Supporting the advancement of the Framework for diabetes in Canada: Dialogues report

Download the alternative format
(PDF format, 7.03 MB, 15 pages)
Organization: Public Health Agency of Canada
Published: 2023-09-29
Related links
Background
The Framework for diabetes in Canada, tabled by the federal Minister of Health in October 2022, outlines numerous opportunities to improve the lives of people in Canada who are affected by diabetes and the systems that support diabetes care, research, and the prevention of type 2 diabetes.
The Framework was informed by an engagement process conducted with the assistance of Drs. Diane Finegood and Lee Johnston, and the Morris J. Wosk Centre for Dialogue, based at Simon Fraser University (SFU). The Public Health Agency of Canada (PHAC) and SFU have continued to engage Canadians through a series of dialogues in support of the advancement of the Framework and activity on diabetes.
About this report
This report provides a summary of what we heard at two dialogues following the tabling of the Framework. The dialogues were informed by interviews conducted with a sub-set of interviewees who, having contributed to the Framework engagement process, shared with us their thoughts on its content and potential for future conversation. The dialogues were held in March of 2023 and focused, respectively, on two topics deemed widely relevant to furthering action on diabetes – collaboration and knowledge synthesis and mobilization.
The report was independently prepared by Drs. Lee Johnston and Diane Finegood (SFU). Production of this document has been made possible through a financial contribution from PHAC. The report does not provide an overall representation of public opinion, institutional policies or positions, nor that of a randomly selected population sample. Rather, this report presents our synthesis of the ideas expressed by the people who participated in these dialogues. This report does not necessarily reflect the opinions of SFU, the University at-large, nor of PHAC.Acknowledgement
SFU and PHAC are grateful to everyone who took the time to participate in these dialogues, particularly those living with diabetes. Your contributions enriched our conversations and made clear the need to act now to improve care, in its many forms, for the individuals, families and communities affected by diabetes.
Table of contents
- Continuing the conversation about diabetes in Canada
- Dialogue one: Strengthening the diabetes ecosystem in Canada
- Dialogue two: Strengthening knowledge mobilization and synthesis for diabetes in Canada
- Conclusion
- Footnotes
Continuing the conversation about diabetes in Canada
Process
The Dialogue to Help Strengthen the Diabetes Ecosystem in Canada was held on March 2, 2023 and the Dialogue Towards Strengthening Knowledge Mobilization and Synthesis for Diabetes in Canada on March 7, 2023. Invitations to both dialogues were distributed to a list that included everyone who took part in the prior Framework engagement process in 2022. Invitations to the dialogues were also distributed more widely through various organizational networks.
Approximately 45 individuals attended each dialogue. There was considerable overlap in dialogue participants as many individuals signed up for both sessions. Participants represented a wide breadth of experience and perspectives, including people living with diabetes, not-for-profit organizations, health care professionals, researchers, and governmental representatives.
Both events were 2.5 hours in length and hosted on the Zoom platform. Participants received a brief discussion guide prior to both sessions. Supports were offered to increase accessibility including real-time captioning; alt-text documents for blind/low-vision participants; French/English simultaneous interpretation; and $100 honoraria available upon request.
Both sessions opened with a territorial acknowledgement provided by Jessica Guss (Leader, Strategic Initiatives, Indigenous Health, BC Patient Safety & Quality Council). Linxi Mytkolli (Lead of Patient Engagement and Knowledge Mobilization, Diabetes Action Canada) also helped to set up both conversations with tips for engaging respectfully. Diane Finegood served as lead facilitator for both dialogues, with additional facilitators moderating breakout room conversations. Graphic facilitator Sam Bradd attended both sessions to provide a visual recording of key messaging. His work can be found in this report.
