Prolonged pertussis outbreak in Ontario


Download this article as a PDF (396 KB - 8 pages)
Published by: The Public Health Agency of Canada
Issue: Volume 40-3: Pertussis
Date published: February 7, 2014
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 40-3, February 7, 2014: Pertussis
Outbreak report
Prolonged Pertussis Outbreak in Ontario Originating in an Under-immunized Religious Community
Deeks SL1,2*, Lim GH1, Walton R1, Fediurek J1, Lam F1, Walker C3, Walters J4, Crowcroft NS1,2,5
Affiliations
1 Public Health Ontario, Toronto, ON
2 Dalla Lana School of Public Health, University of Toronto, Toronto, ON
3 Elgin St. Thomas Public Health
4 Wellington-Dufferin-Guelph Public Health
5 Department of Laboratory Medicine and Pathobiology, Faculty of Medicine, University of Toronto, Toronto, ON
Correspondence
DOI
https://doi.org/10.14745/ccdr.v40i03a03
Abstract
Background: A prolonged pertussis outbreak began in Ontario in November 2011 in an under-immunized religious community and subsequently spread to the general population and a second religious community in the same region of the province.
Objective: To compare the epidemiology in the religious communities to that of the general population within the affected jurisdictions.
Methods: The analysis includes cases reported through the integrated Public Health Information System (iPHIS) between November 1, 2011 and April 15, 2013 that met the outbreak case definition. Health unit staff assessed whether cases were members of religious communities through case investigations and collected information on immunization status, treatment and outcomes.
Results: A total of 443 confirmed and probable outbreak cases were reported in 7 health units. The outbreak began in one religious community (138 cases), before spreading to the general population in the region (273 cases). A second under-immunized community within the region experienced 32 cases. Thirteen cases were hospitalized and no deaths were reported. Disease peaked earlier in the religious community; cases were significantly younger, more likely to be at high risk for pertussis and more likely to be unimmunized. Among the fully immunized general population, 51% of cases were between 10-14 years and with a median of 5.6 years since their last immunization.
Conclusion: The epidemiology of pertussis in the under-immunized community is distinct from the general population. Transmission of pertussis to the general community is not unexpected during an outbreak; however, the proportion of cases up to date with immunization warrants further investigation.
Introduction
Between 2010 and 2012, a number of jurisdictions throughout North America were experiencing pertussis outbreaks Footnote 1 Footnote 2 Footnote 3 Footnote 4 Footnote 5. Pertussis is a highly communicable respiratory infection caused by Bordetella pertussis, which is most dangerous in infants under one year of age; particularly those under four months. Footnote 6 Footnote 7 Disease control is challenging due to the long period of communicability, the disease's atypical presentation among adults and immunized children and the fact that it can be difficult to diagnose. Footnote 8 Footnote 9 Footnote 10
Pertussis vaccines have been available in Ontario since 1943. In 1984, a combination adsorbed whole cell pertussis vaccine was used in the province's universal publicly-funded immunization program. In 1997, acellular pertussis vaccine replaced the whole cell vaccine and was delivered as part of a combination product (diphtheria [D], tetanus [T], acellular pertussis [aP], inactivated polio vaccine [IPV] and Haemophilus influenzae type b [Hib]) at 2, 4, 6 months of age, with a pentavalent (DTaP-IPV-Hib) booster dose at 18 months and a quadrivalent booster dose (DTaP-IPV) at 4-6 years of age. In 2003, an adolescent dose was publicly-funded using dTap at 14-16 years of age. Finally, in 2011, a single dose adult pertussis immunization program was introduced. Footnote 11
On January 25, 2012 a provincial outbreak of pertussis was declared after a cluster of cases was detected in an under-immunized religious community (religious community A) in southwestern Ontario, Canada. The outbreak was initially limited to three health units (HUs) and one religious community (A) but subsequently spread to the general community and a second under-immunized religious community (B) in 7 HUs in the province.
