Archived - Shigella sonnei in Montréal, 2015

 Download this article as a PDF (147 KB - 5 pages)
Download this article as a PDF (147 KB - 5 pages) Published by: The Public Health Agency of Canada
Issue: Volume 42-4: Vaccine-Preventable Diseases
Date published: April 7, 2016
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 42-4, April 7, 2016: Vaccine-Preventable Diseases
Outbreak report
Outbreak of Shigella sonnei in Montréal’s ultra-Orthodox Jewish community, 2015
Pilon PA1,2*, Camara B1, Bekal S3,4
Affiliations
1 Infectious Disease and Prevention Control, Montréal Regional Public Health Department, Montréal, QC
2 School of Public Health, Université de Montréal, Montréal, QC
3 Laboratoire de santé publique du Québec, Sainte-Anne-de-Bellevue, QC
4 Department of Microbiology and Immunology, Université de Montréal, Montréal, QC
Correspondence
Suggested citation
Pilon PA, Camara B, Bekal S. Outbreak of Shigella sonnei in Montréal’s ultra-Orthodox Jewish community, 2015. Can Comm Dis Rep 2016;42:86-90. https://doi.org/10.14745/ccdr.v42i04a03
Abstract
An outbreak of Shigella sonnei that occurred in the ultra-Orthodox Jewish community (UOJC) was the subject of an investigation and response by the Montréal Regional Public Health Department, who collaborated with several health and community partners. A total of 27 confirmed cases were reported in this outbreak, which lasted from February to June 2015. The epidemic curve was compatible with a point source with secondary person-to-person transmission. In 11 of the 27 cases, pulsed-field gel electrophoresis (PFGE) analysis of strains found a single PFGE pattern newly identified in Quebec. Almost all strains tested showed resistance to ampicillin and trimethoprim-sulfamethoxazole (TMP/SMX). All the cases resided in centre west Montréal. Most of the cases were under 5 years old and attended a daycare centre, an environment recognized to be conducive to the transmission of enteric diseases. The Montréal Regional Public Health Department sent timely information to families, daycare and school stakeholders, community partners and synagogues in the UOJC, which helped reduce the transmission of shigellosis in the community.
Background
On March 25, 2015, the Montréal Regional Public Health Department detected a statistically significant space‑time cluster of 7 cases of shigellosis reported in the previous 12 days using SaTScan™ analytical software. The first epidemiologic investigations indicated that 3 of the 7 cases were children from the ultra-Orthodox Jewish community (UOJC). The other 4 cases had contracted the infection while travelling, and there were no links between them. Prior to this cluster, on February 25, there had been a report of a case in a daycare centre in this community; this child’s symptoms had begun on February 19. Based on epidemiologic and historical data, an outbreak of shigellosis in the Montréal UOJC was strongly suspected and an investigation was launched.
Meanwhile, in December 2014 Footnote 1 New York City issued a public health alert regarding an outbreak involving 43 cases of Shigella sonnei affecting two similar communities. Because members of the UOJC regularly travel between Montréal and New York, it was important to investigate a possible link between the two outbreaks. The objectives of this investigation were to further characterize the S. sonnei outbreak in the UOJC, develop hypotheses and guide the Montréal Regional Public Health Department’s potential interventions. An investigation report was written to share intervention strategies and to serve as a reference document for similar investigations.
Methodology
Case definition
A case was defined as a Montréal resident belonging to the UOJC, with no history of recent travel abroad and with a laboratory confirmation of S. sonnei infection, reported to the Montréal Regional Public Health Department between January 1 and August 31, 2015.
Case finding and data collection
Cases were identified through Quebec’s registry of notifiable diseases. Data were collected through the registry and then by examining case files from the epidemiologic survey. Cases were assigned to the UOJC or an orthodox group (e.g., Belz, Satmar, etc.) based on survey responses.
Laboratory tests
Laboratory tests were performed in the medical microbiology laboratories of reporting hospitals (identification of genus and species and sensitivity profile). Identification was confirmed using pulsed-field gel electrophoresis (PFGE) at the Laboratoire de santé publique du Québec (LSPQ).
Epidemiologic analysis
A case list was generated and imported into Microsoft Excel 2010; the list included demographic, clinical and epidemiologic variables. Descriptive analyses were conducted using SPSS version 12.0.2.
Public health intervention
A survey was conducted with each family that had a reported case. Information on prevention was provided to the family and the appropriate daycare centre or school. Public health officials worked with two partners within the UOJC to inform community members through synagogues, daycare centres and schools and to strengthen hygiene practices.
