a shared responsibility. Real change requires collaborative action by all levels of government, sectors, partners and the public to better coordinate efforts to reduce the risk of and manage all types of diabetes. Combining competencies and pooling resources and networks will help increase information sharing and the development of innovative, effective and sustainable solutions (please refer to Appendix C for jurisdictional roles in diabetes).
Framework components
The Framework is comprised of six interdependent and interconnected components that represent the range of areas where opportunities to advance efforts on diabetes could be beneficial. The components include the following: prevention; management, treatment and care; research; surveillance and data collection; learning and knowledge sharing; as well as access to diabetes devices, medicines, and financial supports.
Prevention
Background
A variety of intersecting social, economic, environmental, genetic and lifestyle factors influence the development of type 2 diabetes. These include factors such as age, physical activity levels, eating habits, access to and affordability of nutritious foods, obesity, ethnicity, family history of diabetes, community design and the built and food environment. Currently, there is no known way to prevent or reduce the risk of type 1 diabetes. However, known risk factors include genetic predisposition and certain environmental triggers. In addition, the onset of type 1 diabetes can often occur quite rapidly, and preventing or delaying complications is important.
Type 2 diabetes develops more gradually, as there is typically a slow increase of high blood sugar.Footnote 4 In some cases, it can take years before glycemic levels are sufficiently high to present symptoms.Footnote 15 Because of this, complications of type 2 diabetes can begin to develop before individuals are diagnosed, or when diagnosed with prediabetes. However, many cases of type 2 diabetes can be prevented or delayed, highlighting the importance of supporting a healthy lifestyle, reducing the risks of developing type 2 diabetes and promoting screening and early detection.Footnote 18
The risk of developing gestational diabetes is associated with many of the same factors as those for type 2 diabetes. Gestational diabetes occurs in pregnant persons if high blood sugar levels develop during pregnancy. Although gestational diabetes usually disappears after the delivery, it increases the risk of developing type 2 diabetes later in life. Breastfeeding has been shown to have a protective effect against diabetes for postpartum mothers and may be protective against obesity for both the infant and mother.Footnote 19 Footnote 20 Maintaining a healthy weight, prior to and during pregnancy, can reduce the risk or developing gestational diabetes.
Prediabetes, type 2 diabetes and gestational diabetes can be determinants of other serious health conditions, and share preventable risk factors with other chronic diseases. The underlying social and environmental conditions that influence diabetes risk have roots in other sectors beyond health, such as industry, recreation, transportation and municipal planning. This highlights the importance of collaboration and multi-sectoral partnerships to address upstream determinants of health to reduce risks for chronic diseases, including diabetes.
Challenges
There are many broad upstream determinants of health that influence eating behaviours and physical activity levels, such as income and education level, employment and working conditions, neighbourhood characteristics and early childhood development. These contribute to a person's risk of developing chronic diseases, including type 2 diabetes, and are not always easily modifiable. Systemic and structural inequities, such as poverty, food insecurity, racism and ableism, lead to socioeconomic and environmental barriers to the accessibility of and participation in prevention behaviours and measures. They stem from many sources, including from regional and urban planning decisions, costs to enroll in programs and services, the presence of comorbidities and the predisposition to other conditions including obesity, social determinants of health (e.g., food and housing insecurities and internet access).
During the stakeholder engagement process, people living with diabetes acknowledged the importance of prevention for type 2 diabetes, but noted that it is harmful to generalize "prevention" to all types of diabetes. In particular, when prevention practices and programs do not address social determinants of health and health equity considerations, and are not relevant to type 1 diabetes.
Opportunities
- Foster collaborative leadership between all levels of government and sectors to address inequities in social determinants of health and promote awareness of and access to social and physical environments that are more supportive of physical activity and healthy eating practices in community and school settings (embedding a "health-in-all-policies" approach).
- Build on the success of the Canadian Diabetes Prevention Program, a 12-month lifestyle intervention program funded through PHAC's Healthy Canadians and Communities Fund, by developing or scaling up evidence- and community-based prevention and health promotion interventions that are tailored to populations at higher risk of chronic diseases and address systemic inequities on a policy and program level.
- Develop new and flexible funding models that utilize sustainable and effective prevention and intervention programs to address national-level data gaps and research, and support a learning system approach (e.g., scale up proven or promising interventions).
- Increase public awareness of type 2 diabetes risk factors, the relationship of obesity to type 2 and gestational diabetes, and its contribution to the severity and complexity of diabetes to help to reduce stigma.
- Promote, support and widely utilize validated preventative measures (e.g., screening tools to determine diabetes risk).
Management, treatment and care
Background
While diabetes management, treatment and care practices vary depending on the type of diabetes, the common goal is to eliminate symptoms and reduce risks for uncontrolled glycemic levels, and prevent or delay the progression of complications through early detection and care. Optimal self-management and care for diabetes and related complications relies on services and supports from many health professionals, specialists and providers, including doctors, nurses, pharmacists, dietitians, diabetes educators in varying settings, as well as access to nutritious foods and physical activity opportunities, diabetes therapies (including devices and drugs) and self-management.
Stigma (e.g., feelings of shame and self-blame), depression or anxiety can be experienced by those affected by diabetes at the point of diabetes diagnosis or throughout the ongoing self-management of the condition. Persons affected by diabetes may also find themselves overwhelmed with the physical and economic demands of managing their condition. Among those affected by type 1 diabetes, the transition from pediatric to adult-based health care can increase stress and anxiety for themselves and their caregivers. This highlights the importance of person-centred care, which was also raised in the Framework engagement process, as people living with diabetes must be treated with compassion and their experiences must be acknowledged at the forefront of health care delivery.
Despite multi-faceted efforts to manage diabetes, the disease can lead to a variety of short-term and long-term complications, requiring varying types of care. In both type 1 and type 2 diabetes, long term complications may include (but are not limited to) heart disease, sight loss or impairments, complications with pregnancy, increased risk of infection, oral health issues, delayed wound healing, and chronic kidney disease. Proper management and care and screening for complications are important to avoid or delay related health complications for all types of diabetes. Further, changes in diabetes medications and lifestyle behaviours may help some individuals with type 2 diabetes to maintain their blood sugar within the recommended target range.