Our objective is to report on the outbreak investigation, comparing the epidemiology in the religious communities to that of the general population, including demographics, immunization status, treatment and outcomes.
Methods
Surveillance
Pertussis is a legally reportable disease in Ontario (population 13.5 million in 2012).12 Cases are identified passively and case information is entered into a provincial reportable diseases registry, the integrated Public Health Information System (iPHIS). Pertussis outbreak case definitions which included a geographic component were established and modified three times throughout the course of the outbreak to reflect the evolving situation. The outbreak period was between November 1, 2011 and April 15, 2013. We extracted data entered into iPHIS meeting the confirmed and probable pertussis outbreak case definitions on August 22, 2013. Extracted data included demographic information, laboratory results, hospitalization status, outcome, and immunization history, although completeness varied by field. We determined episode date for each case using a standardized hierarchy: symptom onset date was preferentially selected, specimen collection date if symptom onset was unavailable, and case reported date if both were unavailable.
Early in the outbreak, we supplemented iPHIS data with additional case note data using an enhanced case report form to gather information on whether the case was at high risk for pertussis, as well as health seeking behavior and treatment. A manual case record review was undertaken on cases reported between November 1, 2011 and August 15, 2012. We classified persons as high risk for pertussis if they were pregnant or under 1 year of age, and assessed whether cases obtained laboratory testing, initiated antibiotic therapy and the time interval to seek treatment.
HUs were requested to identify connection(s) to under-immunized communities within iPHIS. We classified cases as being from one of two under-immunized religious communities, A and B, using specific exposure identifiers. For some analyses, religious communities A and B were combined. We assumed cases not assigned to either exposure identifier originated from the remaining HU population, (the general population).
As accurately assessing immunization status from a single field in iPHIS was problematic, we reviewed the following fields for all cases: immunization agent, immunization administration dates, relevant immunizations up-to-date (RI), and risk factor (RF). The number of doses of pertussis-containing vaccine received was established based on the number of administration dates reported for each case. We determined the validity of doses by considering minimum age and minimum interval requirements between doses, as per the Ontario publicly funded schedule.Footnote 13 An interval of at least 14 days prior to disease onset was required for a dose to be considered valid. We assessed cases without any valid doses (i.e., no administration dates) as unimmunized if RI=No or RF=unimmunized; otherwise we assessed these cases as having unknown immunization status. We assessed cases with at least one valid dose as being complete for age (i.e., up to date) or partially immunized in accordance with the provincial immunization schedule and guidelines established by the National Advisory Committee on Immunization. Footnote 11 Footnote 14
Statistical analyses
We calculated incidence rates per 100,000 population using demographic data from Statistics Canada obtained through IntelliHealth Ontario. Population data by HU were unavailable at the time of analysis for 2013; 2012 population data were substituted. Descriptive analyses and statistical tests were performed using SPSS version 19 (IBM, Armonk, NY, USA) and SAS version 9.2. We compared median age and time intervals for selected outcomes between communities using the Kruskal-Wallis test; statistical significance was declared at p<0.05. Where appropriate, we excluded missing data from analyses.
Results
Descriptive epidemiology
A total of 443 pertussis cases were reported by 7 outbreak-affected HUs during the outbreak period. Of these, 344 cases (77.7%) were classified as confirmed based on laboratory confirmation of pertussis or an epidemiologic link to a laboratory-confirmed case and the remaining 99 were classified as probable based on symptomatology. Cases ranged in age from 14 days to 68 years, with a median age of 9.4 years (age was missing for 6 cases). Females accounted for 56.0% of cases. The annualized incidence rate during the outbreak was 25.7 cases per 100,000 population (2012 population of 7 HUs was 1.2 million people). The overall provincial rate during the same time period was 6.1 pertussis cases per 100,000 population. Thirteen cases (2.9%) were hospitalized and there were no deaths. All hospitalized cases were children and 8 were under one year of age.
