Concussions and their association with mental health in Canadian adolescents
Download the alternative format
(PDF format, 1.9 MB, 13 pages)
Organization: Public Health Agency of Canada
Type: Publication
Date published: 2022-01-04
Related topics
Findings from the 2018 Health Behaviour of School-aged Children (HBSC) Study.
On this page
- Introduction
- Prevalence of concussions among youth
- Prevalence of concussions by race
- Activities associated with concussions
- Locations where concussions occur
- Association between concussion and mental health
- Limitations
- Conclusions
- Methods
- References
- Acknowledgements
Introduction
There is growing public awareness about the importance of concussions in the lives of young Canadians (PHAC, 2020b). Population-level data on concussion and its causes is essential to the planning of health promotion initiatives.
Concussions have short-term and long-term effects on the brain (McCrory et al., 2013). It is plausible that concussions influence areas of mental health that are of importance to youth.
This report describes the prevalence of concussions among Canadian youth and examines the relationship between concussion and indicators of mental health status among young people.
This report is based on information from the HBSC national report (PHAC, 2020) and Farmer et al, 2021.
Prevalence of concussions among youth
In 2018, 11.0% of students in grade 6 to 10 reported that they had a medically diagnosed concussion within the past year. 8.7% of these students reported that they had a single concussion and 2.3% reported that they had multiple concussions.
Concussions were more common in grade 8 to 10 students than in grade 6 to 7 students.*
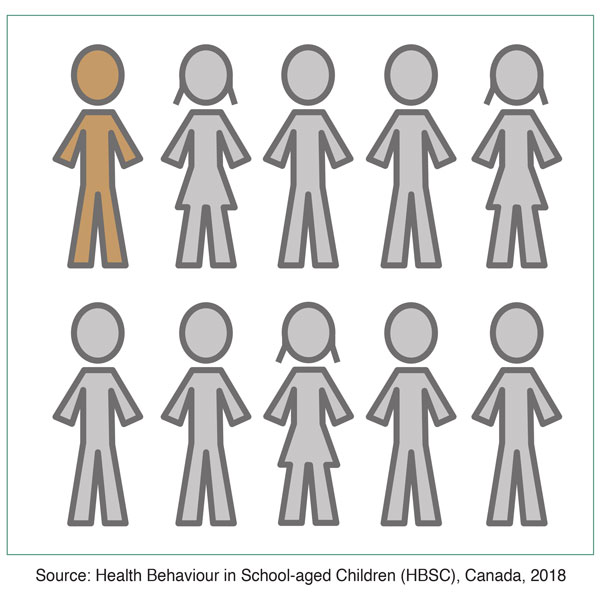
Figure 1: Text equivalent
About 1 in 10 youth had a concussion within the past year.
Source: Health Behaviour in School-aged Children (HBSC), Canada, 2018.
* Refer to Chapter 9 of the HBSC national report for more information on concussions, including prevalence by grade and gender.
Prevalence of concussions by race
This figure illustrates the percentage of youth who reported that they had a concussion in the past year according to race.
Concussions were the most common among Indigenous youth (14.2%) and least common among East Indian and South Asian youth (6.2%).
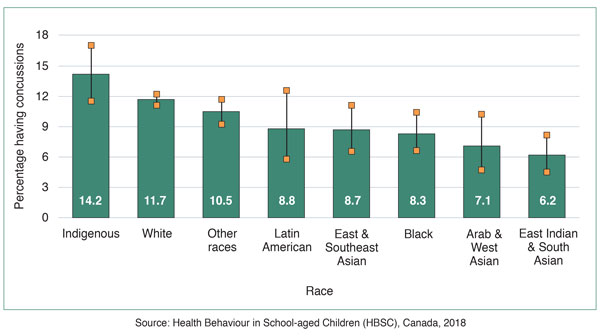
Figure 2: Text equivalent
| Race | Indigenous | White | Other races | Latin American | East & Southeast Asian | Black | Arab & West Asian | East Indian & South Asian |
|---|---|---|---|---|---|---|---|---|
| Percentage having concussions | 14.2 | 11.7 | 10.5 | 8.8 | 8.7 | 8.3 | 7.1 | 6.2 |
| Percentage low to high | 11.5 to 17.0 | 11.1 to 12.2 | 9.2 to 11.7 | 5.8 to 12.6 | 6.5 to 11.1 | 6.6 to 10.4 | 4.7 to 10.3 | 4.5 to 8.2 |
| Source: Health Behaviour in School-aged Children (HBSC), Canada, 2018 | ||||||||
Activities associated with concussions
Almost 6 in 10 concussions among youth occurred while they were participating in a sport. Concussions occurred during both contact and non-contact sports. Boys were more likely than girls to have sustained their most recent concussion while participating in sport.