Dialogue one: Strengthening the diabetes ecosystem in Canada
Overview
The goal of this dialogue was to foster conversation about the current state of collaboration on diabetes and opportunities for improving our collective efforts. To start the session off, participants were polled (using Mentimeter) for their priorities among a list generated by previous dialogues and the Framework. A brief discussion was held about the poll results, which highlighted that participants prioritized addressing inequalities related to the social determinants of health. They also gave priority to enhancing knowledge exchange and education, validating the topic for the second dialogue.
The remainder of the session was built around breakout group conversations in which participants shared their own experiences and their hopes for the future. To help set the context for these conversations, Diane introduced the concept of a "collaboration spectrum" which identifies different types of relationships along a continuum ranging from purely competitive to fully joined together in purpose and structure.
The Collaboration Spectrum
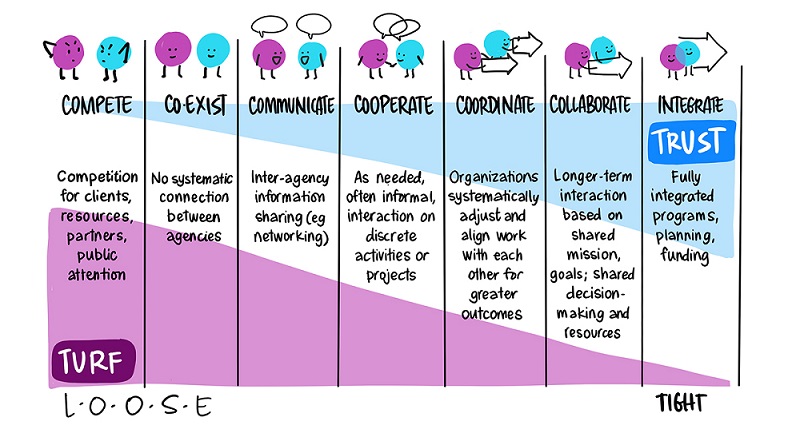
Figure 1 - Text description
The image contains blue and purple chart labelled "The Collaboration Spectrum." The chart is divided vertically into 7 even sections that illustrate separate stages in the spectrum. The left side of the spectrum is labelled as "turf" and the right-most side of the spectrum is labelled as "trust."
The left-most section is labelled at "Compete", with an illustration of a blue blob and a purple blob arguing, with the text: "Competition for clients, resources, partners, public attention." The next section on the spectrum is labelled as "Coexist", with the same two blobs now standing beside each other with a smile on their faces and the text; "No systematic connection between agencies."
The third section is labelled as "Communicate", with the two blobs now talking to each other with positive expressions, and the text "Inter-agency information sharing (e.g. networking)". The next section to the right is labelled as "Cooperate", with the two blobs now shaking hands, with the text: "As needed, often informal, interaction on discrete activities or projects."
The next section or stage is labelled as "Coordinate", with the two blobs holding arrows that are pointing in the same direction, also with the text: "Organizations systematically adjust and align work with each other for greater outcomes." The next stage is labelled as "Collaborate" with the two blobs holding a singular arrow, with the text: "Longer-term interaction based on shared mission, goals; shared decision-making and resources." The last stage is labelled "Integrate", with the two blobs overlapping each other, with the text: "Fully integrated programs, planning, funding."
©Tamarack Institute, Illustration by Sam BraddFootnote *
Breakout rooms were assigned randomlyFootnote †, enabling a diverse mix of participants in each room. The conversations were rich and varied, and reflective of the passion and commitment that dialogue attendees have towards improving the lives of Canadians living with diabetes. In many respects the conversation echoed what we learned during the engagement before the Framework was tabled. For this report, we have highlighted key themes from the conversations that move us beyond the previous dialogues and into ideas related to future collaborative action on diabetes.