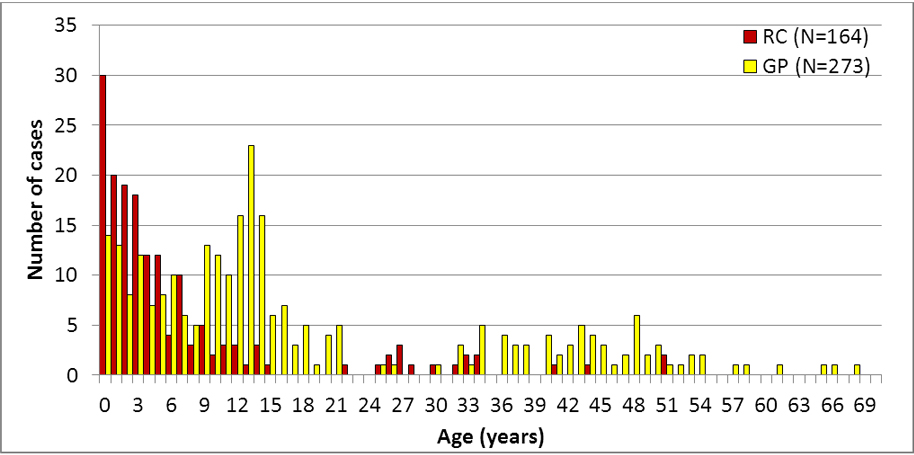
Of the 443 cases, 31.2% originated in religious community A, 7.2% in religious community B and 61.6% in the general population (Table 1). The age distribution of cases from the two religious communities was distinct from that of the general population (Figure 1). The median age of cases from the general population was approximately 10 years older and significantly higher than the median age of cases from either of the two religious communities (p < 0.001). While over half of the cases from religious community A and B were under 5 years of age, only 19.8% of the general population cases occurred in this age group (p<0.0001). Among the general population, the highest proportion of cases (28.2%) occurred in the 10-14 year age group. The probability of hospitalization did not vary by community.
| Religious community A | General population | Religious community B | |
|---|---|---|---|
| iPHIS Data (n=443) | |||
| Number of cases (%) | 138 (31.2%) | 273 (61.6%) | 32 (7.2%) |
| Median age (years) | 3.7 | 13.2 | 3.9 |
| Proportion less than 5 years old | 60.6% | 19.8% | 59.4% |
| Case Report Form Data (n=303) | |||
| Number of forms completed | 115 | 188 | 0 |
| % high risk | 22.6% | 5.3% | N/A |
| % obtaining laboratory tests | 50.9% | 81.3% | N/A |
| % initiating antibiotic therapy | 82.1% | 92.6% | N/A |
| Median interval between onset and treatment | 15.5 days | 9 days | N/A |
|
|||
Figure 1: Pertussis Cases by Age and Community Status: Ontario, November 1, 2011 to April 15, 2013 (n=437Footnote *)
Text Equivalent
This figure is a histogram with the number of cases ranging from zero to 35 on the y axis, and age in years ranging from zero to 69 on the x axis. The bars in the histograms are either dark, representing 164 cases in religious communities A and B, or light, representing 273 cases in the general population.
The highest bar in the histogram is at 30 in the 0-1 year age group from the religious communities. The number of pertussis cases in religious communities then gradually tapers off to 1 in the 15 year age group with a slight increase in the mid-twenties to mid-thirties and a few sporadic cases between 40 and 50 year olds.
In contrast, the highest bar in the histogram in the general population is at 23 in the 13 year age group, whereas only 14 cases were observed in the 0-1 year age group. The number of pertussis cases in the general population then generally tapers off to 5 in the 8 year age group followed by a rapid rise in number of cases peaking in the 13 year age group. The number of cases in the general population then generally decreases to 1 case by age 19 and up to 5 cases by age 21. There are few cases in the rest of that decade, generally 1-7 cases in the mid-thirties to the mid-fifties and then only occasional cases until the mid-sixties.
