Archived - Salmonella Reading outbreak in Canada, 2014–2015

 Download this article as a PDF (551 KB - 7 pages)
Download this article as a PDF (551 KB - 7 pages) Published by: The Public Health Agency of Canada
Issue: Volume 43-1: Enteric disease outbreaks
Date published: January 5, 2017
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 43-1, January 5, 2017: Enteric disease outbreaks
Outbreak report
Outbreak of Salmonella Reading in persons of Eastern Mediterranean origin in Canada, 2014–2015
F Tanguay1*, L Vrbova2, M Anderson3, Y Whitfield4, L Macdonald4,5, L Tschetter6, A Hexemer2 for the Salmonella Reading Investigation Team7
Affiliations
1 Centre for Food-borne, Environmental and Zoonotic Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
2 Centre for Food-borne, Environmental and Zoonotic Infectious Diseases, Public Health Agency of Canada, Guelph, ON
3 Centre for Public Health Infrastructure, Public Health Agency of Canada, Ottawa, ON
4 Public Health Ontario, Toronto, ON
5 Dalla Lana School of Public Health, University of Toronto, Toronto, ON
6 National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, MB
7 See acknowledgements
Correspondence
Suggested citation
Tanguay F, Vrbova L, Anderson M, Whitfield Y, Macdonald L, Tschetter L, et al. Outbreak of Salmonella Reading in persons of Eastern Mediterranean origin in Canada, 2014–2015. Can Commun Dis Rep. 2017;43(1):14-20. https://doi.org/10.14745/ccdr.v43i01a03
Abstract
Background: Salmonella Reading (S. Reading) is a rare serotype of Salmonella subspecies (spp.) in Canada with less than nine cases reported each year (2011–2013). An increase in S. Reading was identified in several Canadian provinces in early 2015, prompting the initiation of a national outbreak investigation.
Objectives: To describe a multi-provincial S. Reading outbreak in Canada that affected over 30 people.
Methods: Cases were defined as laboratory-confirmed S. Reading with related pulsed-field gel electrophoresis (PFGE) patterns. Onset dates were between November 2014 and September 2015.
Early in the investigation, investigators noted cases were predominantly of Eastern Mediterranean origin, mainly Afghan and Lebanese and many of those affected had consumed food items not typically captured on standard enteric outbreak hypothesis-generating questionnaires. An open-ended three day food consumption survey was conducted with a convenience sample of community informants to better understand food preferences of the affected ethnocultural populations. Results of the survey were used to design a focused questionnaire for case re-interviews and subsequent outbreak cases. Public health investigators obtained food samples from case homes and relevant food premises. Food safety authorities conducted traceback of suspected food items and collected food samples for laboratory testing.
Results: There were 31 confirmed cases (Ontario=23, Alberta=7, New Brunswick=1) and three probable (Ontario=2, Alberta=1) cases of S. Reading identified as part of the outbreak. The median age was 31 years (range less than one to 85 years) and 53% (18/34) of cases were female. Seven cases were hospitalized. No deaths were reported. Most cases were of Eastern Mediterranean origin (n=23) or had reported consuming Eastern Mediterranean foods (n=3). The predominant ethnic origins reported by cases were Afghan in Ontario (n=12) and Lebanese in Alberta (n=3). Genetic similarity of clinical isolates was further confirmed using whole genome sequencing.
Three ethnic bakeries were identified as possible common exposures for the cases; however, traceback of foods of interest from these bakeries did not identify a common supplier and the source of the illness was not identified. In total, 227 food samples from retail premises (n=142), restaurants (n=13) and case homes (n=72) were tested; two food samples, kalonji seeds and tahini, were positive for S. Ruiru and S. Meleagridis. These products were recalled from the marketplace.
Conclusion: Despite extensive epidemiological, microbiological and food traceback investigations, a common source was not identified for this S. Reading outbreak. Challenges included lack of familiarity with the food items consumed in affected ethnocultural groups, as well as a lack of background data on expected food exposures in the outbreak population. Engaging local partners helped build understanding of food preferences in affected communities. Given Canada's ethnic and cultural diversity, culturally competent approaches to enteric outbreak investigations and food consumption surveys may be useful.