Health system partners and the Laboratoire de santé publique du Québec were informed to increase vigilance among health professionals and enhance surveillance and to obtain confirmatory test results and characterization results from the laboratory.
Results
Case description based on time
Between February 19 and June 1, 2015, 27 confirmed cases of S. sonnei (contracted locally) occurred in the Montréal UOJC. This represented 79% (27/34) of all confirmed cases of S. sonnei reported in the area for the same period. The first case was observed on February 19, and the outbreak lasted five months. The peak occurred in May with 10 (about 37%) reported cases. This was followed by a decrease in June until there were no cases in July and August. Based on the 1- to 3-day incubation period, the case exposure period seems to have been between February 18 and May 28, 2015. The epidemic curve (Figure 1) was consistent with a point source with secondary person-to-person transmission.
Figure 1: Epidemic curve of the Shigella sonnei outbreak in the ultra‑Orthodox Jewish community, Montréal area, February to June 2015 Figure 1 footnote 1

Text description: Figure 1
Figure 1: Epidemic curve of the Shigella sonnei outbreak in the ultra‑Orthodox Jewish community, Montréal area, February to June 2015 Figure 1 footnote 1
| Week (symptom onset) (Sampling week if missing, N = 4 ) |
Pulsotype 148 | Unknown | Total |
|---|---|---|---|
| 31-Dec-14 | 0 | 0 | 0 |
| 07-Jan-15 | 0 | 0 | 0 |
| 11-Jan-15 | 0 | 0 | 0 |
| 18-Jan-15 | 0 | 0 | 0 |
| 25-Jan-15 | 0 | 0 | 0 |
| 01-Feb-15 | 0 | 0 | 0 |
| 08-Feb-15 | 0 | 0 | 0 |
| 15-Feb-15 | 0 | 1 | 1 |
| 22-Feb-15 | 0 | 0 | 0 |
| 01-Mar-15 | 1 | 0 | 1 |
| 08-Mar-15 | 2 | 0 | 2 |
| 15-Mar-15 | 0 | 0 | 0 |
| 22-Mar-15 | 0 | 0 | 0 |
| 29-Mar-15 | 2 | 2 | 4 |
| 05-Apr-15 | 3 | 1 | 4 |
| 12-Apr-15 | 1 | 0 | 1 |
| 19-Apr-15 | 1 | 0 | 1 |
| 26-Apr-15 | 1 | 0 | 1 |
| 03-May-15 | 0 | 3 | 3 |
| 10-May-15 | 0 | 5 | 5 |
| 17-May-15 | 0 | 2 | 2 |
| 24-May-15 | 0 | 0 | 0 |
| 31-May-15 | 0 | 2 | 2 |
| 07-Jun-15 | 0 | 0 | 0 |
| 14-Jun-15 | 0 | 0 | 0 |
| 21-Jun-15 | 0 | 0 | 0 |
| 28-Jun-15 | 0 | 0 | 0 |
| 05-Jul-15 | 0 | 0 | 0 |
| 12-Jul-15 | 0 | 0 | 0 |
| 19-Jul-15 | 0 | 0 | 0 |
| 26-Jul-15 | 0 | 0 | 0 |
| 02-Aug-15 | 0 | 0 | 0 |
| 09-Aug-15 | 0 | 0 | 0 |
| 16-Aug-15 | 0 | 0 | 0 |
| 23-Aug-15 | 0 | 0 | 0 |
| 30-Aug-15 | 0 | 0 | 0 |
| 06-Sep-15 | - | - | - |
| 13-Sep-15 | - | - | - |
| 20-Sep-15 | - | - | - |
| 27-Sep-15 | - | - | - |
| 04-Oct-15 | - | - | - |
| 11-Oct-15 | - | - | - |
| 18-Oct-15 | - | - | - |
| 25-Oct-15 | - | - | - |
| 01-Nov-15 | - | - | - |
| 08-Nov-15 | - | - | - |
| 15-Nov-15 | - | - | - |
| 22-Nov-15 | - | - | - |
| 29-Nov-15 | - | - | - |
| 06-Dec-15 | - | - | - |
| 13-Dec-15 | - | - | - |
| 20-Dec-15 | - | - | - |
| 27-Dec-15 | - | - | - |
| - | 11 | 16 | 27 |
Case description based on environment
All the cases resided in centre west Montréal. Of the 27 cases, 11 lived within the same postal code. The environments frequented by 23 of the 27 cases during their infectious period were known: 8 daycare facilities for 13 cases (57%), 3 primary schools for 5 cases (22%), their homes for 4 cases (17%) and a university for 1 case (4%). A daycare and a school had the highest incidence with 3 cases each.
