Archived - Challenges of an invasive Streptococcus pneumoniae outbreak in a marginalized population

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 44-12: Adult immunization
Date published: December 6, 2018
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 44-12, December 6, 2018: Adult immunization
Outbreak Report
Outbreak of invasive Streptococcus pneumoniae among an inner-city population in Victoria, British Columbia, 2016–2017
G McKee1*, A Choi1, C Madill2, J Marriott2, P Kibsey2, D Hoyano2
Affiliations
1 School of Population and Public Health, University of British Columbia, Vancouver, BC
2 Island Health, Victoria, BC
Correspondence
Suggested citation
McKee G, Choi A, Madill C, Marriott J, Kibsey P, Hoyano D. Outbreak of invasive Streptococcus pneumoniae among an inner-city population in Victoria, BC, 2016–2017. Can Commun Dis Rep 2018;44(12):317-322. https://doi.org/10.14745/ccdr.v44i12a02
Keywords: Pneumococcal infections, disease outbreaks, homeless persons, drug users, British Columbia, Canada
Abstract
Background: Invasive pneumococcal disease (IPD) is a significant cause of morbidity and mortality; however, outbreaks of IPD are relatively rare. Homelessness and substance use are known risk factors for IPD and have been associated with several outbreaks in Canada, despite national recommendations for routine childhood and targeted adult pneumococcal vaccination.
Objectives: To describe the epidemiology and public health challenges related to an outbreak of novel serotype 4 IPD in a homeless and unstably housed population in Victoria, British Columbia during the autumn and winter of 2016–2017.
Results: Prospective, enhanced surveillance was initiated for laboratory confirmed cases reported to public health, including variables recording housing status and substance use. Thirty-three cases of serotype 4 IPD within the Victoria area were reported to public health between August 1, 2016 and September 1, 2017. Compared with other serotypes, these cases were more likely to be middle-aged, homeless or unstably housed, and to have a recent history of substance use. A targeted pneumococcal vaccination campaign was initiated in collaboration with external community organizations; however, these initiatives were challenged by incomplete data and staffing constraints.
Conclusion: This report illustrates an outbreak of serotype 4 IPD among an inner-city population with multiple risk factors, including homelessness, unstable housing and substance use. Given the challenges controlling the outbreak, outreach capacity and pneumococcal vaccination coverage is needed among this marginalized population.
Introduction
Invasive pneumococcal disease (IPD) results from infection of a normally sterile site by the gram-positive bacterium Streptococcus pneumoniae Footnote 1. Commonly presenting as pneumonia, meningitis or bacteremia, the overall incidence of IPD in Canada ranges between 8.9 and 9.9 cases per 100,000 population Footnote 2. While rates among infants have declined significantly following the implementation of routine childhood vaccination, rates in adults have remained largely unchanged. IPD still represents a significant source of morbidity and mortality, particularly among under-vaccinated, at-risk populations Footnote 2.
Homeless and low-income, inner-city communities are examples of high-risk populations for IPD. While most cases of IPD are sporadic, and (rare) outbreaks are most frequently described in “closed” institutional settings, a number of community-based outbreaks have been reported in inner-city populations in Western Canada Footnote 3Footnote 4Footnote 5. In 2008, the National Advisory Committee on Immunization (NACI) concluded there was sufficient evidence that homeless persons had a higher risk of IPD, whether this represented a causal linkage or a reflection of the risk factors disproportionately present in homeless individuals Footnote 3Footnote 5Footnote 6Footnote 7.
Given that the serotypes attributable to these outbreaks have been among those included in widely-available pneumococcal vaccines, there are considerable opportunities for intervention Footnote 8. NACI recommends that the 23-valent pneumococcal polysaccharide vaccine be provided to homeless persons, as well as those using substances; however, accessing this population has proven challenging, particularly given its transience.