Theme 1: Build momentum towards creating meaningful, collaborative action on diabetes
An overarching message heard during the session was that more collaboration is very much needed to overcome the silos and challenges currently holding back progress in many areas related to diabetes in Canada. Participants spoke to the need for collaboration across the health care systems, within care teams, in relation to policy design and implementation, and between decision-makers and community members to address the underlying conditions that foster inequity in diabetes prevalence and outcomes. They spoke to gaps in care that exist for both type 1 and 2 diabetes, and across different geographic regions that have differing levels of access to resources and care. Connecting and integrating the efforts of organizations, community members individuals was seen as a means of making real progress on addressing many of the issues outlined in the Framework. Participants suggested that opportunities exist to leverage resources that are already in place by building linkages between like-minded parties.
Intrinsic to this conversation was a discussion about the quality of collaboration that needs to occur. Many participants would like to see collaborative efforts that are co-created to help reduce the hierarchies that currently exist in Canada's diabetes ecosystem and are reflected in the inequities of diabetes' disproportionate impact on racialized and Indigenous communities. Reflecting on the collaboration spectrum, they spoke to ways of building trust through encouraging long-term commitment to relationships and shifting away from structures that foster competition for resources to support short-term pilot projects. Participants also spoke to the time and labour necessary to building trust in collaborative relationships, particularly with and within community. Indigenous ways of knowing and practices, such as sharing circles, were identified as ways to help decolonize our thinking about collaboration.
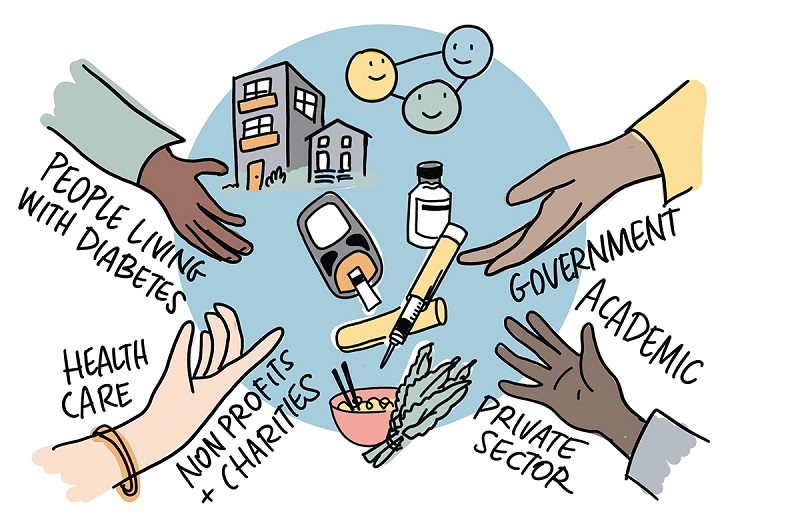
Figure 2 - Text description
Representing cross-sector collaboration, four open hands reach into the centre of a circle. These words are around the hands: People living with diabetes, Government, Academic, Health care, Non profits and charities, Private sector. The four hands are different tones, and one is wearing a bracelet. Inside the circle, representing both systemic issues for people living with diabetes as well as daily experiences, there are small icons of multi-family housing, 3 people being symbolically connected as a trio, insulin and glucose monitoring equipment, a bowl of noodles with chopsticks and leafy greens.
Theme 2: Position people living with diabetes at the heart of collaboration

Figure 3 - Text description
Six people sit in a semi circle, dressed casually and who are having an engaged discussion together, representing a range of ages, genders and showing both professional and lived expertise. Above them are symbolic talking bubbles that overlap and these words are in a ribbon connecting the speech bubbles: Lived Experience, systemic Inquiry, Professional Expertise. Overall, each person in this group could have both lived experience and processional expertise. From left to right: older masculine person with short hair in manual wheelchair, Sikh turbaned man holding cellphone wearing a hoodie, racialized woman with long pink highlighted hair in overalls taking notes on a clipboard, a Black woman with short natural hair in professional suit jacked and pants is leaning forward listening actively, a racialized doctor with long brown hair in a white doctor's coat and glasses is also taking notes on a tablet, a white man, who is blind, with short brown hair wearing a collared shirt sits with his eyes closed and a guide dog at his feet.