Description of case characteristics
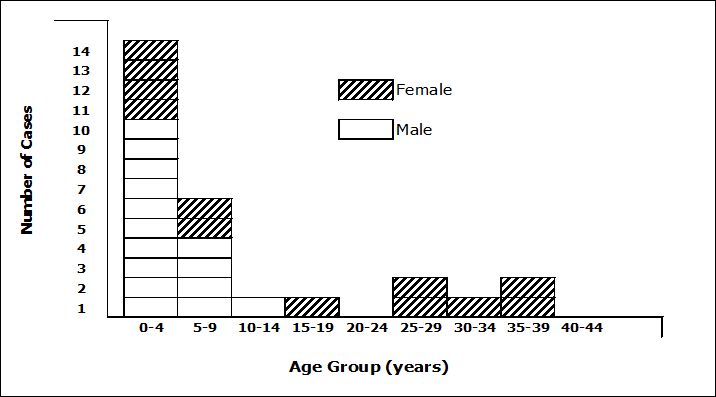
Ages ranged from 1 to 35 years; the average age was 10 years, and the median age 4 years. Most (74%) of the cases were aged less than 10 years and 52% aged less than 5 years) [Figure 2].
There were 15 (56%) males and 12 (44%) females, a 1:3 M/F ratio. It is interesting to note that all the reported adult cases were women, probably because women are more involved in childcare.
Figure 2: Number of cases of Shigella sonnei in the ultra-Orthodox Jewish community, by age group and sex, Montréal area, February to June 2015
Text description: Figure 2
Figure 2: Number of cases of Shigella sonnei in the ultra-Orthodox Jewish community, by age group and sex, Montréal area, February to June 2015
| Age Group (years) |
Sex | Total | Percentage | |
|---|---|---|---|---|
| Female | Male | |||
| 0 to 4 | 4 | 10 | 14 | 51.9 |
| 5 to 9 | 2 | 4 | 6 | 22.2 |
| 10 to 14 | 0 | 1 | 1 | 3.7 |
| 15 to 19 | 1 | 0 | 1 | 3.7 |
| 20 to 24 | 0 | 0 | 0 | 0 |
| 25 to 29 | 2 | 0 | 2 | 7.4 |
| 30 to 34 | 1 | 0 | 1 | 3.7 |
| 35 to 39 | 2 | 0 | 2 | 7.4 |
| 40 to 44 | 0 | 0 | 0 | 0 |
| Total | 12 | 15 | 27 | 100 |
Clinical presentation
Information on signs and symptoms was obtained for 22 of the 27 cases (Table 1). Fever and lower gastrointestinal symptoms were the most common symptoms. Fever and blood in the stool, indicating a more serious illness, occurred in 55% of the cases.
| Clinical presentation | 0–9 years N=15 (%) |
10–39 years N=7 (%) |
All ages N=22 (%) |
|---|---|---|---|
| Diarrhea | 15 (100) | 7 (100) | 22 (100) |
| Cramps / abdominal pain | 14 (93) | 5 (71) | 19 (86) |
| Fever (≥38 °C) | 13 (86) | 5 (71) | 18 (82) |
| Blood in the stool | 10 (67) | 3 (43) | 13 (59) |
| Unusual tiredness | 9 (60) | 3 (43) | 12 (55) |
| Nausea | 7 (47) | 4 (57) | 11 (50) |
| Vomiting | 8 (53) | 1 (14) | 9 (41) |
Medical consultation and hospitalization
The first contact with the health care system took place at an outpatient clinic for 24 cases (89%), and at a hospital emergency room for 3 cases (11%). Of the 24 cases who sought medical advice at a clinic, 18 (75%) reported to the same clinic, which appears to serve the UOJC.
None of the 27 cases had been hospitalized or had died at the time of the survey.