Victoria has a population of approximately 86,000, over 1,700 of whom are homeless or under-housed Footnote 9Footnote 10. A considerable portion of the homeless population is transient, with 28% having moved to Victoria within the past year Footnote 9. Outreach, street nurse and public health services are provided by Island Health, one of five British Columbia (BC) regional health authorities; however, the capacity of these services to serve a dual harm reduction and communicable disease prevention role has been limited. The confluence of rising homelessness, inadequate staffing and competing priorities due to the opioid overdose epidemic have created additional challenges, complicating the response to a serotype 4 IPD outbreak in Victoria, BC, that was detected in the fall of 2016.
The objective of this report is to describe the epidemiology of a community-based serotype 4 IPD outbreak in a homeless and unstably housed population in Victoria, BC, and to describe the associated challenges in the implementation of public health investigations and interventions.
Methods
Outbreak detection
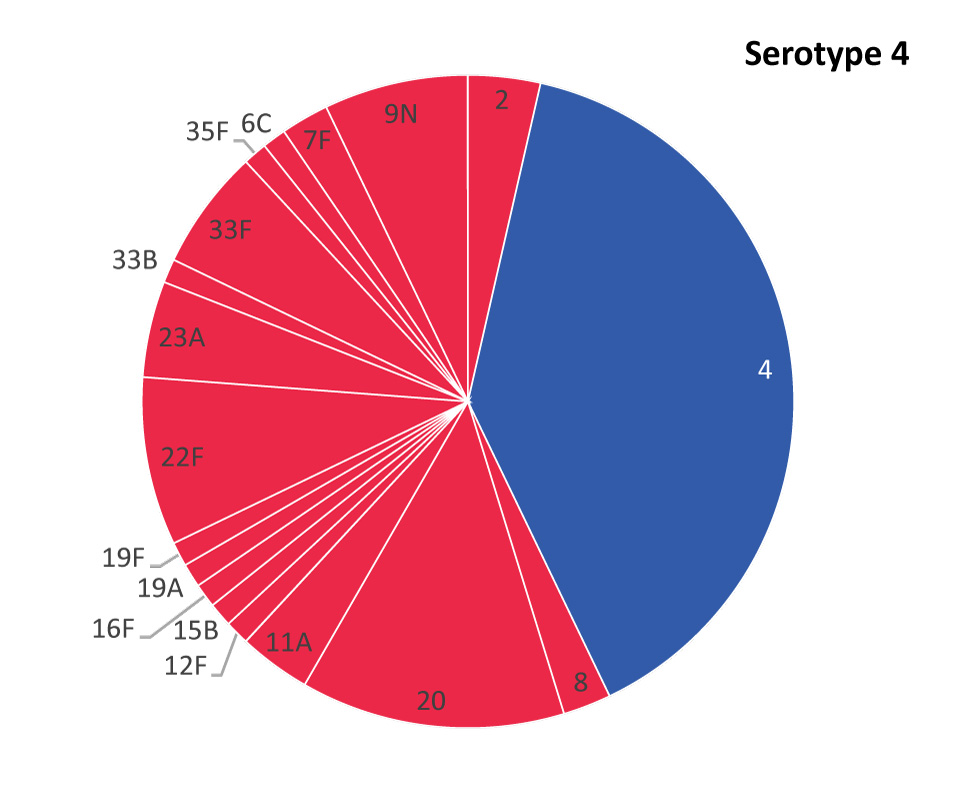
In August 2016, the specialized communicable disease nurses who routinely receive notifications of reportable diseases observed an increase in cases of serotype 4 IPD (predominantly pneumonia), while at the same time the local hospital’s medical microbiologists reported an unusually high number of intensive care unit admissions for homeless, inner-city patients with invasive pneumococcal infection. Regional routine surveillance alerts, which compare counts of reportable diseases to historical 5-year averages, noted an increase in reported cases of IPD, as did the provincial system which issues alerts based on statistical discrepancies between the observed data and historical patterns. According to regional surveillance, the number of IPD cases reported in September 2016 was eight times higher than the 5-year monthly average, while October 2016 experienced a 3-fold increase. In light of these multiple signals, the Medical Health Officer declared an outbreak of serotype 4 IPD in October 2016.
Investigation
IPD has been reportable in BC since 1999 and nationally notifiable in Canada since 2000 Footnote 1Footnote 11. In BC, a case of IPD is defined by clinical evidence of invasive disease with laboratory confirmation of Streptococcus pneumoniae from a normally sterile site, such as blood and CSF, but excluding the middle ear Footnote 12.