Introduction
Salmonellosis is one of the most common causes of food-borne outbreaks and typically results in diarrhea, fever and abdominal pain. The most common species of this gram-negative bacteria is S. enterica and this is further divided into six subspecies and many serotypes (or serovars). S. Reading is a rare serotype in Canada: there were seven cases reported in 2012 to the National Enteric Surveillance Program (NESP) and nine cases reported in 2013 Footnote 1Footnote 2. The NESP is a laboratory-based surveillance system that provides weekly analysis and reporting for laboratory-confirmed cases of enteric pathogens in Canada. The objective of this article is to describe a multi-provincial S. Reading outbreak in Canada that affected over 30 people.
Outbreak detection
On January 21, 2015, the NESP identified an increase in reported cases of S. Reading in Alberta (n=2) and British Columbia (n=2). One week later, on January 27, 2015, the NESP identified an increase in S. Reading in Ontario (n=4). Public Health Ontario opened an Ontario outbreak investigation on February 4, 2015. As additional cases began to occur in Alberta, a national outbreak investigation coordinating committee was activated as per Canada's Foodborne Illness Outbreak Response Protocol (FIORP) Footnote 3.
Methods
Case findings
Cases were identified between January 21 and August 25, 2015. The case definitions used during this investigation were:
| Confirmed | A resident of or visitor to Canada with:
|
|---|---|
| Probable | A resident of or visitor to Canada with:
|
Questionnaires and exposures
Initial public health investigations were conducted by public health units for all salmonellosis cases, as per routine practice. Outbreak case questionnaires were collected and centrally analyzed by the investigation team where available. Until May 4, 2015, available cases were re-interviewed using a standardized hypothesis-generating questionnaire. Interviews focused on foods identified during initial case follow up and thought to be frequently consumed by individuals of Eastern Mediterranean origin (see definition below). These included sesame seeds, tahini, pistachios and black (onion/nigella/kalonji) seeds. Supplementary questions were developed to identify a possible link between cases in Alberta and Ontario (e.g. a visitor from Ontario and/or food brought directly from Ontario to Alberta).
In May 2015, field epidemiologists were deployed to assist the investigation team and to collaborate with local public health units and community partners as they conducted an open-ended, detailed three day food consumption survey. Participants were made up of convenience samples of populations affected by the outbreak to identify additional food items typically consumed. In-person interviews were conducted, using approaches that aimed to respect cultural differences and adapt services to meet unique needs within the identified culture Footnote 4Footnote 5. In Alberta, an environmental health officer fluent in Arabic participated in case interviews and three day food consumption surveys and cases were re-interviewed in their homes. In Ontario, volunteers from the affected groups (community informants) were interviewed in community-based settings (e.g. community centres). Findings of the three day food consumption survey informed the development of a focused questionnaire.
Case ethnicity was self-reported in interviews and/or estimated from reported food exposures. For this investigation, Eastern Mediterranean backgrounds were defined as per the World Health Organization's as individuals who identified their ethnicity as linked to countries in the Eastern Mediterranean region: i.e. Afghanistan, Bahrain, Djibouti, Egypt, Iran (Islamic Republic of), Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Pakistan, Qatar, Saudi Arabia, Somalia, Sudan, Syrian Arab Republic, Tunisia, United Arab Emirates and Yemen Footnote 6.
Laboratory investigation
Pulsed-field gel electrophoresis (PFGE) was done on all S. Reading isolates. A request was then sent to PulseNet USA and PulseNet International to find PFGE matches to this cluster. An EPIS (European Centre for Disease Control's [ECDC] Epidemic Intelligence Information System) notification was used to inquire whether any PFGE matches to the isolates in this cluster had been reported to the ECDC. Whole genome sequencing (WGS) was conducted for cases and select background isolates. A maximum-likelihood phylogenetic tree, generated through the use of the SNV Phyl Pipeline developed by the Bioinformatics Unit of the National Microbiology Laboratory, was used to determine the level of relatedness among isolates based on single nucleotide variant positions (SNVs). SNV Phyl phylogeny was built using 642 hqSNVs identified across 93% of the reference genome (SPAdes assembled genome of isolate 15-0793).
Food safety investigation
Food premises (retail and restaurants) of interest were identified from case interviews. The food safety investigation focused initially on products containing sesame seeds, kalonji seeds and tahini. Halal beef, spices and pistachios were also investigated.