Challenges
Diabetes is a complex condition that requires the individual or caregiver to play a lead role in their care through daily self-monitoring and management of their condition. Diabetes management, treatment and care involve a complex system of many health professionals and partners with different expertise (e.g., health care delivery, education sector, community supports) that often work in silos. The COVID-19 pandemic highlighted the fragmentation in care systems, as well as other long-standing challenges in Canada's health system, including workforce capacity, staffing shortages and limited or reduced access to programs, services and resources.Footnote 14 These factors have resulted in delayed disease screenings, diagnoses and treatments. This can lead to reduced quality of care that is tailored to the needs of patients with different types of diabetes, comorbidities, disabilities, complications or other complex health needs.
To achieve a person-centred approach, stakeholders emphasized that they want to be provided with the tools, education, support and resources necessary to empower them in the management of their own care and as leaders and partners in collaborative community-led efforts. Stakeholders also called for more flexibility and humanity in support systems and care, as well as more inclusion, consultation, understanding and compassion.
Communities facing marginalization and stigmatization may experience additional barriers to care related to prior experiences of bias, racism and discrimination from health professionals and within health systems (e.g., discriminatory policies), as well as cultural and language differences. In addition, there may be a lack of culturally appropriate education, resources and services to improve the support for self-management and decision making. Negative social stigma and a lack of understanding about diabetes and its complications may affect an individual's ability to self-manage their disease in different settings, such as a place of employment, in a school setting or in public facilities. The social, physical and economic stresses associated with diabetes management and its complications can also affect the quality of life and overall health of an individual, their caregivers and those of family members, reinforcing the need for care supports.
Opportunities
- Build capacity for diabetes care in different community contexts, including rural and remote communities, and increase collaboration between interdisciplinary teams of professionals, specialists and services.
- Enhance access to virtual care and support options (e.g., care provider visits, virtual management tools, peer support) with diverse teams that focus on all aspects of diabetes (e.g., prevention, risk reduction, management, treatment, care).
- Explore options to enhance specialized patient-centred training (e.g., cultural considerations, anti-racism, overcoming bias or stigma) for medical professionals to properly identify and manage diabetes and related complications in their patients.
- Increase public awareness, understanding of and access to culturally relevant diabetes content, such as the different types of diabetes, symptoms, signs, risk factors, effective self-management practices and preventative steps.
Research
Background
Canada is home to internationally recognized diabetes researchers, building on the legacy of the Canadian discovery of insulin that occurred 100 years ago. Canadian researchers have contributed to tremendous advances in approaches to diabetes prevention and treatment.
Addressing diabetes, including its prevention, management and care or finding a cure, requires interdisciplinary approaches and collaboration between researchers, scientists, the health product industry, health professionals, community groups and individuals with lived experience to integrate knowledge and skills into research and innovation efforts to inform practice and improve health outcomes.
Research activities can generate new therapies, evidence about how to improve care and information to better understand diabetes pathology, and support policy and programs at many levels and for different audiences, including care providers and individuals living with diabetes.
Important diabetes research activities are underway, including biomedical research (e.g., to understand mechanisms of disease and to develop new treatments), clinical research (e.g., randomized controlled trials to test new therapies), health services and policy research (e.g., to understand and develop effective interventions to prevent diabetes), and population health research (e.g., to understand how the built environment influences risk factors for diabetes). Research on diabetes can take place at varying levels, including globally, nationally, provincially/territorially, or municipally, and is situated in diverse settings across all sectors. Varying mechanisms exist for funding and supporting research, as well as systems employed to collect, share and use data.
The Government of Canada collaborates with many partners and invests in health research to advance the prevention, diagnosis, and treatment of all forms of diabetes. For example, CIHR and JDRF Canada announced the CIHR-JDRF Partnership to Defeat Diabetes in 2017 to jointly fund a total of $30 million in type 1 diabetes research. This partnership was renewed in 2021 with an additional investment of $15 million from Budget 2021, to be matched by JDRF Canada and its donors for type 1 diabetes research.
Innovation in research is also important to support the strengthening of interventions and their evaluation, and to determine the needs of individuals, particularly priority populations, and the effectiveness of diagnostic tools and devices, and quality improvement. Through the use of new technologies, researchers are working to understand the underlying mechanisms of diabetes and its complications, different subtypes of diabetes, and how to optimize or personalize treatments. Research is imperative to improving our understanding of diabetes, its causes and the impacts of disease progression to better tailor clinical care and improve outcomes for patients.
Challenges
Despite tremendous advances in research in Canada, funding for diabetes research and for translation of new discoveries into therapies is limited in Canada. This has been documented in previous reports.Footnote 21
Stakeholder engagement highlighted that traditional research processes may not be people or patient-centred, and may not include meaningful patient or caregiver engagement throughout the research process. In addition, ethics and privacy concerns were raised. Further, some diabetes research lacks indicators to measure progress, as well as appropriate sociocultural measurements of outcomes in marginalized communities.
Increased emphasis on research that addresses new and emerging priorities in diabetes is needed, including the relationship between diabetes and other conditions, such as COVID-19, improving our understanding of the impacts of social determinants on chronic diseases, or the impacts of being diagnosed earlier and living longer with diabetes. Research innovation and capacity of users to access, analyze and use data is often an issue across and within jurisdictions. In addition, duplication and fragmentation challenges for diabetes research can limit the translation of research into evidence-informed practice, which affects opportunities for learning and knowledge exchange.
Opportunities
- Enhance investments for innovative diabetes research for all types of diabetes in Canada to support strong investigator-initiated and strategic research.
- Build stronger connections between researchers, practitioners, industry, policy-makers and people with lived experience to establish research priorities on diabetes in order to pool resources, drive innovation, and achieve common goals to advance diabetes research.
- Build on the success of the Strategy for Patient-Oriented Research (SPOR) by advancing research activities which are inclusive of persons with diabetes and related complications, and ensuring that research instruments are accessible (e.g., multiple accessible formats, multiple ways to participate).
- Enhance research with innovation and health equity considerations by targeting intervention research on the social determinants of health that are root causes of inequities.
- Identify effective interventions to prevent prediabetes, gestational and type 2 diabetes in order to provide an evidence base for families, community leaders, and decision makers.