All samples were collected at Island Health facilities. S. pneumoniae isolates were cultured and evaluated for drug sensitivity at Royal Jubilee Hospital in Victoria, BC. Further serotyping was performed at the National Microbiology Laboratory. Cases identified by laboratory physicians that met the definition of IPD were reported to public health. Data from all cases of invasive pneumococcal disease in the surrounding region (Southern Island Health Service Delivery Area of Island Health) were collated in Microsoft Excel (Microsoft Corporation, Redmond, Washington, United States) from standardized case report forms used for routine surveillance, as well as electronic medical records.
Case report forms were expanded with additional risk factor variables not previously collected, including housing status and substance use. Although patients were not directly contacted to obtain additional information, a retrospective chart review was conducted using electronic health records from public health encounters, emergency room visits, hospital admissions, outpatient investigations, and mental health and substance use clinical profiles. Case charts were reviewed by two authors (GM and AC) and data was coded based on standardized definitions (Appendix 1). Cases were stratified by serotype (serotype 4 vs. non-serotype 4) for descriptive analysis in Excel. Continuous variables were compared using a non-paired Student’s t test assuming unequal variance. Categorical variables were compared using a χ2 or Fisher’s exact test, depending on cell size. Unadjusted odds ratios were calculated using logistic regression in R statistical software (R Foundation, Vienna, Austria).
Results
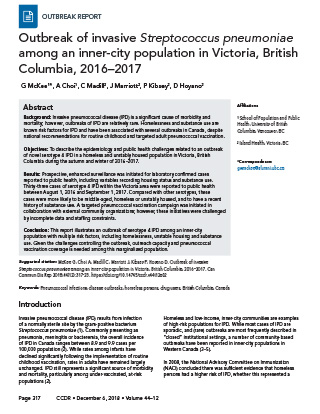
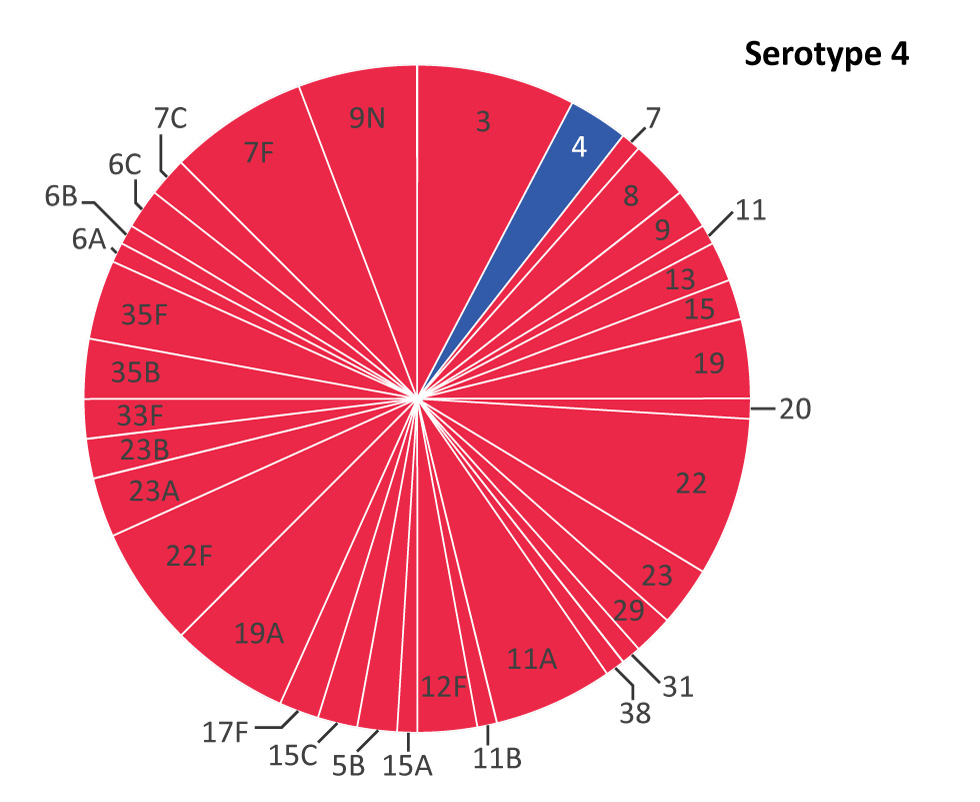
A total of 84 cases of IPD within the South Island Health Service Delivery Area (HSDA) were reported to public health between August 1, 2016 and September 1, 2017. Whereas only three cases of S. pneumoniae serotype 4 were reported within the prior 4.5 years, 33 were identified during the study period, comprising 39.3% of all reported cases of IPD (Figure 1A and 1B).