Treatment
Of the 25 cases who provided information on treatment, 17 (68%) received antibiotics; of these, 9 (53%) received ciprofloxacin. One case received ampicillin despite the strain’s resistance profile (Table 2).
| Antibiotic treatment | Number (%) Table 2 - Footnote 1 |
|---|---|
| Ciprofloxacin | 9 (53) |
| Azithromycin | 2 (12) |
| Cefixime | 2 (12) |
| Cephalexin | 1 (6) |
| Ampicillin | 1 (6) |
| Unknown | 2 (12) |
| Total | 17(100) |
Laboratory results
All cases were laboratory confirmed by stool culture. Antibiotic sensitivity test results were available for 24 of the 27 cases; all were resistant to ampicillin and trimethoprim-sulfamethoxazole (TMP/SMX) [Table 3]. In all but 2 cases (1 ciprofloxacin and 1 cefixime), we had no data on sensitivity to these antibiotics or to azithromycin. The PFGE was performed in 11 of 27 cases, and a single genetic profile, pulsotype 148, was highlighted. This pulsotype, not previously identified in Quebec, was different from the PFGE pattern of the strain that caused an outbreak in the New York area in December 2014.
| Resistance profile | Number (%) |
|---|---|
| Ampicillin (R) + TMP/SMX (R) | 16 (67) |
| Ampicillin (R) + TMP/SMX (I) | 6 (25) |
| Ampicillin (R) | 1 (4) |
| TMP/SMX (I) | 1 (4) |
| Total | 24 (100) |
Potential sources of exposure
Of the 27 cases, 5 had a family relationship with another confirmed case already reported to the Montréal Regional Public Health Department. Of the 27 cases, 8 reported having had contact with a case with diarrhea before the start of their illness (including 3 contacts of confirmed cases). In 4 cases, the contact was with a family member, and for the 4 other cases, the only contact was via a daycare centre or primary school. The index case was a 2-year-old boy who attended a daycare centre (name not indicated), and whose symptoms began in February. Three members of his family also had diarrhea (unknown time sequence), but neither he nor anyone in his family had travelled recently. The 5 cases that followed in March (4 of which had identical pulsotypes) were also children aged between 4 and 10 years attending primary schools or different daycare centres, but did not seem to have any clear link to the index case. However, they were all of a similar age and could have participated in a common activity within the UOJC, giving rise to transmission. Of the cases that occurred in April and June, some were siblings of earlier cases and were probably infected through intrafamily transmission. One transmission may have also occurred in two daycare centres (DCC A and DCC B) and a primary school (primary school A) [initial case followed by other cases soon after] (Table 4).
| Exposure site | Name of site | Number of cases |
|---|---|---|
| Daycare centre (N=13) | DCC A | 3 |
| DCC B | 2 | |
| DCC C (girls) | 1 | |
| DCC D (boys) | 1 | |
| DCC E | 1 | |
| DCC F | 1 | |
| Daycare G (girls) | 1 | |
| Daycare H | 1 | |
| Unknown | 2 | |
| Primary school (N= 5) | A (boys) | 3 |
| B (girls) | 1 | |
| C (girls) | 1 | |
| University (N=1) | A | 1 |
| Other (N=8) | Residence | 4 |
| Unknown | 4 | |
Public health intervention
In this investigation, there was a response to each reported case of shigellosis confirmed by the laboratory. The response involved waiting at least 48 hours after cessation of diarrhea before sending the child back to daycare or school. In addition, an information sheet on the prevention of shigellosis was sent to the parents of affected children as well as the schools and daycares to increase the vigilance of other parents and officials in the various settings and to strengthen preventive measures.
Discussion
Shigellosis outbreaks are cyclical within the UOJC in Montréal, having occurred at different intensities at approximately 1- to 5-year intervals (Table 5) Footnote 2Footnote 3Footnote 4Footnote 5Footnote 6Footnote 7Footnote 8Footnote 9. The regular recurrence of shigellosis in the UOJC is caused by the spread of the infectious agent as a result of travel to other similar communities with high prevalence of the disease or through chronic carriers who serve as a reservoir Footnote 2Footnote 5Footnote 10. The periodicity of Shigella outbreaks in the UOJC may be due to persistent low endemicity that generates an outbreak when a new cohort of young children with no previous shigellosis enters daycare or school Footnote 3.