Surveillance and data collection
Background
Surveillance is the ongoing, systematic collection, analysis and interpretation of population data, and the timely dissemination of this information to decision-makers. Population data include aggregated individual data (health status, use of health services, quality of life, risk factors and health determinants) and community data (environment, policies, programs and services). High quality surveillance data is used for planning and evaluating policies, community programs, clinical services, education programs and research. In Canada, surveillance is a shared responsibility, and each federal, provincial and territorial, regional/local, and Indigenous jurisdiction needs data on its own population, at its own level.
The surveillance of diabetes at the national level is well established through the Canadian Chronic Disease Surveillance System (CCDSS), a collaborative network of provincial and territorial surveillance systems supported by PHAC. The system collects data on all residents who are eligible for provincial or territorial health insurance. It generates national estimates and trends over time for over 20 chronic diseases and conditions, including diabetes mellitus (which encompasses all types of diabetes except for gestational diabetes), and other selected health outcomes.
The Government of Canada, through PHAC, works with provinces and territories to improve the way information is shared across jurisdictions to allow for effective collection, analysis and sharing of relevant information. In addition to helping public health officials provide their best advice in public health emergencies such as the COVID-19 pandemic, reliable, timely and relevant public health data will lead to improvements in health outcomes for those living in Canada in the longer term. Led by PHAC, in collaboration with provinces and territories, the Pan-Canadian Health Data Strategy is being created to help improve health data collection, access, sharing and use.
Challenges
Important gaps exist in the collection, linking and sharing of health data, which includes public health, health system and population health data. Currently there is an inability to differentiate between the types of diabetes, associated complications, comorbidities, outcomes or measures of diabetes control and to link health data to sociodemographic information and other important determinants (e.g., Indigeneity, race, income, age, employment, housing) at a national level. These components are critical to identifying the needs and disparities among communities facing marginalization, setting priorities for action, and assessing programmatic progress, while respecting Canadians' rights to privacy and confidentiality of information.
Surveillance systems, practices, standards, policies and legislation vary significantly from one region to another in Canada. For example, irregular data collection of dietary intakes and nutrition related indicators, including across diverse populations, limit our understanding of the impact of nutrition on diabetes. Innovation in surveillance systems is required to reduce fragmentation, streamline data collection and improve its timeliness. Evidence is needed to support people living with diabetes and their caregivers, including monitoring varying costs, access to care, treatments and medical devices, while respecting privacy of information.
Opportunities
- Explore options to enhance national diabetes surveillance to establish a comprehensive system that allows for differentiation by types of diabetes, and include (where possible) demographic information to identify priority populations at an elevated risk of diabetes.
- Leverage multi-sectoral partnerships to scale up and expand current data sharing and sources, and create new data linkages to enhance the surveillance of diabetes, and report on more diabetes-related indicators (e.g., types, risk factors, complications, comorbidities, management).
- Ensure that data collection activities include health equity considerations (e.g., inclusive of persons with disabilities and from various racialized communities), data collection instruments are accessible (e.g., multiple accessible formats), and respectful, non-stigmatizing patient-centric language is used for people living with diabetes.
Learning and knowledge sharing
Background
There are many health care providers involved in diabetes care. Learning and knowledge sharing among all providers is important, as care for all types of diabetes can occur in many different settings, such as local pharmacies, specialized children's hospitals or nursing stations in a remote community, for example. Tailoring communication to communities is also important to ensure that information is accessible and relevant to intended audiences.Footnote 22
Clinical practice guidelines, which are comprehensive and evidence-based, have been established for use by health care providers to guide prevention efforts and treatment practices, as well as to reduce the burden of diabetes complications in Canada. Many organizations in Canada provide clinical practice guidelines related to health promotion and chronic disease prevention and management, including diabetes-specific guidelines. This information, as well as other evidence-based tools and resources and knowledge translation products are accessible online and through portals such as the National Collaborating Centres for Public Health.
Providing effective diabetes prevention, risk reduction, management and treatment information and services depends on knowledgeable, skilled health care providers. Community and health service providers require a wide variety of skills, such as effective communication, community development, collaborative practice, advocacy, social marketing, planning and evaluation, management and research synthesis. Building human resource capacity involves many approaches, including initial training for health care providers, allied health workers and volunteers; effective recruitment and retention strategies; and ongoing training and education to update essential skills. In addition, an effective mechanism for knowledge synthesis and exchange is needed, as knowledge and skills requirements change constantly in response to new research findings.
While the COVID-19 pandemic created additional health care system pressures, it improved collaboration and knowledge sharing between all levels of government, the private sector, health associations, organizations and communities. It also led to increased mobilization of human resources with specialized skills and allied health professionals to support complex and ongoing health priorities, and to provide culturally adapted materials and resources. Pandemic response efforts made important gains to increase access to health care services and supports, particularly for remote communities, and Indigenous Peoples in the provision of virtual and tele-health services.Footnote 22 Although some services may be more readily available since COVID-19, access to health care continues to be an ongoing issue in remote and northern communities.
Challenges
The pandemic demonstrated that increased reliance on digital health care for diabetes management, and general support and learning to improve health can expand reach and have a positive impact. However, limitations in digital literacy and lack of reliable internet access in northern, rural and remote communities can pose challenges in accessing virtual services.
Participants in the Framework engagement process noted the need for current, accurate, reliable and timely messaging on diabetes. This was particularly evident during the COVID-19 pandemic. Further, given the strain placed on available health resources as a result of the pandemic, stakeholders stressed the importance of ensuring information is easily accessible and available in multiple formats.
Stakeholders also highlighted the need to make clinical practice guidelines more relevant and accessible for both professionals and patients. Concerns were also raised about gaps that exist between recommended care outlined in diabetes guidelines, and actual practice, including the type of care required and enhanced clinical decision-making tools for primary care providers. In addition, clinical practice guidelines are expensive and time-consuming to develop and update, as the evidence is always evolving. In order to increase efforts to address chronic disease within communities, the capacity to provide these services must also be increased.
Opportunities
- Expand technologies and digital solutions (e.g., social media, digital tools or knowledge hub platforms) to provide equitable, educational and accessible resources that increase diabetes awareness, understanding and knowledge sharing.
- Promote collaborative efforts among health professionals to identify, develop and share best practices, align messaging and coordinate knowledge mobilization, particularly for treating priority populations living with diabetes in various stages in life (e.g., transition from youth to adulthood, as noted in Diabetes 360°: A Framework for a Diabetes Strategy for Canada).