Figure 1A: Serotype distribution of Streptococcus pneumoniae isolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), January 1, 2012–July 31, 2016
Text description: Figure 1A
Figure 1A: Serotype distribution of Streptococcus pneumoniae isolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), January 1, 2012–July 31, 2016
This figure is a pie chart illustrating the Serotype distribution of Streptococcus pneumoniae isolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), January 1, 2012–July 31, 2016
| Serotype | N |
|---|---|
| 3 | 8 |
| 4 | 3 |
| 7 | 1 |
| 8 | 3 |
| 9 | 2 |
| 11 | 1 |
| 13 | 2 |
| 15 | 2 |
| 19 | 4 |
| 20 | 1 |
| 22 | 8 |
| 23 | 3 |
| 29 | 2 |
| 31 | 1 |
| 38 | 1 |
| 11A | 6 |
| 11B | 1 |
| 12F | 3 |
| 15A | 1 |
| 5B | 2 |
| 15C | 2 |
| 17F | 2 |
| 19A | 6 |
| 22F | 6 |
| 23A | 3 |
| 23B | 2 |
| 33F | 2 |
| 35B | 3 |
| 35F | 4 |
| 6A | 1 |
| 6B | 1 |
| 6C | 2 |
| 7C | 2 |
| 7F | 7 |
| 9N | 6 |
Figure 1B: Serotype distribution of Streptococcus pneumoniae isolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), August 1, 2016–September 1, 2017
Text description: Figure 1B
Figure 1B: Serotype distribution of Streptococcus pneumoniae isolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), August 1, 2016–September 1, 2017
This figure is a pie chart illustrating the serotype distribution of Streptococcus pneumoniaeisolates from patients with invasive pneumococcal disease within the South Island Health Service Delivery Area (British Columbia, Canada), August 1, 2016–September 1, 2017
| Serotype | Number of cases |
|---|---|
| 2 | 3 |
| 4 | 33 |
| 8 | 2 |
| 20 | 11 |
| 11A | 3 |
| 12F | 1 |
| 15B | 1 |
| 16F | 1 |
| 19A | 1 |
| 19F | 1 |
| 22F | 7 |
| 23A | 4 |
| 33B | 1 |
| 33F | 5 |
| 35F | 1 |
| 6C | 1 |
| 7F | 2 |
| 9N | 6 |
Case reports of serotype 4 peaked in September and October 2016 and persisted throughout the study period, slowing down by March 2017 (Figure 2).
Figure 2: Number of reported cases of serotype 4 and non-serotype 4 invasive pneumococcal disease compared with a 5-year monthly average of all serotypes, South Island Health Service Delivery Area (British Columbia, Canada), January 1, 2016–September 1, 2017
Text description: Figure 2
Figure 2: Number of reported cases of serotype 4 and non-serotype 4 invasive pneumococcal disease compared with a 5-year monthly average of all serotypes, South Island Health Service Delivery Area (British Columbia, Canada), January 1, 2016–September 1, 2017
This figure is a combination of a bar chart and a line chart which features the number of reported cases of serotype 4 and non-serotype 4 invasive pneumococcal disease compared with a 5-year monthly average of all serotypes between January 1, 2016 and September 1, 2017.