- Footnote RC
- RCreligious communities A and B
- Footnote GP
- GPgeneral population
- Footnote *
- *excludes 6 cases for whom age was unknown
Enhanced case report forms were available for 68.4% of cases; 115 from religious community A and 188 from the general population (no cases from religious community B had enhanced case report forms as they occurred later in the outbreak). As seen in Table 1, religious community A cases were more likely than general population cases to be high risk (p <0.0001), and were less likely to obtain the recommended laboratory testing for pertussis (p<0.0001), as well as initiate antibiotic therapy (p<0.01). Religious community A cases also had a longer time period between symptom onset and initiation of treatment compared to the general population cases (p<0.005).
The temporal distribution of cases showed a bimodal pattern over the course of the outbreak (Figure 2). The first wave peaked in January 2012 and was limited almost exclusively to cases from religious community A. The second wave peaked in June 2012 and was comprised primarily of cases from the general population, although the tail of the epidemic curve was mixed and involved religious community B cases.
Figure 2: Confirmed and probable outbreak cases (n=443) by onset date, case classification and community, southwestern Ontario: November 1, 2011 to April 15, 2013
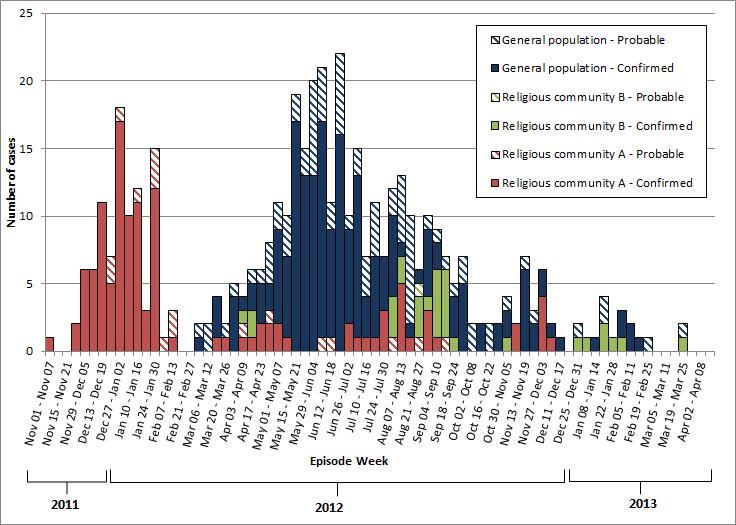
Text Equivalent
This figure is a histogram with number of cases ranging from zero to 25 on the y axis, and time by week from November 1, 2011 to April 15, 2013 on the x axis. There are six types of stacking bars in the histogram representing six types of cases: general population probable, general population confirmed, religious community A probable, religious community A confirmed, religious community B probable and religious community B confirmed.
Two waves are present. The first wave peaks at the end of December 2011, with mostly confirmed cases in religious community A and some probable cases in religious community A. The second wave peaks mid-June 2012 with mostly confirmed cases in the general population, and some probable cases in the general population. There are some confirmed and probable cases from religious community B sporadically throughout the second wave and a mix of confirmed and probable cases from religious community A mostly in the second half of the second wave.
Immunization status
We could determine immunization status for 85.1% (n=377) of cases. Of these, 34.5% were complete-for age, 11.9% were partially immunized, and 53.6% were unimmunized. Immunization status was similar between the two religious communities and we therefore combined their data for this analysis. We found a significant difference in proportion immunized and complete-for-age between the religious communities and the general population (p < 0.01). While 86.6% of cases in the two religious communities with known status were unimmunized, only 32.0% of cases in the general population were unimmunized. The age distribution of unimmunized cases varied by community. Unimmunized cases were younger in the religious communities compared to the general population (median age of 3.0 versus 8.4 years, respectively, p<.0001). Conversely, 6.0% (n=9) of cases with known immunization status were complete for age in the religious communities compared to 53.1% (n=121) among the general population (p<.0001). The median age of cases in the general population who were complete for age was 11.7 years (range 2 months to 43 years) and over half (51.2%) were between 10- 14 years. The median number of years since their last immunization was 5.6 (range 15 days to 9.9 years).