- Facilitate regular updating of clinical practice guidelines to ensure that the most recent research evidence to improve care for people living with all types of diabetes is being integrated.
- Ensure that centralized and culturally appropriate educational materials and evidence-informed approaches can be adapted and are accessible at the community level to reach all persons with diabetes, particularly those with disabilities and priority populations.
Access to diabetes devices, medicines, and financial supports
Background
The development, research, innovation, approval and delivery of medical devices in Canada involves many actors, including governments, insurance and pharmaceutical companies, healthcare professionals, researchers, and other stakeholders. Each has a role in ensuring that Canadians have access to the innovative and appropriate treatments they need. Regulatory processes, health insurance and health systems all affect access to new and existing drugs and devices. Provincial and territorial programs and public drug plans provide coverage for certain diabetes-related medications, supplies and equipment and medical devices.
At the federal level, there are a number of key responsibilities and supports. Health Canada is responsible for the safety and effectiveness of new treatments, diagnostic and self-management technologies and prevention tools through the approval of drugs and devices in Canada. This includes devices used to monitor, control and maintain blood sugar levels, such as insulin pumps or insulin injections using a syringe or pen. Indigenous Services Canada implements the Non-Insured Health Benefits Program that provides registered First Nations and recognized Inuit coverage for a range of health benefits not covered through social programs, private insurance plans or provincial/territorial health insurance.
The Disability Tax Credit (DTC), administered by the Canada Revenue Agency (CRA), provides greater tax equity by recognizing the costs of disability. People living with diabetes who meet eligibility criteria may receive a non-refundable income tax credit. The Medical Expense Tax Credit also provides some tax relief for out-of-pocket costs related to managing diabetes, such as medication, medical devices and supplies, and travel costs for medical appointments. Several other credits and benefits are also available to provide income supports for individuals facing physical and mental health impairments.
Manufacturers of medical devices are responsible for developing and testing their devices. This includes the development of innovative safety features for medical devices that meet the specific needs of specific user groups, such as persons with diabetes who have experienced sight loss.
Stakeholders have emphasized that people living with diabetes need access to devices and medications that best meet their needs in order to effectively manage their own care. Specifically, a number of stakeholders noted the limitations of the DTC, notably the burden of completing benefit-related forms and have asked for simplified eligibility criteria aligned with the 2021 HESA report recommendations related to the DTC, the 2019 CRA Disability Advisory Committee's Annual Report, and the 2018 Report by the Standing Senate Committee on Science, Social Affairs and Technology entitled, Breaking Down Barriers: A Critical Analysis of the Disability Tax Credit and the Registered Disability Savings Plan (RDSP). The Government of Canada has addressed these recommendations through Budget 2019 and Budget 2021 investments, which include several changes to the RDSP and to the life-sustaining therapy rules for qualifying for the DTC. In addition, the recently enacted Budget Implementation Act, 2022 also includes amendments that deem persons with type 1 diabetes to have met the time-related criteria for qualifying for the DTC for life-sustaining therapy.
Challenges
Many Canadians with diabetes continue to face barriers and challenges in accessing necessary treatments and supports due to various obstacles, including lack of transportation, lack of financial coverage for treatments and devices, language barriers, unreliable internet access, varying quality of treatment and care or previous experiences of discrimination by the healthcare system.Footnote 14 Public health measures as a result of COVID-19 further impeded access to treatments and supports through increased wait times and delays for medical appointments, and treatments, reduced hours and closures of medical centres.Footnote 22
In addition to varying regulatory processes for the development, approval and delivery of drugs and medical devices, health insurance coverage, socioeconomic status and health systems practices across jurisdictions, all affect access to devices, medications and services, and can act as barriers to receiving care. For example, while many provinces and territories have diabetes supplies programs, access to and eligibility of drugs and device coverage varies across provinces and territories, widening inequities for people affected by diabetes and other health conditions. In addition, people moving across provinces or territories must navigate different drug coverage and benefit systems.
The cost of diabetes treatment has been rapidly increasing in Canada in recent years. This concern was echoed by stakeholders. While the growing prevalence of the disease is a contributing factor, more expensive treatments have been a major cost driver, especially given the uptake in new, higher-cost drugs.Footnote 24 In addition, people living with diabetes may require access to many different types of medications and treatments, and may use a combination of therapies to manage diabetes, including insulin-releasing devices to maintain blood sugar levels, or medical equipment required as a result of diabetes related complications, such as eye glasses for vision loss or prosthetics and assistive devices for limb impairments.
While manufacturers and researchers continue to innovate to develop new products and enhance the features of existing medical devices, there are not many authorized diabetes medical devices which have been optimized to include accessible options for use by persons with disabilities. For example, those affected by diabetes complications, such as vision impairments or limb loss, may have difficulty using or cleaning certain devices, or may require assistance, affecting their ability to self-manage their condition. In addition, people living with disabilities, including diabetes, often require more financial assistance for under or unfunded disability supports.
Opportunities
- Explore the need for additional supports to alleviate barriers, such as accessing care, and determine what tools could provide better support for people with diabetes and their care providers.
- Enhance collaboration with industry to encourage innovation in the development of accessible diabetes devices and product designs through meaningful engagement with priority populations.
- Increase information sharing regarding new technologies across federal, provincial and territorial jurisdictions, with a focus on their safety and effectiveness, accessibility for use by people with different abilities, as well as evaluations of costs, improvements and health outcomes.
Moving forward
Informed by key stakeholders, including people affected by diabetes, the Framework serves as a policy guidance document that lays out a common direction to address diabetes in Canada. All sectors and levels of government are invited to use the Framework to address diabetes and advance opportunities in ways that meet their respective mandates and objectives, and that are adapted to their respective community priorities and contexts. An inclusive and broad social determinants of health perspective and person-centred approach must be applied to respectfully and meaningfully move forward in addressing diabetes in Canada.
The release of the Framework for Diabetes in Canada marks an important milestone in efforts to support stakeholders to identify areas for action to address the challenges that diabetes presents, and to help advance activities in their respective communities. However, there is still significant work ahead. Among other aspects, it will require ongoing multi-sectoral collaboration and a curiosity for innovative approaches to support those living with diabetes.