Local public health units in Alberta and Ontario (in partnership with regional Canadian Food Inspection Agency [CFIA] staff) visited the case homes and food premises (restaurants and retail) identified by cases in interviews. For food premises, review of handling practices for relevant food items was conducted using a modified Hazard Analysis Critical Control Point (HACCP) approach. Samples were taken from food premises and case homes for testing at Alberta Provincial and Public Health Ontario laboratories. A list of suppliers was obtained from establishments and common suppliers were identified. Product distribution information was also collected for bakery products from retail food premises of interest.
Supplier and distributor information for sesame seeds, onion/kalonji seeds, tahini, pistachios, Halal chicken and Halal beef was collected by the CFIA from Ontario and Alberta food premises reported by cases. In addition, the CFIA collected supplier information from two ethnic bakeries identified by cases in Ontario and Alberta.
Results
Descriptive epidemiology
There were 31 confirmed (ON=23, AB=7, NB=1) and three probable (ON=2, AB=1) cases included in this investigation. Illness onset dates ranged from November 7, 2014 to July 24, 2015 (see Figure 1). The median age was 31 years (range less than one to 85 years), 53% (18/34) of cases were female. Seven cases were hospitalized. No deaths were reported.
Figure 1: Confirmed and probable Salmonella Reading outbreak cases by week of illness onset and province, Canada, November 1, 2014 to September 11, 2015 (n=34)
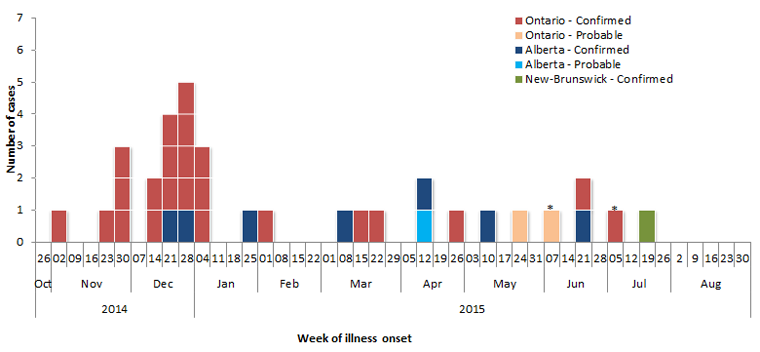
Text description: Figure 1
Figure 1: Confirmed and probable Salmonella Reading outbreak cases by week of illness onset and province, Canada, November 1, 2014 to September 11, 2015 (n=34)
| Week of illness onset | Number of cases | ||||||
|---|---|---|---|---|---|---|---|
| Year | Month | Day | Alberta - Confirmed | Alberta - Probable | Ontario - Confirmed | Ontario - Probable | New-Brunswick - Confirmed |
| 2014 | Oct | 26 | - | - | - | - | - |
| Nov | 02 | - | - | 1 | - | - | |
| 09 | - | - | - | - | - | ||
| 16 | - | - | - | - | - | ||
| 23 | - | - | 1 | - | - | ||
| 30 | - | - | 3 | - | - | ||
| Dec | 07 | - | - | - | - | - | |
| 14 | - | - | 2 | - | - | ||
| 21 | 1 | - | 3 | - | - | ||
| 28 | 1 | - | 4 | - | - | ||
| 2015 | Jan | 04 | - | - | 3 | - | - |
| 11 | - | - | - | - | - | ||
| 18 | - | - | - | - | - | ||
| 25 | 1 | - | - | - | - | ||
| Feb | 01 | - | - | 1 | - | - | |
| 08 | - | - | - | - | - | ||
| 15 | - | - | - | - | - | ||
| 22 | - | - | - | - | - | ||
| Mar | 01 | - | - | - | - | - | |
| 08 | 1 | - | - | - | - | ||
| 15 | - | - | 1 | - | - | ||
| 22 | - | - | 1 | - | - | ||
| 29 | - | - | - | - | - | ||
| Apr | 05 | - | - | - | - | - | |
| 12 | 1 | 1 | - | - | - | ||
| 19 | - | - | - | - | - | ||
| 26 | - | - | 1 | - | - | ||
| May | 03 | - | - | - | - | - | |
| 10 | 1 | - | - | - | - | ||
| 17 | - | - | - | - | - | ||
| 24 | - | - | - | 1 | - | ||
| 31 | - | - | - | - | - | ||
| Jun | 07 | - | - | - | 1 | - | |
| 14 | - | - | - | - | - | ||
| 21 | 1 | - | 1 | - | - | ||
| 28 | - | - | - | - | - | ||
| Jul | 05 | - | - | 1 | - | - | |
| 12 | - | - | - | - | - | ||
| 19 | - | - | - | - | 1 | ||
| 26 | - | - | - | - | - | ||
| Aug | 2 | - | - | - | - | - | |
| 9 | - | - | - | - | - | ||
| 16 | - | - | - | - | - | ||
| 23 | - | - | - | - | - | ||
| 30 | - | - | - | - | - | ||
| Sept | 6 | - | - | - | - | - | |
Most cases reported being of Eastern Mediterranean origin (n=23) or consuming Eastern Mediterranean foods (n=3). The predominant ethnic origins among cases were Afghan (n=12) in Ontario and Lebanese (n=3) in Alberta (Figure 2). The New Brunswick case reported travel to Ontario during the exposure period.