| Year | Month | Non-Serotype 4 | Serotype 4 | 5-year Monthly Average |
|---|---|---|---|---|
| 2016 | January | 5 | 0 | 3.2 |
| 2016 | February | 4 | 0 | 2.8 |
| 2016 | March | 3 | 0 | 0.6 |
| 2016 | April | 3 | 1 | 2 |
| 2016 | May | 3 | 0 | 1.2 |
| 2016 | June | 0 | 1 | 0.6 |
| 2016 | July | 2 | 0 | 3 |
| 2016 | August | 2 | 2 | 3 |
| 2016 | September | 2 | 6 | 1 |
| 2016 | October | 5 | 6 | 3.4 |
| 2016 | November | 3 | 1 | 5.4 |
| 2016 | December | 2 | 4 | 1.6 |
| 2017 | January | 4 | 4 | 3.2 |
| 2017 | February | 9 | 3 | 4.8 |
| 2017 | March | 10 | 1 | 1.4 |
| 2017 | April | 3 | 0 | 3.2 |
| 2017 | May | 1 | 2 | 2.8 |
| 2017 | June | 2 | 0 | 0.6 |
| 2017 | July | 4 | 2 | 2 |
| 2017 | August | 2 | 0 | 1.2 |
The demographic and risk profiles of serotype 4 and non-serotype 4 cases of IPD reported during the study period are compared in Table 1. There was no significant difference in gender distribution between the two groups, with both serotype groups seen predominantly in males. The median age of serotype 4 cases (median=46 years, Standard Deviation [SD]=15.22 years) was significantly (p<0.001) lower than non-serotype 4 cases (median=63 years, SD=18.21 years) and included no cases over the age of 75 years. Serotype 4 cases were also much more likely to be homeless or unstably housed (48.48% vs. 15.69%). Substance use was more prevalent among serotype 4 cases, although significant differences were only noted for methamphetamine, cannabis, opioids and tobacco smoking.
Variable |
Serotype 4 | Non-Serotype 4 | p-value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Total cases | 33 | 100 | 51 | 100 | N/A |
| Gender | |||||
|
23 | 69.70 | 29 | 56.86 | 0.34 |
| Housing status | |||||
|
16 | 48.48 | 8 | 15.69 | <0.01 |
| Substance use | |||||
|
13 | 39.39 | 16 | 31.37 | 0.80 |
|
10 | 30.30 | 5 | 9.80 | 0.054 |
|
8 | 24.24 | 5 | 9.80 | 0.20 |
|
10 | 30.30 | 3 | 5.88 | <0.05 |
|
18 | 54.55 | 8 | 15.69 | <0.01 |
|
18 | 54.55 | 7 | 13.73 | <0.001 |
|
27 | 81.82 | 18 | 35.29 | <0.001 |
| Co-morbidities | |||||
|
7 | 21.21 | 9 | 17.65 | 1.00 |
|
1 | 3.03 | 3 | 5.88 | 0.64 |
|
9 | 27.27 | 23 | 45.10 | 0.086 |
|
5 | 15.15 | 21 | 41.18 | <0.05 |
|
1 | 3.03 | 13 | 25.49 | <0.01 |
|
1 | 3.03 | 9 | 17.65 | <0.05 |
| IPD presentation | |||||
|
28 | 84.85 | 43 | 84.31 | 1.00 |
|
2 | 6.06 | 3 | 5.88 | 1.00 |
| Level of care | |||||
|
31 | 93.94 | 46 | 90.20 | 1.00 |
|
10 | 30.30 | 12 | 23.53 | 0.70 |
| Outcome | |||||
|
0 | 0 | 10 | 19.61 | <0.01 |
| Immunization | |||||
|
3 | 9.09 | 8 | 15.69 | 0.52 |
Serotype 4 cases generally reported fewer co-morbidities than other serotypes, with significant differences in cardiovascular disease, renal disease and diabetes. No significant differences in clinical presentation or hospital and Intensive Care Unit admission were observed; however, while 10 in-hospital deaths were reported among the non-serotype 4 cases, no in-hospital deaths were reported among the serotype 4 cases.