The Government of Canada will continue to advance efforts to support improved access to diabetes prevention and treatment to ensure better health outcomes for Canadians. Further engagement with stakeholders is planned to advance health equity, encourage innovation and build collaborative mechanisms. The Indigenous-led engagement process on diabetes will acknowledge the voices, interests and unique perspectives of Indigenous communities and support their plans to address diabetes in their own communities.
After five years (2027), a progress report identifying federal efforts that are addressing diabetes will be tabled in Parliament by the Minister of Health, as required by the Act. It will note collaborative efforts with provincial, territorial and local governments and with diabetes stakeholders, and report on the current state of diabetes prevention and treatment in Canada.
Appendices
Appendix A: National Framework for Diabetes Act
Visit the Justice Laws website to see the National Framework for Diabetes Act.
Appendix B: Engagement process
The Public Health Agency of Canada, with the assistance of the Morris J. Wosk Centre for Dialogue based at Simon Fraser University, undertook a virtual engagement process to support the Act. A wide range of key stakeholders had an opportunity to share their views, experiences and perspectives to help identify gaps and priorities for advancing efforts on diabetes in Canada, and inform the development of the Framework.
The engagement process was comprised of a series of key informant interviews with key diabetes stakeholders, followed by larger dialogue sessions to identify and discuss challenges related to diabetes, opportunities for collaboration and action, and share ideas for a framework. In addition, an online feedback tool provided an opportunity for stakeholders to voice their perspectives on key themes, and identify gaps and opportunities to help advance diabetes in Canada.
Stakeholder engagement process
Phase 1: February to March 2022
- 32 Key informant interviews conducted with 50 individuals
Phase 2: April 2022
- Two dialogue sessions conducted in English and in French
- 89 key diabetes stakeholders participated
Online feedback tool: April to May 2022
- 884 individuals provided input
- Over 2,000 comments provided
Key stakeholders engaged in the dialogue for diabetes, including (but not limited to):
- representatives of population groups that face health and social inequities (e.g., organizations representing different races, age groups and health conditions, including people living with a disability or experiencing diabetes related complications);
- diabetes device and insulin manufacturers;
- health professionals involved in diabetes prevention and management;
- researchers and academics;
- health charities and organizations with a primary focus on diabetes, or those involved in addressing diabetes indirectly;
- all levels of governments responsible for health and related sectors; and
- people living with diabetes and their caregivers.
To ensure effective coordination of effort and advice, two advisory groups were established to provide input and feedback throughout the engagement process and Framework development:
- an External Advisory Group on Diabetes, comprised of key diabetes-related stakeholders, including individuals affected by diabetes; and
- an Internal Advisory Group on Diabetes, comprised of key federal departments.
PHAC leveraged existing federal, provincial and territorial mechanisms to engage provincial and territorial governments. Further, a broad range of frameworks, strategies and best practices related to the prevention, management and treatment of diabetes were considered in the development of this Framework.
Indigenous organizations were included in the engagement process designed to support this Framework. However, to capture the unique interests, circumstances and perspectives of First Nations, Inuit and Métis Peoples, and recognize the principles of reconciliation and the right to self-determination, a separate and more extensive nation-wide Indigenous-led engagement approach is being undertaken.
The overall approach to stakeholder engagement was designed to ensure that various policy considerations were addressed including sex and gender based analysis plus (SGBA Plus), official languages, and accessibility, equity, diversity and inclusion.
Appendix C: Roles and responsibilities in Canada to address diabetes
All governments and many stakeholders and sectors have a role to play in the prevention, treatment and management of diabetes in Canada. The promotion and protection of health is an area of shared jurisdiction in Canada.
The federal role includes promoting and protecting the health of Canadians, while respecting provincial and territorial areas of jurisdiction. The Government of Canada's responsibilities include:
- the surveillance of chronic diseases in Canada, including diabetes;
- developing policies and guidelines, and supporting implementation through awareness and education;
- delivering and funding healthcare services for Indigenous populations (including First Nations people living on-reserve, and Inuit communities);
- supporting education of federally employed healthcare providers;
- facilitating research and innovation to understand diabetes risk factors and prognosis and supporting the development of new diagnostic and treatment tools;
- administering the financial supports for expenses related to diabetes and other disability-related expenses;
- approving and regulating food labelling and marketing, and the safety and effectiveness of new treatments, diagnostic and self-management technologies and prevention tools through the approval of drugs and devices;
- facilitating community-based interventions; and
- collaborating and engaging with provinces and territories, international partners and other sectors to address diabetes.
Provincial and territorial governments are also responsible for promoting and protecting health within their jurisdictions, including:
- healthcare settings, health insurance, and the delivery of health programs and services;
- establishing policies, guidelines, and standards for healthcare settings;
- supporting medical education; implementing programs for chronic disease prevention;
- supporting research and academic initiatives and collecting data used for surveillance;
- facilitating community-based interventions; and
- establishing certification programs for health service providers.
Indigenous Peoples and organizations identify the health priorities of First Nations, Inuit, and Métis; and develop and implement policies, strategies, programs, and services to address their priorities and needs.
Civil society, including community-based and other non-governmental organizations, activists and allies, and those affected by diabetes and their caregivers, take action to deliver diabetes prevention, education and awareness initiatives; advance the health promotion by contributing to research, collaborating with other actors to share knowledge and implementing initiatives to increase access to testing, treatment and ongoing care and support; and advocating for programs and services for affected individuals and communities.
Health professionals provide front-line care for the detection, treatment, management and support of diabetes and its complications by providing screening and diagnostic tests; prescribing treatments; contributing to surveillance and monitoring; educating individuals on healthy living and diabetes care practices; and implementing prevention initiatives.
Professional associations and licensing bodies establish standards and certification for their professions, prescribing guidelines, awareness and training of health service providers.
The academic sector undertakes research to better understand the types of diabetes and to discover solutions and innovative approaches to prevent, treat, manage and care for individuals affected by diabetes.
Local authorities, including local health authorities, are responsible for providing services or facilities to promote health, delivery of health services and programs, including primary care, acute care, home and community care and surveillance.
The pharmaceutical and medical device industry and the private sector support the development of new prevention, diagnostic and treatment technologies, manufacture drugs and devices; support community action; and provide public and professional education related to these products.