Figure 2: Outbreak-related Salmonella Reading cases by ethnic origin and province, Canada, November 1, 2014 to September 11, 2015 (n=34)
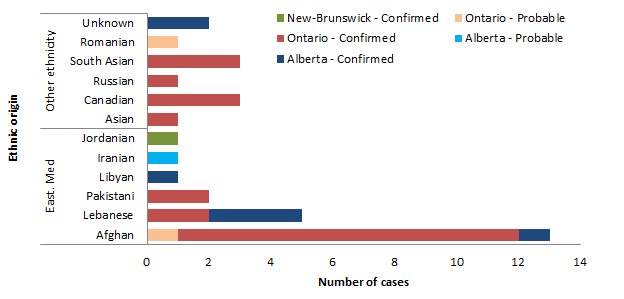
Text description: Figure 2
Figure 2: Outbreak-related Salmonella Reading cases by ethnic origin and province, Canada, November 1, 2014 to September 11, 2015 (n=34)
| Ethnic origin | Ethnicity | Ontario - Confirmed | Ontario - Probable | Alberta - Confirmed | Alberta - Probable | New-Brunswick - Confirmed |
|---|---|---|---|---|---|---|
| East. Med | Afghan | 11 | 1 | 1 | - | - |
| Lebanese | 2 | - | 3 | - | - | |
| Pakistani | 2 | - | - | - | - | |
| Libyan | - | - | 1 | - | - | |
| Iranian | - | - | - | 1 | - | |
| Jordanian | - | - | - | - | 1 | |
| Other ethnicity | Asian | 1 | - | - | - | - |
| Canadian | 3 | - | - | - | - | |
| Russian | 1 | - | - | - | - | |
| South Asian | 3 | - | - | - | - | |
| Romanian | - | 1 | - | - | - | |
| Unknown | - | - | 2 | - | - |
Laboratory findings
The three PFGE combinations in the outbreak (ReadXI.0011/ReadBNI.0005, ReadXAI.0012/ReadBNI.0005 and ReadXAI.0014/ReadBNI.0005) were highly similar and were considered genetically identical through WGS analysis (Figure 3). None of the three PFGE pattern combinations had previously been identified in Canada, USA, Caribbean or Central and South America.
The PFGE pattern combinations ReadXAI.0015/ ReadBNI.0007 (n=1) and ReadXAI.0018/ ReadBNI.0010 (n=2) were both new pattern combinations that were not considered closely related to the patterns associated with confirmed cases; cases with these patterns were included in the outbreak investigation as probable cases based on their exposure to Eastern Mediterranean food. These isolates were not included in the WGS.