As illustrated in Table 2, bivariate analysis of risk factors further distinguished serotype 4 cases from other serotypes. Similar to the descriptive analysis, the odds that serotype 4 cases were homeless or unstably housed was 4.82 (95% Confidence Interval [CI] [1.79, 13.97]) times higher than non-serotype 4 cases. Serotype 4 cases were also associated with a higher odds of substance use, including injection drug use (Odds Ratio [OR] 3.65; 95% CI [1.15, 12.95]), methamphetamine use (OR 6.23; 95% CI [1.71, 29.89]), cannabis use (OR 5.85; 95% CI [2.17, 17.07]), opioid use (OR 6.69; 95% CI [2.41, 20.36]) and tobacco smoking (OR 7.25; 95% CI [2.64, 22.62]). Negative associations were observed for cardiovascular disease (OR 0.22; 95% CI [0.07, 0.63]) and renal disease (OR 0.08; 95% CI [0, 0.45]).
| Risk factor | OR | CI 95% |
p-value |
|---|---|---|---|
| Homeless or unstable housing | 4.82 | [1.79, 13.97] | <0.01 |
| Heavy alcohol use | 1.26 | [0.50, 3.18] | 0.62 |
| Injection drug use | 3.65 | [1.15, 12.95] | <0.05 |
| Cocaine | 2.62 | [0.79, 9.53] | 0.12 |
| Methamphetamine | 6.23 | [1.71, 29.89] | <0.01 |
| Cannabis | 5.85 | [2.17, 17.07] | <0.001 |
| Opioids | 6.69 | [2.41, 20.36] | <0.001 |
| Tobacco smoking | 7.25 | [2.64, 22.62] | <0.001 |
| HCV | 1.17 | [0.37, 3.52] | 0.78 |
| HIV | 0.47 | [0.02, 3.85] | 0.52 |
| Lung disease | 0.39 | [0.15, 1.00] | 0.054 |
| Cardiovascular disease | 0.22 | [0.07, 0.63] | <0.01 |
| Renal disease | 0.08 | [0, 0.45] | <0.05 |
| Diabetes | 0.13 | [0.01, 0.76] | 0.060 |
Public health response
In response to the outbreak, Island Health’s Street Outreach Program initiated a campaign to increase uptake of 23-valent polysaccharide vaccine containing serotype 4, which was significantly bolstered through collaborations with several inner-city service providers that had pre-existing relationships with those at highest risk of infection. Approximately 100 doses were administered between August 2016 and September 2017 by street outreach nurses, while over 80 additional doses were administered by other providers serving this at-risk population.
By April 2017, the total number of reported IPD cases had declined to levels comparable to the baseline average. Following persistent, low numbers of reported cases over the subsequent months, it was concluded that enhanced surveillance was no longer necessary; however, the proportion of IPD cases due to serotype 4 remained higher than pre-outbreak levels, suggesting persistent low-level circulation.
Discussion
Despite ongoing endemicity of pneumococcal infection in Canada, outbreaks of invasive pneumococcal disease are relatively rare. Serotype 4 is reported to have a high level of invasiveness, although some studies have suggested that this may be more strongly linked to capsular composition than serotype Footnote 13. Nonetheless, invasive serotypes are often implicated in outbreaks of IPD, such as the serotype 5 outbreaks reported in Canada Footnote 3Footnote 5. This report adds to the limited literature available on outbreaks of serotype 4 IPD. Given the characteristics of the homeless population affected by this outbreak and what is known about the risks of IPD, strengthening targeted prevention programs may be indicated.
The implication of a vaccine-preventable serotype Footnote 4 in this outbreak suggests the current approach to administering recommended vaccines among this at-risk population is not entirely effective. Despite the NACI recommendations to offer pneumococcal vaccine to homeless individuals and people who used drugs, these populations are often difficult to reach. The limited capacity for street nurses to provide outreach services to the inner-city population presented a challenge both prior to and during the outbreak. Despite pre-existing staffing constraints, this service was further challenged by competing priorities associated with the response to the opioid crisis. Transmission of pneumococcus may thus have been exacerbated by a decrease in targeted pneumococcal vaccination in the preceding year due to this limited street outreach capacity within the Victoria region. These deficiencies were recognized during the outbreak and an additional position was created to bolster the service.