Centering people with lived experience (PWLE) with diabetes in our collaborative efforts was a dominant theme in these conversations. PWLE are seeking a seat at the table in the form of meaningful inclusion in decision-making and planning, including in the area of resource allocation. They noted that collaboration between professionals was insufficient; more needs to be done to work with those living with diabetes and their communities. Another essential component of tapping into the rich resource of information provided by PWLE is the creation of infrastructure that financially reimburses them for their contributions. Diabetes Action Canada's patient partners program was noted as an example of a supportive infrastructure.
Health care was another area in which people with diabetes called for reform. PWLE are looking for more trust and collaboration in the patient-provider relationship, and the use of patient-centered, strength- based approaches that embrace cultural humility. This approach was noted as being important for managing chronic conditions like diabetes, given that positive outcomes are more likely to occur when patients are actively involved in their care plan and receive guidance in a respectful and appropriate manner. PWLE asked that providers ask, rather than tell, and work to be active listeners. As one individual noted, "if you are not the one with diabetes, you are the guest in the relationship."
Theme 3: Collaborate in equitable ways, for equitable outcomes
Given that equity was identified as a key priority during the session's opening poll, it was not surprising that the theme carried through to breakout room conversations. Participants spoke of the need to move upstream with collaborative efforts in order to improve prevention of type 2 diabetes, and mitigate the negative impacts of diabetes for populations disproportionality affected by the disease in all its forms. They noted moving the dial in this area will require that leaders work closely with communities, respecting their wisdom and strong networks of relationships.
Participants want to see collaboration across schools, hospitals and other community organizations in the service of improving the material conditions for folks living with diabetes. Community workers were cited as being an untapped resource that, with the right system for collaboration in place, could help lessen the burden on the health care system and physicians and provide more accessible service to patient with lower socio-economic status or who lack trust in the medical system.
Dialogue attendees also challenged the broader systems that guide the diabetes ecosystem in Canada, noting a lack of intersectional understanding of the ways in which race, class, Indigenous status, queer identity and other factors impact an individual's experience of having and managing their diabetes. This theme was echoed in the dialogue on knowledge mobilization and synthesis, particularly in regard to how research on diabetes is organized.
Figure 4 - Text description
Four people, with multiple genders and races, are standing an collaborating at a whiteboard which reads, Coming Together for Impact. On the whiteboard is a small diagram with two loops and connected dots. In front of the whiteboard is a round table, on it is a flip char which reads "housing, food security, justice" like a to-do list. The four people are a white man with glasses and a goatee, a Black woman with locs and long hair in a suit who's pointing at the diagram, an Indigenous person with long braided hair who is holding a pen up to the board, and a racialized man with short hair who is smiling and holding up paper casually.
Dialogue two: Strengthening knowledge mobilization and synthesis for diabetes in Canada
During previous public engagement in support of the Framework, a diverse range of participants spoke to challenges in translating knowledge into action in ways that meaningfully improve the lives of Canadians affected by diabetes. This dialogue was designed to strengthen our collective understanding of the landscape of diabetes knowledge and identify opportunities to build on our current assets.
To help set the context for this session, Diane overviewed how data, often in the form of numbers or counts, can be processed into information (groupings that answer who, what, where and when questions). When used in the service of answering questions, information can be considered knowledge, which in turn builds our understanding as we begin to examine patterns and draw connections. The presence of wisdom speaks to an understanding of why and how we use data (and information, knowledge and understanding), and to what ends. The theme of wisdom in relation to lived experience was a strong one over the course of the dialogue.