Figure 3: Whole Genome sequencing (WGS) for S. Reading cases, National Microbiology Laboratory -Public Health Genomics Unit, December 10, 2015
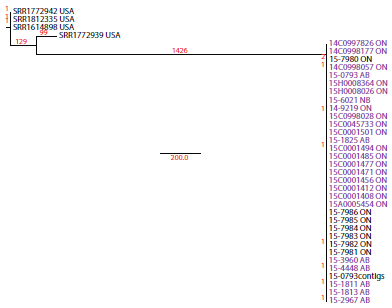
Text description: Figure 3
Figure 3: Whole Genome sequencing (WGS) for S. Reading cases, National Microbiology Laboratory -Public Health Genomics Unit, December 10, 2015
This Figure is a phylogenetic tree of a Salmonella Reading outbreak with sequencing date from 37 isolates. It shows the Canadian isolates originated predominately from Ontario, but also from Alberta and News Brunswick, and were grouped together within in a single clade. The 37 isolates were identified as: SRR1772942 USA, SRR1812335 USA, SRR1614898 USA, SRR1772939 USA, 14C0997826 ON, 14C0998177 ON, 15–7980 ON, 14C0998057 ON, 15–0793 AB, 15H0008364 ON, 15H0008026 ON, 15–6021 NB, 14–9219 ON, 15C0998028 ON,15C0045733 ON, 15C0001501 ON, 15–1825 AB, 15C0001494 ON, 15C0001485 ON, 15C0001477 ON, 15C0001471 ON, 15C0001456 ON,15C0001412 ON, 15C0001408 ON, 15A0005454 ON, 15-7986 ON, 15-7985 ON, 15–7984 ON, 15-7983 ON, 15-7982 ON, 157981 ON, 15-3960 AB, 15-4448 AB, 15-0793contigs, 15-1811 AB, 15-1813 AB, 15-2967 AB
Exposure history
Food items reported most frequently among cases were bread (27/27, 100%), chicken and Halal chicken (23/26, 88% and 15/16, 94% respectively), black pepper (12/12, 100%), Halal beef (13/16, 81%) and pita bread (10/11, 91%). Turmeric (10/13, 77%), dried fruits (13/19, 68%), sesame seeds (14/24, 58%) and pistachios (12/21, 57%) were also reported at a higher frequency but no specific commonalities between the cases were noted.
Given the shape of the epidemic curve and the long range in case onset dates, the investigation focused on the hypothesis that a shelf stable food item was the potential source of the outbreak. Initially, sesame seeds, tahini, kalonji/black seeds and Eastern Mediterranean baked goods ('sweets'), including ingredients/toppings on sweets, such as pistachios, were suspect food items and hypothesized as potential outbreak sources. Following re-interview of Alberta cases, as well as data collected from open-ended food histories with members of the affected community, Halal beef was also hypothesized as a common source of exposure.
In some instances, cases were reluctant to provide information on foods eaten in the three days prior to illness onset. Open-ended interviews with community key informants of Eastern Mediterranean origin in both Ontario and Alberta uncovered recurring themes that suggest potential barriers to eliciting this information (see Text Box).
Qualitative exposure history findings: Potential barriers to collecting three day food exposure information:
- Language was viewed as a common barrier by both interviewers and respondents.
- Multiple names for the same food/dish: Uncertainty or lack of familiarity among investigators, which was mitigated by help from an interpreter.
- Questions using unclear terms: Uncertainty among some respondents about what foods/dishes were considered 'typical' or 'Eastern Mediterranean'.
- Perceived lack of trust of government officials among some newcomers when asked about foods recently consumed, cooking practices or sampling foods/spices from home kitchens.
- Gender: Gendered food preparation roles may have resulted in challenges eliciting information from males in households where females typically prepared food.
- Positive response bias: Some respondents may have provided public health investigators with socially desirable responses to questions about food preparation which did not reflect actual practice, such as cooking meat thoroughly versus eating raw meat.
Food safety investigation
Food samples for laboratory testing were obtained from case homes, restaurants and retail food premises. In total, over 200 samples were tested by the CFIA, Public Health Ontario and Alberta provincial laboratories for presence of Salmonella spp. A summary of food samples collected and microbiologic results is provided in Table 1. One sample of tahini sauce tested positive for Salmonella Ruiru (recalled on February 26, 2014) and one sample of kalonji whole seeds tested positive for Salmonella Meleagridis (recalled on March 1, 2015).