The targeted pneumococcal vaccination campaign represented a core component of the public health response to the IPD outbreak. It is difficult to determine the degree to which the efforts to expand uptake contributed to the observed reduction in new onset cases. Similar vaccine campaigns designed to curtail IPD outbreaks have reported mixed results Footnote 3Footnote 5.
During the outbreak, several barriers to targeted vaccination were identified, including incomplete vaccination records, which made it difficult to identify those who required vaccination. While both public health staff and community providers within the health authority administer vaccines, they utilize different information systems. Integrated health and vaccination records could have improved both individual-level assessments of vaccination status and population-level assessments of vaccine effectiveness.
In addition to staffing constraints and incomplete vaccination records, other challenges limited the extent of the investigation. As we relied on retrospective chart review for information about case risk factors, under-reporting of risk factors may have introduced misclassification bias. While the standard practice for public health nurses within the health authority involves no direct follow-up of IPD cases, interviews may have provided additional details, allowing for better insight into potential transmission patterns. In the future, further analysis of contact networks may allow for identification of potential sites of transmission, such as a specific shelter or gathering place, which could inform targeted public health measures.
Conclusion
This report illustrates an outbreak of serotype 4 invasive pneumococcal disease among an inner-city population with multiple risk factors for transmission, including homelessness, unstable housing and substance use. It also reinforces the ongoing need to improve outreach capacity and pneumococcal vaccine coverage among this marginalized population.
Authors' statement
All authors were involved in conceptualization, analysis/interpretation of data, and drafting of the manuscript. GM, AC, CM and JM were also involved in data collection.
Conflict of interest
None.
Acknowledgements
We would like to acknowledge the Island Health and community partners who were instrumental in managing this outbreak, both through care provision, social supports, and assistance with the vaccination campaign, as well as the National Microbiology Laboratory for their role in serotyping the samples. We would also like to acknowledge Angela Reid, surveillance analyst at Island Health, for providing data support, and Dr. Monika Naus, Medical Director for the Communicable Diseases & Immunization Service at the BC Centre for Disease Control, for reviewing the manuscript.
Appendix
| Variable | Definition |
|---|---|
|
Age at hospital admission for IPD, as documented in electronic medical record |
|
Gender as documented in electronic medical record |
|
No fixed address OR identified as homeless OR under-housed OR couch surfing OR living in tents OR shelters as documented in electronic medical record |
| Substance use | |
|
Current alcohol use disorder OR alcohol use that exceeds low-risk guidelines, as documented in electronic medical record |
|
Injection drug use as documented in electronic medical record |
|
Cocaine use described in chart notes OR detected on toxicological screen within last year, as per electronic medical record |
|
Methamphetamine use described in chart notes OR detected on toxicological screen within last year, as per electronic medical record |
|
Cannabis use described in chart notes OR detected on toxicological screen within last year, as per electronic medical record |
|
Illicit opioid use described in chart notes OR detected on toxicological screen within last year, as per electronic medical record |
|
Recent tobacco smoking (within previous year) described in chart notes, as per electronic medical record |
| Co-morbidities | |
|
Hepatitis C virus infection described in chart notes or laboratory records, as per electronic medical record |
|
HIV infection described in chart notes or laboratory records, as per electronic medical record |
|
Co-morbid lung disease described in chart notes, as per electronic medical record |
|
Co-morbid cardiovascular disease described in chart notes, as per electronic medical record |
|
Co-morbid renal disease described in chart notes, as per electronic medical record |
|
Co-morbid diabetes mellitus described in chart notes, as per electronic medical record |
| IPD presentation | |
|
Pneumococcal pneumonia as documented in electronic medical record |
|
Pneumococcal meningitis as documented in electronic medical record |
| Level of care | |
|
Admission to hospital for IPD, as documented in electronic medical record |
|
Number of days calculated from date of hospital admission (within Island Health) for IPD to date of death or discharge. |
|
Admission to ICU during hospital stay for IPD, as documented in electronic medical record |
| Outcome | |
|
Death during hospital admission for IPD, as documented in electronic medical record |
| Immunization | |
|
Previous pneumococcal vaccination within the last 5 years as documented in electronic medical record or electronic Public Health Information System |