The rest of the session was organized around two breakout sessions that asked participants to discuss promising practices in knowledge about diabetes, as well as consider opportunities for change. Some aspects of the conversation reinforced what we heard during the Framework engagement process. Individuals and organizations interested in diabetes emphasized the importance of data, particularly when analyzed and applied well and appropriately. However, they remain frustrated with Canada's failure to build systems that capitalize on data collection. Data is not reaching its full potential due to persistent silos, system gaps and the patchwork approach to its management, exacerbated in healthcare by our 13 different provincial and territorial systems of care.
Theme 1: Integrate an equity lens in our thinking about data and knowledge
Equity was a driving theme in conversations about data and knowledge, much as it was during the engagement process and in the dialogue on the diabetes ecosystem. Participants spoke to systemic injustices across the board in relation to data – its collection, analysis, focus and application. They called for a shift in the focus of data collection towards addressing populations who have been historically excluded. Speakers suggested we expand data collection into less traditional areas relevant to addressing the upstream determinants of health, including information about language barriers, newcomer status, service access, transportation barriers and others. These social risk factors would complement and expand on the use of clinical risk factor data to improve diabetes screening practices and other forms of care.
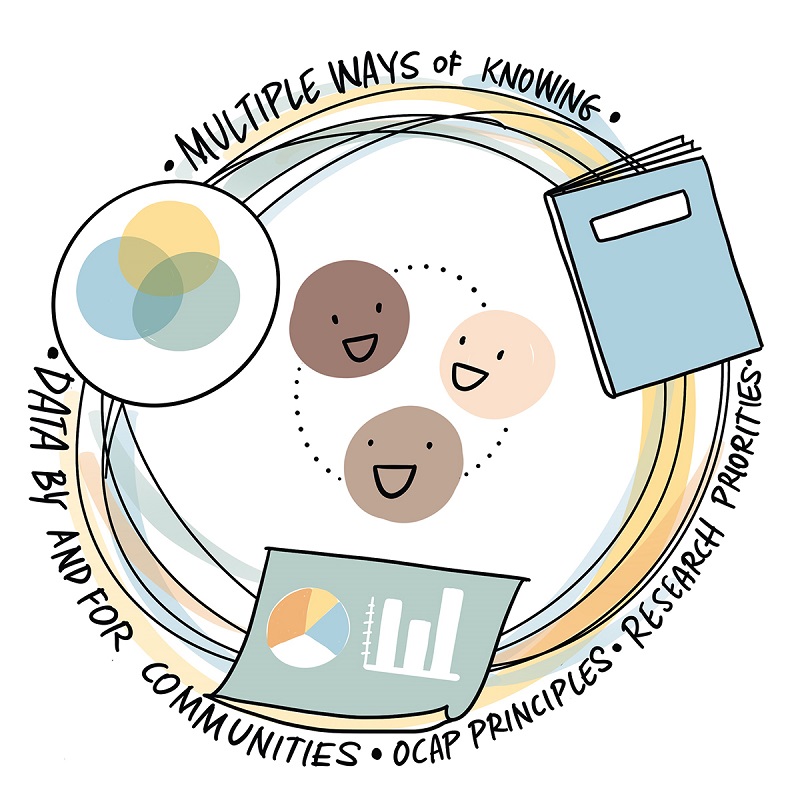
Figure 5 - Text description
An abstracted model about equity and ways of having knowledge. The main structure is a large circle made up of artistic, thin, overlapping, and muted rings; this gives the impression of the circle being dynamic and moving slightly. Then, three icons are placed on the circle: a small venn diagram, a book, and a poster with a pie chart/bar chart. Inside the circle are three emoji faces in three skin tones, connected as a trio with lightly dotted lines. Wrapping around the entire circle/ring is text that says, "multiple ways of knowing; data by and for communities; OCAP principles; research priorities" and in this way, the three icons can connect to any of these words. The overall impression is that there are multiple ways of knowing, with all the icons of equal sizes, and the diagram balances qualitative, quantitative and oral ways of sharing.