Appendix D: Strategies and frameworks addressing diabetes and chronic diseases
The purpose of this appendix is to provide examples of diabetes related strategies, frameworks and best practices, which have been considered in the development of this Framework. They cover initiatives at various levels, including those endorsed by Ministers of federal, provincial and territorial governments in Canada; led by the Government of Canada; and related international initiatives. It is not meant to be an exhaustive list.
Many other organizations and stakeholders in Canada are leading activities related to chronic diseases, including diabetes, and have developed their own strategies and frameworks. These national, regional or local level organizations include those in both the private and public sectors with varying mandates, missions, scopes and sizes. For example, activities advanced by the provinces, territories and not-for-profit organizations, such as Diabetes Canada's Diabetes 360°: A Framework for a Diabetes Strategy for Canada.
Federal, provincial and territorial (FPT) governments (Endorsed by FPT Ministers)
A Common Vision for Increasing Physical Activity and Reducing Sedentary Living in Canada - Let's Get Moving (2018)
Through a national consultation and engagement process, areas of focus for collaborative action were identified to help guide a collective approach to policies, planning, priorities and programming across Canada, endorsed by FPT Ministers Responsible for Sport, Physical Activity and Recreation.
Creating a Healthier Canada: Making Prevention a Priority (2010)
Through the Declaration on Prevention on Promotion, FPT Ministers of Health endorsed a written, public statement of vision to work together, and with others, to make the promotion of health and the prevention of disease, disability and injury a priority for action.
Curbing Childhood Obesity: A Federal, Provincial and Territorial Framework for Action to Promote Healthy Weights (2010)
This framework marks the first policy initiative endorsed by FPT Ministers of Health offering a common direction for moving forward on three integrated strategies to address childhood obesity.
Integrated Pan-Canadian Healthy Living Strategy (2005)
FPT Ministers of Health endorsed the Pan-Canadian Healthy Living Strategy in 2005, joining other countries around the world that have recognized the fundamental importance of promoting healthy living behaviours through coordinated and sustained action.
Government of Canada
Pan-Canadian Health Data Strategy (in development)
Led by the Government of Canada in collaboration with provinces and territories, the Pan-Canadian Health Data Strategy is being created to help improve health data collection, standardization, and use.
Disability Inclusion Action Plan (in development)
The Disability Inclusion Action Plan aims to improve the social and economic lives of Canadians with disabilities across four pillars: financial security, employment, accessible and inclusive communities, and a modern approach to disabilities. The government is working with stakeholders and experts in the disability community to finalize its release.
Canada's National Active Transportation Strategy (2021)
The National Active Transportation Strategy increases opportunities for Canadians and promotes active transportation and its benefits. The Active Transportation Fund supports the Strategy to help to shift away from cars and toward active transportation.
Wellness Together Canada (2020)
A mental health and substance use portal that provides free physical activity resources and supports to Canadians, including information on maintaining a healthy lifestyle, as well as access to peer support workers, social workers, psychologists and other professionals.
Pan-Canadian Health Inequalities Reporting Initiative (2019)
The aim of this report is to strengthen the measurement, monitoring and reporting of health inequalities in Canada to help inform healthy living programs and policies that target priority population groups.
Canada's Tobacco Strategy (2018)
The key activities in Canada's Tobacco Strategy are supporting improved services and resources to help people quit smoking; funding programs to explore the most effective ways to help Canadians quit smoking; and giving information on and access to less harmful sources of nicotine.
Healthy Eating Strategy (2016)
The Healthy Eating Strategy aims to improve the food environment in Canada to make it easier for Canadians to make the healthier choice by improving healthy eating information, improving nutrition quality of foods, protecting vulnerable populations and supporting increased access to and availability of nutritious foods. Key initiatives include the revised Canada's Food Guide and front-of-pack labelling regulations and restrictions on food marketing to children.
Truth and Reconciliation Commission (TRC) Calls to Action
This final TRC report contains 94 calls to action in areas of promoting healing, education, and listening to redress the legacy of residential schools and advance the process of reconciliation in Canada.
International efforts
WHO Global Action Plan on Physical Activity (2018-2030)
The WHO global action plan aims to help countries scale up policy actions to promote physical activity. It responds to the requests by countries for updated guidance, and a framework of effective and feasible policy actions to increase physical activity at all levels. The plan sets out four objectives and recommends 20 policy actions that are applicable to all countries and address the cultural, environmental and individual determinants of inactivity.
Bangkok Charter for Health Promotion (2016)
The Bangkok Charter identifies actions, commitments and pledges required to address the determinants of health in a globalized world through health promotion. The four key commitments are to make the promotion of health: central to the global development agenda, a core responsibility for all of government, a key focus of communities and civil society, a requirement for good corporate practice.
2030 Agenda for Sustainable Development (2015)
The Sustainable Development Goals are a universal call to action to end poverty, protect the planet and improve the lives and prospects of everyone, everywhere. The 17 Goals were adopted by all UN Member States in 2015, as part of the 2030 Agenda for Sustainable Development which set out a 15-year plan to achieve the Goals.
WHO Global Action Plan on Non-Communicable Diseases (2013-2020)
The plan follows commitments made by Heads of State and Government in the United Nations Political Declaration on the Prevention and Control of NCDs (resolution A/RES/66/2), recognizing the primary role and responsibility of Governments in responding to the challenge of NCDs and the important role of international cooperation to support national efforts.
Rio Political Declaration on Social Determinants of Health (2011)
The declaration expresses global political commitment for the implementation of a social determinants of health approach to reduce health inequities and to achieve other global priorities. It will help to build momentum within countries for the development of dedicated national action plans and strategies.
Ottawa Charter for Health Promotion (1986)
The first International Conference on Health Promotion was held in Ottawa in November 1986. The intent of the Charter was to achieve Health for All by the year 2000 and beyond. This conference was primarily a response to growing expectations for a new public health movement around the world.
Appendix E: Glossary
For the purposes of this Framework, the following definitions are used:
Allied Health Professionals: A diverse group of clinicians, specialists and health care workers who collaborate to deliver high-quality care to patients across a variety of different settings.
Age-standardized: Rates are adjusted for changes in the age structure of the population over time, or for differences in age structure across different populations (for example, by provinces, territories, or ethnicity).
Asymptomatic: When an individual has a disease or condition but does not experience or present with any symptoms.
Body mass index (BMI): A measure of human body size and proportion. It is defined as the weight in kilograms divided by the square of height in meters (see Obesity). Various levels of BMI are used as guidelines for healthy targets.