Discussion
Ontario experienced an outbreak of pertussis that lasted more than 17 months. We found that the epidemiology of pertussis in the under-immunized community was distinct from that of the general population, with a younger age distribution, a larger proportion of cases with no immunization and a larger proportion of high risk cases. The pertussis epidemiology in the under-immunized community is more consistent with that found in the developing world and similar to that seen prior to immunization programs in North America.Footnote 15 Footnote 16 Despite the younger age distribution, the disease did not appear to be more severe in the under-immunized communities. Although 86.6% of the religious community cases were unimmunized, some community members were willing to receive immunizations during specific outreach clinics held by the HUs, where testing and chemoprophylaxis were also offered.
One concern raised by public health staff arose from the observation that some religious community members declined follow-up for confirmatory laboratory testing. While cases from the religious community were less likely to have laboratory testing than cases from the general population, it was somewhat reassuring that almost half sought testing. It was also encouraging that the majority of individuals from all communities obtained treatment once they were identified as cases, although religious community cases obtained this less often. The delay in receipt of treatment by the religious community may be amenable to public health interventions.
Transmission to the general community is not unexpected during a pertussis outbreak, especially considering the infectiousness of the organism. Ontario does not have a comprehensive immunization registry, so we cannot determine immunization coverage in the general population or vaccine effectiveness. The lack of denominator information for the religious communities also precludes assessment of vaccine effectiveness using the screening method. However, Ontario has a school-based immunization information system and in 2011/2012 school year, the proportion of 7 and 17 year old Ontario students who were up to date with their pertussis immunizations was 76.0% and 67.7%, respectively.Footnote 17 This coverage is not high enough to prevent transmission of pertussis within communities, especially in regions where coverage is even lower as a result of religious or conscientious objection to immunization.
The proportion of general population cases who were fully immunized in this outbreak was concerning and has also been seen in other recent outbreaks in North America.Footnote 1 Footnote 4 In Ontario, acellular pertussis vaccine was implemented in 1997, and therefore the oldest cohort of children vaccinated solely with acellular vaccine would have been between approximately 14 and 15 years of age during this outbreak. Although children 10-14 years of age account for 5.7% of Ontario's population, they accounted for 20.4% of outbreak cases overall, 28.2% of the general population cases and 51.2% of the general population cases who were up to date with their immunizations. This warrants further investigation and is suggestive of waning immunity associated with acelluar pertussis vaccine, which has also been demonstrated in the United States.Footnote 1 Footnote 18 Footnote 19
Our analysis has a number of limitations. Accurately assessing immunization status within iPHIS is challenging for diseases such as pertussis with a complex immunization schedule. Records were frequently missing clinical information and immunization status was unknown for 14.9% of cases, despite extensive follow-up by health unit staff. These limitations were somewhat offset through the use of enhanced case report forms at the beginning of the outbreak. Given the prolonged nature of the outbreak and the human resources required to complete the report forms, they were only completed on cases occurring during the first nine and a half months of the outbreak, which may impact their representativeness. Finally, as noted above, we were not able to calculate vaccine effectiveness as we do not have a comprehensive provincial immunization registry.
Conclusion
This outbreak provided the opportunity to contrast pertussis epidemiology in distinct communities within one geographic area. Transmission from under-immunized communities to the general community is not unexpected, however the number of adolescent cases who were up to date with immunization suggests waning vaccine immunity.
Acknowledgements
The authors would like to thank all persons involved in the outbreak and outbreak response from the affected Health Units, the Ontario Ministry of Health and Long Term Care and Public Health Ontario.
Conflict of Interest
All authors have no conflicts of interest to disclose.
Funding
No external funding was secured for this study.
Financial Disclosure
All authors have no financial relationships relevant to this article to disclose.
Page details
- Date modified: