Responding to syphilis in Canada (fact sheet)
Download the alternative format
(PDF format, 188 KB, 1 page)
Organization: Public Health Agency of Canada
Date published: January 2020
The number of syphilis cases is increasing dramatically.
Outbreaks have been reported in 8 provinces and territories as well as some Indigenous communities.
Figure 1. Syphilis outbreak map
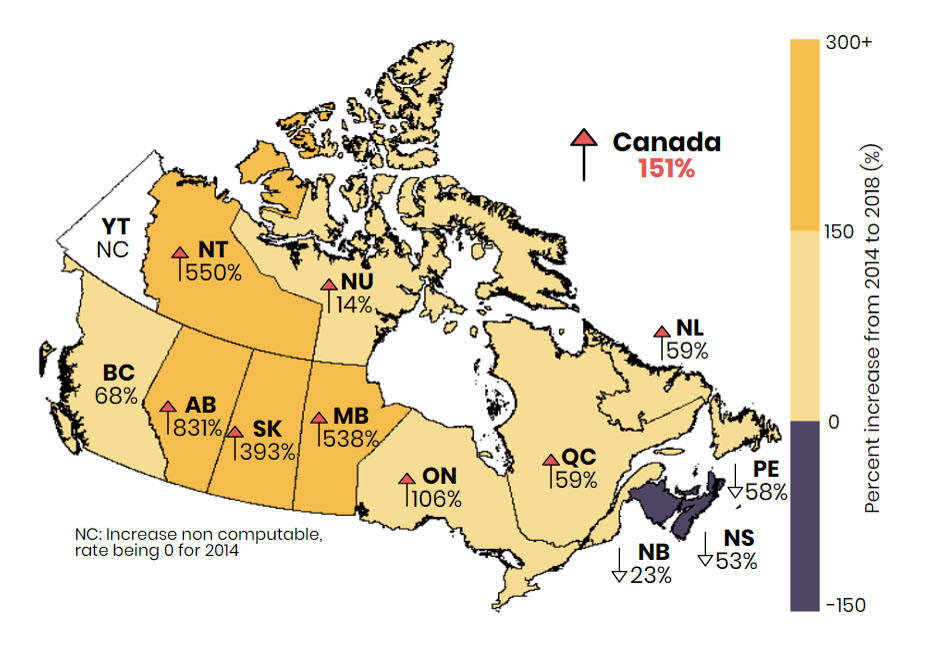
Figure 1: Text description
Provincial and territorial rate increases (%) from 2014–2018:
- Between 2014 and 2018, rates of infectious syphilis increased in most provinces and territories.
- Eight provinces and territories are experiencing outbreaks.
- Increases in rates of infectious syphilis above the Canadian average of 151% were reported by Alberta (831%), Northwest Territories (550%), Manitoba (538%) and Saskatchewan (393%).
- Increases in rates of infectious syphilis below the Canadian average were reported by Ontario (106%), British Columbia (68%), Newfoundland and Labrador (59%) Quebec (59%), and Nunavut (14%).
- Three provinces reported a rate decrease since 2014: Prince Edward Island (‑58%), Nova Scotia (‑53%) and New Brunswick (‑23%).
- The rate of infectious syphilis increased in Yukon Territory since 2014, but as the rate for 2014 was 0, the relative increase from 2014 to 2018 was not computable.
Prior to 2014, over 90% of cases were among men, primarily gay, bisexual and other men who have sex with men (gbMSM).
More heterosexual men are being diagnosed with syphilis and the rates among women have tripled in the past 5 years.
The number of congenital syphilis cases is the highest ever reported (2018), and a further 3-fold increase is anticipated for 2019.
Syphilis is an important public health issue: it can result in significant morbidity such as neuropathologies, decreased visual acuity and hearing, as well as congenital syphilis (stillbirth and birth defects). It can increase HIV transmission and acquisition risk.
What you can do as a health care provider
Talk
Every encounter is an opportunity to screen and prevent syphilis.
Start the conversation about syphilis: let your patients know syphilis infection is serious and on the rise. This is particularly important for women of childbearing age and their partners.
In a safe and respectful way, let them know you're talking to everyone who is sexually active about:
- risk factors - new, anonymous or multiple partners, condomless sex, substance use (e.g., methamphetamine) and/or previous sexually transmitted and blood-borne infection (STBBI)
- risk reduction - encourage safer sex (use of condoms, reducing the number of partners) and couples testing
- signs and symptoms - (e.g., lesions, rashes, swollen glands) and that syphilis may be asymptomatic
Test
Patients may not be aware they were exposed and/or may not notice lesions.
Offer syphilis and other STBBI screening to people with risk factors, sexually active gbMSM and people living with HIV.
- Repeat screening for people at ongoing risk.
- Offer a pregnancy test to women of childbearing age diagnosed with syphilis.
Screen all pregnant women for syphilis, as early as possible.
- Repeat at 28 to 32 weeks of gestation and at delivery in areas with outbreaks or for women at ongoing risk.
- Consider more frequent screening for women at high risk.
Screen all infants born to mothers who were diagnosed with syphilis during their pregnancy.
Prevent
- Treat empirically when syphilis is probable, especially when follow up cannot be assured.
- Screen for HIV in all cases of syphilis.
- Discuss the importance of partner notification and treatment to prevent transmission and/or reinfectionFootnote *.
- Do follow-up testing (serology) to ensure the treatment was successfulFootnote *.
- Consider treating sexual contacts who are within the 90-day window period, without waiting for results.
Resources
- Canadian Guidelines on Sexually Transmitted Infections
- Infectious syphilis in Canada 2009-2018
- Discussing sexual health, harm reduction and STBBIs: A guide for service providers (Canadian Public Health Association)
- Footnote *
-
Refer to the Canadian Guidelines on Sexually Transmitted Infections or your provincial or territorial guidelines for information on treatment, post-treatment testing intervals and trace-back periods.
Your local public health unit can assist you with the management of cases and contacts.