| Sampling location | Foods sampled | Number of samples | Results of microbiologic testing for Salmonella spp. |
|---|---|---|---|
| Tested by the Ontario Provincial Laboratory | |||
| ON case homes | Spices, seeds (sesame, kalonji, etc.), bulgar, pistachios, dried fruits and other products | 49 | Not detected |
| ON restaurants | Fatoush salad ingredients, dressings and various seeds used as garnish | 13 | Not detected |
| ON retail samples | Rot, cookies, various seeds, tahini, spices and other retail food products | 27 | Not detected |
| Tested by the Alberta provincial laboratories | |||
| AB case homes | Tahini, chicken breasts, kishk and various spices | 21 | Not detected |
| AB retail samples | Halva, pistachios, raw Halal beef and spices | 5 | Not detected |
| Tested by the Canadian Food Inspection Agency | |||
| ON retail samples | Seeds (sesame, kalonji, etc.) and tahini products | 40 | Not detected in 39 samples S. Meleagridis identified in a kalonji whole seeds sample |
| AB retail samples | Seeds (sesame, kalonji, etc.), bakery and tahini products, spices and pistachios | 63 | Not detected in 62 samples S. Ruiru identified in a tahini sauce sample |
Traceback
No convergence was identified in the supplier and distributor information collected from Ontario and Alberta food premises. Other than major suppliers, no commonalities were noted between the suppliers of the ethnic bakeries identified by cases in Ontario and Alberta.
Discussion
Outbreaks of S. Reading are not common. Previously documented S. Reading outbreaks have been associated with sprouts Footnote 7Footnote 8 iceberg lettuce Footnote 9 beef Footnote 10Footnote 11Footnote 12Footnote 13 pork Footnote 13 turkey Footnote 14Footnote 15 oysters Footnote 16 shepherd dogs Footnote 17 and an unknown source Footnote 18. Despite extensive epidemiological, microbiological and traceback investigations, a common source was not identified in this investigation.
This investigation adds to the literature exploring cultural factors (including barriers) related to outbreak investigation and control Footnote 19Footnote 20. It illustrates the importance of cultural competence, i.e. "the knowledge, skills and attitudes […] that are necessary for providing health information, education and services among diverse groups" Footnote 4 for effective public health practice and restates that communicable disease outbreak investigations are aided by a culturally competent approach Footnote 21Footnote 22. Multiple strategies were used to address the critical ethnocultural component of this investigation. Public health personnel, including field epidemiologists, encountered barriers to hypothesis generation due to a lack of reference data on food preferences of the affected ethnocultural communities. To overcome this barrier, the initial questionnaire was tailored towards food items thought to be frequently consumed by individuals of Eastern Mediterranean origin. Additional effort was then invested in a three day food consumption history survey. Interviews were conducted by an Arabic-speaking environmental health officer and/or in partnership with a facilitator known to local public health through established community networks. Cases and community respondents were interviewed in their homes or in familiar community settings to build trust and promote information sharing. Interviews conducted in homes also provided the opportunity to collect food samples.
While resource intensive, these approaches proved invaluable for mitigating language and cultural barriers and for informing the development of the outbreak questionnaire and re-interview tool. Interestingly, despite disparate geographies and different ethnocultural communities affected by the outbreak in Ontario and Alberta, investigators in both jurisdictions aimed for a culturally competent approach that resulted in similar information gathering. This suggests that similar approaches could be adapted to meet the needs of different ethnocultural communities involved in outbreak investigations.
CFIA and provincial laboratories involvement in this investigation was crucial given the number of food samples that were submitted and analyzed. A challenge with a protracted outbreak investigation is that retail samples tested throughout the investigation are unlikely to be representative of the produce that was available at the time of case exposure. Moreover, data detailing the exact date(s) and location(s) of purchase of food items of interest were not available from all cases or small retail premises, which limited the ability of the CFIA to conduct traceback investigations.
Finally, the importance of molecular sub-typing in outbreak investigations cannot be overemphasized. As in many other countries, outbreak investigations in Canada are supported by skilled experts at PulseNet Canada. The ability to conduct PFGE supports identification of geographically disparate clusters that would otherwise be undetected. Reading is a rare Salmonella serotype and isolates were sent to the National Microbiology Laboratory for serotyping confirmation or designation. Thus, challenges in the timeliness of case reporting were encountered. For example, the extended delays between case onset and confirmation of an outbreak case resulted in delayed case interviews and food sampling.