| Period | Number of confirmed cases |
|---|---|
| February and June 2015 | 27 (pulsotype 148) |
| August 2011 to December 2012 (8) | 38 (several pulsotypes) |
| November 2007 to January 2008 (7) | 11 (pulsotype 35 and related pulsotypes) |
| October 2004 to July 2005 (6,7) | 76 |
| July 1997 and January 1998 (6,7) | 100 |
| 1994 to 1996 (2) | 34 (pulsotypes 3, 3A) |
The spread of shigellosis in this outbreak was caused by intrafamily transmission (4 of the 27 confirmed cases were siblings and several other cases had contact with family members suffering from diarrhea) and transmission at daycare centres (13 of the 27 cases) and school (5 of the 27 cases were connected to a primary school). Having close contacts, attending daycare, and having several young children at home were considered risk factors in previously reported outbreaks Footnote 3Footnote 5. The space‑time cluster of cases and diversity of environments suggested person-to-person transmission. The fact that cases occurred in several groups within the UOJC supported the argument that community environments (in addition to the family environment) played a role in transmission. The characteristics of the Montréal outbreak were similar to those described in other cities Footnote 2Footnote 3Footnote 4Footnote 5. Undeveloped hygiene habits in young children and the low infectious dose required to transmit S. sonnei diminish the effectiveness of preventive measures in this population Footnote 3.
In the wake of outbreaks in recent years in Montréal, efforts had been made to try to reach different groups within the UOJC to prevent transmission of infectious diseases and, in particular, transmission of enteric diseases. As a result of these efforts, close ties were established with two Jewish community organizations who deal with various groups in Montréal’s UOJC. Through them, preventive messages from the Montréal Regional Public Health Department were sent to those groups who have limited contact with anyone outside their community.
As soon as the outbreak was suspected, these two Jewish community organizations were notified and provided with the relevant information. The first organization has a medical clinic, a Yiddish telephone information line available to over 2,000 Jewish families, especially ultra-Orthodox groups, and contact with the synagogues; the second organization had counsellors in the community (daycare centre and schools). Both organizations participated in the Montréal Regional Public Health Department’s effort to provide timely information on the unfolding shigellosis outbreak and the steps to prevent and control the transmission of this disease. Posters in French, English and Yiddish on handwashing were sent to families, daycare centres, schools and community partners in the UOJC to educate children and their parents and people working at daycare centres and schools. We assume that this timely information on preventive measures could help reduce the transmission of shigellosis. While the outbreak appeared to persist after March 25, preventive messages sent to the UOJC reduced the extent of the outbreak.
The decrease in the number of cases in the epidemic curve between April 5 and May 3 could be related to Passover celebration that took place from April 3 to 11. The closing of daycare centres and schools during this period reduced transmission.
Strains of S. sonnei from confirmed cases showed resistance to the first-line antimicrobials, ampicillin and TMP/SMX, which was considered a serious threat in the United States by the Centers for Disease Control and Prevention Footnote 11. This led clinicians to make more extensive use of antimicrobials such as ciprofloxacin or azithromycin, although some infections were already reported to be resistant to both these antibiotics.
The PFGE pattern of strain isolated in this investigation (pulsotype 148) showed that it had been previously unreported in Quebec and different from the strain responsible for the New York outbreak. Since strains of Shigella do not undergo routine laboratory monitoring, the possibility that this strain has been circulating for some time in Montréal or in other areas cannot be ruled out. Laboratory monitoring of Shigella strains could certainly facilitate epidemiologic surveillance in certain risk groups.
This investigation has several limitations. Only cases confirmed by laboratory analysis are identified in this report. The information collected during case finding suggests that the number of reported cases is lower than the true number of cases. Some cases of diarrhea that occurred in several families may have not been confirmed or reported to the Montréal Regional Public Health Department. Although intrafamily and community transmission in daycare centres and schools is strongly suspected, the probable source of exposure was unknown for a number of cases at the time of the survey.
Conclusion
This investigation describes an outbreak of S. sonnei in Montréal’s UOJC that mainly affected preschool- and school-aged children. Identifying person-to-person transmission in a community that has limited contact with outsiders highlights the importance of maintaining and consolidating ties with UOJC partners to prevent outbreaks and respond quickly if they do occur. With these partners, it is possible to work with adults (parents, educators and teachers) to promote and strengthen preventive measures demonstrated to be effective in the prevention and control of infectious disease and, in particular, Shigella outbreaks (e.g. supervising children while they wash their hands, decontaminating toys or other shared objects, temporarily keeping children with diarrhea out of daycare centres and schools).
Acknowledgements
We would like to thank all the investigators who worked on the cases and dealt with families and communities; the managers and stakeholders from the two Jewish community organizations for their work with the UOJC; Dr. Sandra Palmieri, Dr. Robert Allard, Maryse Lapierre and Dr. Carole Morissette for their comments.
Conflict of interest
None.