Cardiovascular (heart) disease: All diseases of the circulatory system including congenital and acquired diseases such as acute myocardial infarction (heart attack), ischemic heart disease, valvular heart disease, peripheral vascular disease, arrhythmias, hypertension, and stroke.
Canadian Chronic Disease Surveillance System (CCDSS): A national surveillance system that uses population-based administrative data from provinces and territories to provide comparative information for assessing the scope, use of health services and health outcomes of chronic diseases in Canada.
Co-morbidity: When two disorders or illnesses occur in the same person, simultaneously or sequentially, they are described as co-morbid. Co-morbidity also implies interactions between the illnesses that affect the course and prognosis of both.
Diabetes: A chronic disease that occurs when the body is unable to sufficiently produce or properly use insulin. Diabetes mellitus occurs in several forms – type 1, type 2 and gestational are the most common. Other uncommon types of diabetes can be caused by other diseases or medications.
Ethnicity: Ethnicity is a multi-dimensional concept referring to community belonging and a shared cultural group membership. It is related to socio-demographic characteristics, including language, religion, geographic origin, nationality, cultural traditions, ancestry, and migration history, among others.
Gestational diabetes: Occurs when elevated blood sugar levels develop during pregnancy, but normally ends following childbirth.
Health equity: The absence of unjust, systemic, and avoidable inequalities in health status or the distribution of health resources among sub-populations defined socially, economically or geographically.
Health inequities: The subset of health inequalities that are deemed to be unfair or unjust, that arise from the systematic and intentional or unintentional marginalization of certain groups, and that are likely to reinforce or exacerbate disadvantage and vulnerability.
Health inequalities: The differences in health status or in the distribution of health determinants between different population groups. These differences can be due to biological factors, or individual choices. Many differences can be attributed to the unequal distribution of the social and economic factors that influence health (e.g., income, education, employment, social supports) and exposure to societal conditions and environments largely beyond the control of the individuals concerned.
Health in all policies (HiAP): A collaborative approach that systematically considers health implications in policymaking across sectors to minimize social and health-related harms. This approach aims to improve the health of all communities and people by recognizing that many drivers for health outcomes are beyond the health sector.
Health literacy: A person's ability to find, understand and use written information to promote, maintain and improve their health.
Hyperglycemia: Elevated blood sugar levels.
Hypoglycemia: Low blood sugar levels.
Indigenous: "Indigenous Peoples" is a collective name for the original Peoples of North America and their descendants. "Aboriginal Peoples" was formerly used. The Canadian Constitution recognizes three groups of Aboriginal Peoples: First Nations, Inuit and Métis. These are three distinct Peoples with unique histories, languages, cultural practices and spiritual beliefs.
Incidence: The number of newly diagnosed cases during a given period in a specified population.
Insulin: A hormone secreted by beta cells in the pancreas that enables the cells of the body to absorb sugar from the bloodstream and use it as an energy source.
Morbidity: Any departure, subjective or objective, from a state of physiological or psychological wellbeing.
Mortality rate: An estimate of the proportion of a population that dies during a specified period.
Obesity: A relative term for excessive accumulation of fat in the body; defined in several ways. A common reference is the World Health Organization definition: individuals are considered obese if they have a Body Mass Index (BMI) equal to or greater than 30 kg/m2.
Overweight: Individuals are considered overweight if they have a Body Mass Index (BMI) equal to or greater than 25 kg/m2.
Person-centred approach: An approach where the person is placed at the centre of services and treatment, and activities are coordinated and tailored to the needs of the individual.
Physical inactivity: An insufficient physical activity level to meet present physical activity recommendations. General definition applies to all age and ability groups.
Prediabetes: A state in which affected persons have fasting blood sugar levels or a response to a fasting glucose tolerance test that is higher than normal, but not high enough for a diagnosis of diabetes.
Prevalence: The number of individuals affected by a disease or a risk factor at a given point in time.
Prevalence rate: The proportion of individuals that are affected by a disease or a risk factor at a given point in time.
Priority populations: For the purposes of this Framework, priority populations refers to sub-populations in Canada at higher risk for developing diabetes or of experiencing challenges with the management of diabetes due in part to genetic, environmental, cultural and behavioural factors, including marginalization, and inequities in social determinants of health. These include people of certain ethnic backgrounds including people of African, Arab, Asian, Hispanic, and Indigenous and South Asian descent.
Race (or racial group): A social construct used to judge and categorize people based on perceived differences in physical appearance in ways that create and maintain power differentials within social hierarchies.
Self-management: Diabetes self-management refers to the activities and behaviours an individual undertakes to control and treat their condition.
Type 1 diabetes: An autoimmune disease in which the body's immune system attacks and destroys the insulin-producing cells of the pancreas.
Type 2 diabetes: A metabolic disorder that occurs when the pancreas does not produce enough insulin and/or when the body does not properly use the insulin it makes.
Uncommon types of diabetes: These include conditions associated with genetic defects, other diseases, infections and specific medications that affect the body's ability to produce or respond to insulin.
Appendix F: Visual of the Framework for diabetes in Canada
Framework for Diabetes in Canada
Purpose: The purpose of the Framework for Diabetes in Canada is to:
- provide a common policy direction for multi-sectoral stakeholders;
- identify gaps in current approaches, avoid duplication of effort, and provide an opportunity to monitor and report on progress.
Scope: The Framework lays the foundation for collaborative and complementary action to be taken by all sectors to reduce the impact of diabetes in Canada.
Desired outcome of the Framework is to improve access to diabetes prevention and treatment to ensure better health outcomes for Canadians.
Cross-cutting principles:
The Framework identifies several cross-cutting principles that should guide efforts to address diabetes in Canada:
- addressing health equity;
- applying a person-centred approach;
- differentiating between types of diabetes;
- supporting innovation; and
- promoting leadership, collaboration and information exchange.
Framework components: The Framework organizes efforts into six separate Framework components:
- prevention
- management, treatment and care
- research
- surveillance and data collection
- learning and knowledge sharing
- access to diabetes devices, medicines and financial supports
References
- Footnote *
-
Although consulted, provincial and territorial government endorsement has not been sought. This Framework, including its appendices, has been prepared by the Public Health Agency of Canada in accordance with the Act, and does not necessarily reflect the views of provinces and territories.