Conclusion
Despite extensive epidemiological, microbiological and traceback investigations, a common source for this S. Reading outbreak was not identified. The identification of specific foods was challenging due to investigators' initial lack of familiarity with frequently consumed food items among affected individuals of Eastern Mediterranean origin, potential language and cultural barriers to case interviews, as well as a lack of background data on expected food exposures in the outbreak population.
Given Canada's ethnic and cultural diversity, cultural competence in approaches to enteric outbreak investigations and food consumption surveys may be useful. Specifically, routine inclusion of questions about ethnicity and/or ethnic foods on hypothesis-generating questionnaires would be of value. Socio-demographic data (income, housing, ethnicity, etc.) are typically not collected by communicable disease outbreak investigators; however, when relevant to exposure data, the information becomes critical. Consideration should also be given to adjusting the food items questioned and terminology adapted to be conducive to the cultures/communities involved. Additional investigative methods following initial case interviews may be indicated. For example, population food consumption surveys in the affected community or in-person open-ended interviews. Addressing the current national reference data gaps on food consumption in ethnocultural minority groups is also needed.
The outbreak investigation team and/or its partners would benefit from cultural competence skills in outbreaks that have an ethnocultural component to identify and address potential barriers. This may involve considering relevant evidence from other areas of public health practice (e.g. health promotion) and/or partnering with local public health and their existing community networks to engage effectively with individuals and ethnocultural and linguistic groups. Appropriate and relevant training to promote cultural competence among Canadian public health professionals, particularly those involved in enteric outbreak investigation, would aid in the implementation of the recommendations.
Author contributions
FT – Project Administration, Conceptualisation, Methodology, Investigation, Writing (original draft and review & editing), LV – Project Administration, Conceptualisation, Methodology, Investigation, Writing (original draft and review & editing), MA – Conceptualisation, Methodology, Investigation, Writing (original draft and review & editing), YW – Investigation, Writing (review & editing), LM – Conceptualisation, Writing (review & editing), LT – Resources, Investigation, Writing (review & editing), AH – Supervision, Writing (review & editing).
Contributors
Salmonella Investigation Team:
- Lance Honish, Albert Health Services - Investigation, Writing (review & editing)
- Victor Mah, Alberta Health - Investigation, Writing (review & editing)
- Karen Johnson, Public Health Ontario - Investigation
- Stephen Moore, Public Health Ontario -Investigation
- Alison Samuel, Public Health Ontario - Investigation
- Aleisha Reimer, National Microbiology Laboratory - Resources
- Chrystal Berry, National Microbiology Laboratory - Resources
- Leah Isaac, Canadian Food Inspection Agency - Investigation
- Sam Mohajer, Canadian Food Inspection Agency - Investigation
- Pasha Marcynuk, Public Health Agency of Canada - Methodology, Investigation
- Sujani Sivanantharajah, Public Health Agency of Canada - Investigation
- Melissa Phypers, Public Health Agency of Canada – Supervision
Acknowledgements
The authors would like to acknowledge all members of the national Outbreak Investigation Coordinating Committee (OICC) for their advice and support for this investigation (local public health colleagues Ontario, Alberta and New Brunswick; Alberta Health Services; Alberta Health; Alberta Provincial Laboratory for Public Health; New Brunswick Department of Health; Public Health Ontario; Public Health Ontario Laboratory; Ontario Ministry of Health and Long-Term Care; Ontario Ministry of Agriculture, Food & Rural Affairs; Canadian Food Inspection Agency; Health Canada; Public Health Agency of Canada).
In addition, the authors also thank the following individuals for their contributions to this investigation or manuscript revision: Sarah Stephen, Samy Tawfik, Ingrid Zazulak, Amanda Yim and Dawn Greenwald from Alberta Health Services-Environmental Public Health; Khalid Hussein from Peel Region Public Health, Melissa Guy from Ottawa Public Health, Kathy Conlon from Toronto Public Health and Margaret McIntyre from Public Health Ontario; Matthew Walker, Christy-Lynn Peterson, Alyssia Robinson, Cynthia Misfeldt and Celine Nadon from the National Microbiology laboratory of the Public Health Agency of Canada.
Conflict of interest
None.
Funding
This work was supported by the Public Health Agency of Canada.