Figure 3: Text equivalent
| N/A | Boys | % | Girls | % |
|---|---|---|---|---|
| Sport | Boys:
|
65.4% | Girls:
|
52.6% |
| Driving or passenger in a motorized vehicle (includes off-road vehicles) | - | 4.6% | - | 3.9% |
| All other activities | - | 30.0% | - | 43.5% |
| Source: Health Behaviour in School-aged Children (HBSC), Canada, 2018 | ||||
Locations where concussions occur
The most common place for concussions to occur were community facilities such as recreation buildings and sports fields.
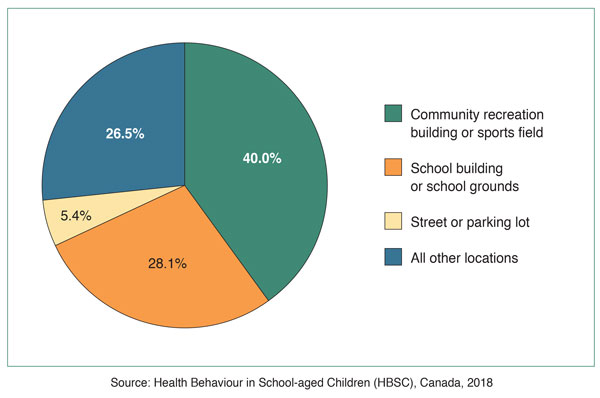
Figure 4: Text equivalent
| Community recreation building or sports field | 40.0% |
|---|---|
| School building or school grounds | 28.1% |
| Street or parking lot | 5.4% |
| All other locations | 26.5% |
| Source: Health Behaviour in School-aged Children (HBSC), Canada, 2018 | |
Association between concussion and mental health
Youth who had a concussion in the past year were less likely to be highly satisfied with their life and more likely to report a lot of emotional problems and poor psychological well-being.
Concussions were associated with many poor/negative mental health outcomes among youth.
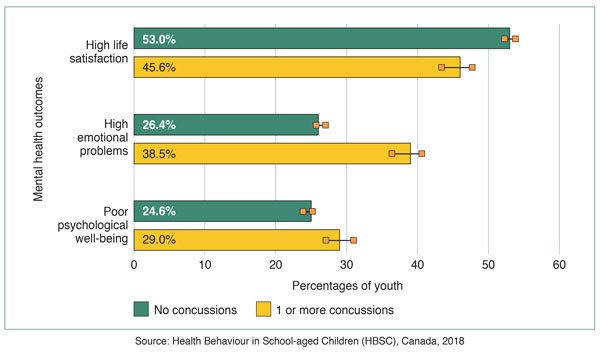
Figure 5: Text equivalent
| Percentages of youth | Mental health outcomes | ||
|---|---|---|---|
| High life satisfaction | High emotional problems | Poor psychological well-being | |
| No concussions | 53.0% | 26.4% | 24.6% |
| (% low to high) | (52.3 to 53.8) | (25.7 to 27.0) | (23.9 to 25.2) |
| 1 or more concussions | 45.6% | 38.5% | 29.0% |
| (% low to high) | (43.5 to 47.8) | (36.4 to 40.6) | (27.1 to 31.0) |
| Source: Health Behaviour in School-aged Children (HBSC), Canada, 2018 | |||
- High life satisfaction: Respondent ranks how happy they are with their life as at least 8 on a laddered scale of 1 to 10.
- High emotional problems: Respondent reports that they often have difficulty getting to sleep and frequently feels depressed, in a bad mood, and nervous.
- Poor psychological well-being: Respondent reports that their life is not "filled with things that interest them", and they often do not feel: "in good spirits", "calm and relaxed", "active and vigorous", or "fresh and rested".
Limitations
All research studies have limitations and it is important to interpret results in light of their limitations.