Researchers identified structural problems in the systems that support data collection and management, noting a lack of research funding to support work with priority populations. They called for research infrastructure that supports work that helps us understand the impacts of racism, colonialism, and structural inequities on individuals and populations. Participants also spoke of the need for cultural humility and respect when working with data, noting the complex history of race- and ethnicity-based data collection, and its weaponization against Black and Indigenous populations. They noted that data should be tailored to different population needs and respect the different lines they may have drawn in their perceptions of what constitutes knowledge, understanding, and wisdom. No one size fits all. Community priorities should help guide decision-making with respect to data and knowledge management.
Theme 2: Engage in more effective and meaningful knowledge mobilization and translation
Participants spoke to the benefits of easy access to digital platforms and networks for knowledge sharing, and the advantages that these provided during the COVID-19 pandemic. They also noted that, while we have more information than ever about diabetes, it is not always effectively distributed or available to those who need it. Good information is competing with a sea of digital misinformation that makes it increasingly difficult for patients and populations to access information that is reliable and relevant. One participant spoke to the challenge by noting that much of the information available to patients is "oversimplified but under-nuanced," often leaving individuals inadequately resourced but still responsible for their own decision-making. Attendees spoke to both the need for enhanced health literacy among patients and easily accessible, evidence-based information from consistent sources. They also called for more evaluation of knowledge mobilization and translation projects to better understand if information is reaching its targeted audience, being understood, and then applied for improved outcomes.
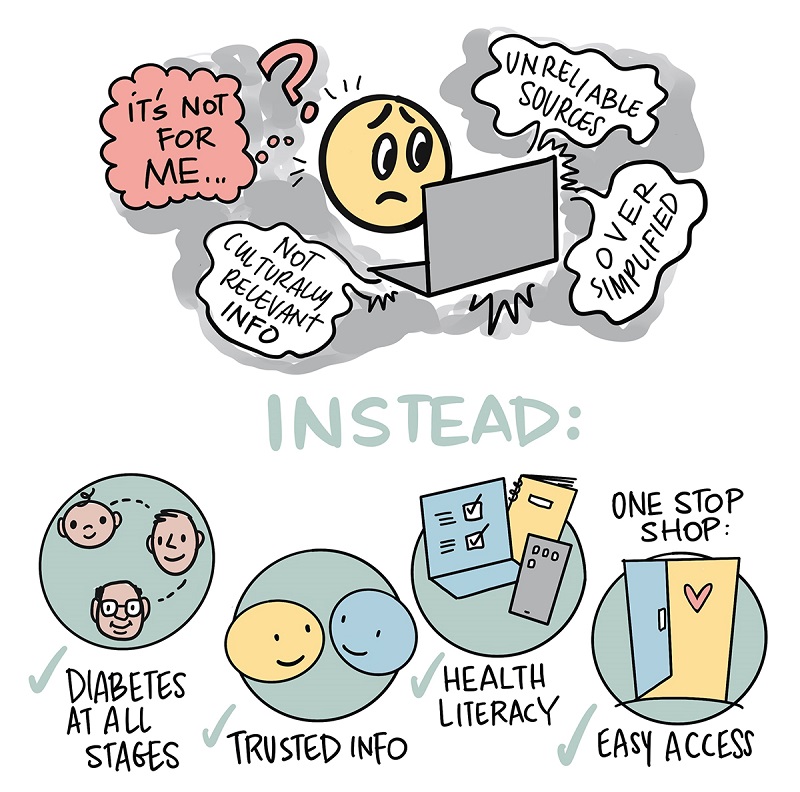
Figure 6 - Text description
A cartoon diagram in two parts. The first part is an emoji smiley-face character that looks very worried, looking at a laptop screen: representing bad information, the screen has threatening/ confusing wavy speech bubbles coming from it that say "not culturally relevant info, over simplified, unreliable sources." The character has a huge question mark over its head and the text in red/contrasting colour says "it's not for me". Under this diagram are big capital letters saying “instead”. The second part of the diagram is solution-focussed with checkmarks representing what is better:
- Diabetes at all stages (icons of baby, middle aged person, older person)
- Trusted info (two smiling emoji faces looking at each other)
- Health literacy (icon of computer with checkmark, brochure and phone)
- Easy Access and One Stop Shop (icon of an open door with a heart on it)
Participants reflected on the need to improve access to formal diabetes education and suggested improving access with more educators, the ability to engage diabetes-trained pharmacists, the development of a one-stop shop, and a range of resources that meet people where they are at. Attendees spoke of inequity in access to information that is culturally appropriate, and the need to acknowledge other systems of seeing and knowing that might not align with traditional models of information exchange. In regard to improved access to information, there were calls to more effectively tap into vehicles for dissemination including virtual courses on diabetes care, public awareness campaigns, social media platforms and community-based distribution (such as through community health centres).