- Footnote 1
-
Public Health Agency of Canada. Diabetes in Canada. Government of Canada, 2017. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/diabetes-canada-highlights-chronic-disease-surveillance-system.html#fn2.
- Footnote 2
-
Public Health Infobase. Canadian Chronic Disease Surveillance System (CCDSS). Public Health Agency of Canada. Available from: https://health-infobase.canada.ca/ccdss/data-tool/Index?G=00&V=1&M=4&Y=2017.
- Footnote 3
-
Public Health Agency of Canada. Key Health Inequalities in Canada: A National Portrait. Government of Canada, 2018. Available from: https://www.canada.ca/en/public-health/services/publications/science-research-data/inequalities-diabetes-infographic.html.
- Footnote 4
-
Public Health Agency of Canada. Diabetes in Canada: Facts and Figures from a Public Health Perspective. Government of Canada; 2012. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/diabetes/diabetes-facts.html.
- Footnote 5
-
Public Health Agency of Canada. Childhood Obesity. Government of Canada, 2016. Available from: https://www.canada.ca/en/public-health/services/childhood-obesity/childhood-obesity.html.
- Footnote 6
-
Imperatore G, Boyle JP, Thompson TJ et al. Projections of Type 1 and Type 2 Diabetes Burden in the U.S. Population Aged <20 Years Through 2050. Diabetes Care. 2012, 35(12): 2515-2520. https://doi.org/10.2337/dc12-0669.
- Footnote 7
-
Dean HJ and Sellers EAC. Children Have Type 2 Diabetes Too: An Historical Perspective. Biochemistry and Cell Biology. 2015, 93(5): 425-429. https://doi.org/10.1139/bcb-2014-0152.
- Footnote 8
-
Wicklow B, Dart A, McKee J, et al. Experiences of First Nations Adolescents Living with Type 2 Diabetes: A Focus Group Study. CMAJ. 2021, 193(12): E40-E409. https://doi.org/10.1503/cmaj.201685.
- Footnote 9
-
Schabert J, Browne JL, Mosely K, Speight J. Social Stigma in Diabetes : A Framework to Understand a Growing Problem for an Increasing Epidemic. Patient. 2013, 6(1):1-10. doi: 10.1007/s40271-012-0001-0. PMID: 23322536.
- Footnote 10
-
Liu NF, Brown AS, Folias AE, Younge MF, Guzman SJ, Close KL, Wood R. Stigma in People With Type 1 or Type 2 Diabetes. Clin Diabetes. 2017, 35(1):27-34. doi: 10.2337/cd16-0020.
- Footnote 11
-
Public Health Agency of Canada. The Chief Public Health Officer's Report on the State of Public Health in Canada 2019 - Addressing Stigma: Towards a More Inclusive Health System. Government of Canada, 2019. Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/addressing-stigma-toward-more-inclusive-health-system.html.
- Footnote 12
-
Public Health Agency of Canada. Your Guide to Diabetes. Government of Canada, 2014. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/reports-publications/diabetes/your-guide-diabetes.html.
- Footnote 13
-
Public Health Agency of Canada. Government of Canada. COVID-19: Who Is At Risk of More Severe Disease or Outcomes. Government of Canada, 2022. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/people-high-risk-for-severe-illness-covid-19.html.
- Footnote 14
-
Public Health Agency of Canada. Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2020. From Risk to Resilience: An Equity Approach to COVID-19. Government of Canada, 2020. Available from: https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19.html.
- Footnote 15
-
Public Health Agency of Canada. Diabetes in Canada: Facts and Figures from a Public Health Perspective. Government of Canada, 2012. Available from https://www.canada.ca/en/public-health/services/chronic-diseases/reports-publications/diabetes/diabetes-canada-facts-figures-a-public-health-perspective.html.
- Footnote 16
-
Harris SB, Tompkins JW, TeHiwi B. Call to Action: A New Path for Improving Diabetes Care for Indigenous Peoples, a Global Review. Diabetes Res Clin Pract. 2017, 123:120-133. doi: 10.1016/j.diabres.2016.11.022. PMID: 28011411.
- Footnote 17
-
Amed S, Dean HJ, Panagiotopoulos C, Sellers EAC, Hadjiyannakis S, Laubscher TA, et al. Type 2 Diabetes, Medication-Induced Diabetes, and Monogenic Diabetes in Canadian Children. Diabetes Care. 2010, 33(4):786–91.
- Footnote 18
-
Public Health Agency of Canada. Type 2 Diabetes. Government of Canada, 2019. Available from: https://www.canada.ca/en/public-health/services/diseases/type-2-diabetes.html.
- Footnote 19
-
Public Health Agency of Canada. Family-Centred Maternity and Newborn Care: National guidelines (Chapter 6). Government of Canada, 2021. Available from: https://www.canada.ca/en/public-health/services/publications/healthy-living/maternity-newborn-care-guidelines-chapter-6.html.
- Footnote 20
-
Health Canada. Nutrition for Healthy Term Infants: Recommendations From Birth to Six Months. Government of Canada, 2015. Available from: https://www.canada.ca/en/health-canada/services/canada-food-guide/resources/infant-feeding/nutrition-healthy-term-infants-recommendations-birth-six-months.html.
- Footnote 21
-
Innovation, Science and Economic Development Canada. Investing in Canada's Future: Strengthening the Foundations of Canadian Research. Government of Canada, 2017. Available from: https://publications.gc.ca/collections/collection_2017/isde-ised/Iu4-223-2017-eng.pdf.
- Footnote 22
-
Public Health Agency of Canada. Chief Public Health Officer of Canada's Report on the State of Public Health in Canada 2021. A Vision to Transform Canada's Public Health System. Government of Canada, 2021. Available from: https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/state-public-health-canada-2021/cpho-report-eng.pdf.
- Footnote 23
-
Government of Canada. Health Inequalities Data Tool. Public Health Infobase. Canadian Community Health Survey - Annual Component (2010-2013). Available from: https://health-infobase.canada.ca/health-inequalities/data-tool/index.
- Footnote 24
-
Patented Medicines Review Board. The Use of Diabetes Drugs in Canadian Public Drug Plans. Government of Canada, 2016. Available from: http://www.pmprb-cepmb.gc.ca/view.asp?ccid=1244&lang=en.