- All data in the HBSC were collected using self-report, which is prone to reporting biases (Choi & Pak, 2005). This could have led to an underestimate of the true number of concussions. Concussions can be difficult to diagnose and the rate of diagnosis can vary across demographic groups (Bressan & Babl, 2016, Bergeron, 2019).
- All data in the HBSC were collected in schools. Students who were absent from school while recovering from a concussion would not have participated in the survey, leading to an underestimate in the number of concussions among students.
- The cross-sectional design of the HBSC does not allow for the inference of causality. Longitudinal designs would be required to determine that concussions led to poorer mental health outcomes.
- Students were asked to respond to the question "Are you male or female?" by selecting from the three responses, "male", "female" or "neither term describes me". Students who indicated "neither term describes me" did not comprise a large enough group to include in the statistical analyses.
Conclusions
- About 1 in 10 youth reported having a concussion in the last 12 months.
- Boys, older youth, and Indigenous youth were at increased risk of having a concussion.
- About 6 in 10 concussions in youth occur while they were participating in a sport and concussions occurred in both contact and non-contact sports.
- Most concussions occurred at community and school locations where youth engage in sport and other physical activities.
- Concussions were associated with many negative mental health outcomes.
Methods
Data source
Data are from the 8th cycle of the Canadian Health Behaviour in School-aged Children (HBSC), a World Health Organization cross-national research study that focuses on the health of 11-15 year-old students and is conducted every 4 years.
The main purposes of the HBSC are to understand youth health and well-being, and to inform education, health policy and health promotion programs in Canada and abroad.
Eligible school classrooms across Canada were selected at random and invited to participate in the study. In 2018, all provinces and two territories participated. In total, 21,753 Canadian youth from 394 schools completed the study.*
* Refer to Chapter 1 of the HBSC national report for more information on the HBSC survey methods.
Statistical analysis
Standard descriptive statistics were used to describe the sample. Nationally-representative estimates were calculated using survey weights, which reflected student enrollment within grades 6 to 10 by province/territory.
Chi-square tests augmented by confidence intervals were used to determine whether concussion prevalence differed by gender, race and socioeconomic status, as well as how the frequency of the mental health outcomes differed across youth based on their concussion status. To supplement the analyses that compared the prevalence (likelihood) of mental health outcomes groups of children with and without concussions, regression models were also employed. Bivariate logistic regression models were used to compare the relative odds of the mental health outcomes according to concussion status. Subsequent models adjusted for confounding variables.
References
Bergeron, G. L. (2019). Incidence, Awareness, and Reporting of Sport-Related Concussions in Manitoba High Schools. Can J Neurol Sci, 46(4), 443-450. https://doi.org/10.1017/cjn.2019.58
Bressan, S., & Babl, F. E. (2016). Diagnosis and management of paediatric concussion. J Paediatr Child Health, 52(2), 151-157. https://doi.org/10.1111/jpc.12967
Choi, B. C. K., & Pak, A. W. P. (2005). A catalog of biases in questionnaires. Preventing Chronic Disease, 2, A13.
Farmer, M., Pickett, W., & Janssen, I. (2021). Concussions and their associations with mental health amongst Canadian youth. Manuscript submitted for publication.
McCrory P., Meeuwisse W.H., Aubry M., et al. (2013). Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. British Journal of Sports Medicine 2013; 47:250-258.
Public Health Agency of Canada [PHAC]. (2020). The health of Canadian youth: Findings from the health behaviour in school-aged children study. Retrieved from https://www.canada.ca/en/public-health/services/publications/science-research-data/youth-findings-health-behaviour-school-aged-children-study.html
Public Health Agency of Canada (2020b). Spotlight on traumatic brain injuries across the life course. Ottawa: PHAC, Cat.: HP15-14/2019E-PDF, 150p.
Acknowledgements
- Health Behaviour in School-aged Children (HBSC) is an international study carried out in collaboration with the World Health Organization, European Region (WHO/EURO). The International HBSC Coordinator was Dr. Joanna Inchley (University of Glasgow, Scotland) for the 2017/18 survey and the Data Bank Manager was Dr. Oddrun Samdal (University of Bergen, Norway). The Canadian 2017/18 HBSC survey was funded by the Public Health Agency of Canada, the principal investigators were Drs. (the late) John Freeman, William Pickett and Wendy Craig (Queen's University), and the national coordinator was Matthew King (Social Program Evaluation Group, Queen's University).