Theme 3: Accelerate the exchange of wisdom through peer and community support
As documented by people living with diabetes, self- management is an isolating and challenging process. It is made more difficult by the many structural challenges patients experience. People living with diabetes frequently remind us that the psychological and emotional burden of diabetes management is steep. In this dialogue they also reminded us that individuals who have learned to manage their diabetes have accumulated a substantial body of wisdom. Peer-to-peer support was highlighted as a special resource for inter- personal knowledge exchange. Dialogue participants with lived experience of diabetes spoke to the power of mentorship and suggested that sharing practices in this way could be key to helping others transform information into their own understanding and wisdom.

Figure 7 - Text description
This is a scene of people cooking together in a First Nations community kitchen with a drop in health clinic operating in the background. In the foreground, three people with different body sizes and lengths of hair, wearing aprons and talking/laughing, are sitting and standing peeling tomatoes with kitchen pots on the tables in front of them. It's a busy and active scene where people are doing multiple things to support their health physically, emotionally, spiritually and mentally with community support. In the background, a large banner with a First Nations medicine wheel and the words "community kitchen and outreach today" hangs on the wall. Next to the banner and door and in the background is a second scene, where a health care provider wearing scrubs and a nametag is seated alongside a patient, taking their blood pressure, and both people have relaxed facial expressions. Behind them is a poster with a beaded stethoscope on the wall and a heart.
Participants spoke of building infrastructure, such as communities of practice, to help support peer and other information exchange. The COVID-19 pandemic was identified as having both positive and negative impacts on networking and peer learning. While individuals lost opportunities to gather in person, the rise in online meeting technology helped to overcome geographic challenges and fostered some new connections between patients, advocates and experts. Social media like Facebook, Reddit, and podcasts were seen as helpful, but not without risk of misinformation. They were also seen as biased and privileging young white individuals who often have access to the latest diabetes equipment. As such it was deemed especially important that we find ways to financially support those who support others through peer- support, including Indigenous knowledge keepers.
Conclusion
Over the course of the two dialogues documented here, key themes emerged that built on those expressed in the Framework and the engagement that informed it. Invested individuals and organizations are seeking collaborative efforts and knowledge mobilization that serve to reduce inequities, move us upstream toward addressing the social determinants of health, work with communities to understand their priorities, and are built around an explicit commitment to centering the experiences of those living with diabetes.
Taken together, these dialogues presented an opportunity for participants to gather and reflect not only on collaboration and knowledge mobilization, but on the path forward after the tabling of the Framework for Diabetes in Canada. To this end participants asserted that they are ready for action in ways that bring diverse participants together and provides the infrastructure to support meaningful participation and contribution. The attendees of these dialogues reflect a national readiness to act on efforts to improve the lives of Canadians affected by diabetes.
Footnotes
- Footnote *
-
All Illustrations are by Sam Bradd
- Footnote †
-
Note: due to technical limitations we were unable to offer simultaneous French/English interpretation in all breakouts. French participants were therefore grouped together with the interpreter(s) in both dialogues.