Mumps outbreak in Manitoba, Canada, 2018–2019

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 46–4: Respiratory syncytial virus (RSV)
Date published: April 2, 2020
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 46–4, April 2, 2020: Respiratory syncytial virus (RSV)
Outbreak
Large community mumps outbreak in Manitoba, Canada, September 2016–December 2018
Yichun Wei1, Krista Wilkinson2, Richard Rusk3, Kamran Kadkhoda4,5, Carla Loeppky1,6
Affiliations
1 Epidemiology and Surveillance, Manitoba Health, Seniors and Active Living, Winnipeg, MB
2 Population and Public Health, Winnipeg Regional Health Authority, Winnipeg, MB
3 Communicable Disease Control, Manitoba Health, Seniors and Active Living, Winnipeg, MB
4 Cadham Provincial Laboratory, Winnipeg, MB
5 Immunopathology Laboratory, Cleveland Clinic – Main Campus, Cleveland, OH
6 Department of Community Health Sciences, University of Manitoba, Winnipeg, MB
Correspondence
Suggested citation
Wei Y, Wilkinson K, Rusk R, Kadkhoda K, Loeppky C. Large community mumps outbreak in Manitoba, Canada, September 2016–December 2018. Can Commun Dis Rep 2020;46(4):70–6. https://doi.org/10.14745/ccdr.v46i04a03
Keywords: mumps, outbreak, incidence, vaccination, MMR vaccine, investigation, immunity, Manitoba
Abstract
Background: After routine mumps immunization programs were implemented in Manitoba in the 1980s, incidence was low, with 0–9 cases of disease annually. In September 2016, a mumps outbreak began in fully vaccinated university students in Winnipeg, Manitoba.
Objective: We describe the investigation of this province-wide mumps outbreak, which lasted between September 2016 and December 2018. We present the details of public health measures implemented and challenges encountered. Possible contributing factors to the sustained transmission are also provided.
Methods: Probable and confirmed cases of mumps were investigated by public health departments using the investigation form developed for this outbreak. Confirmed mumps cases were linked to the provincial immunization registry. An outbreak response team planned and implemented control measures across the province.
Results: The outbreak began in vaccinated university students in September 2016 and spread across the province. Activity was high and prolonged in the northern remote areas. By the end of 2018, 2,223 cases had been confirmed. All age groups were affected, and incidence was highest among people aged 18–29 years. Two-dose coverage of mumps-containing vaccine in confirmed cases was close to 70%.
Conclusion: This prolonged outbreak revealed a large vulnerable population likely resulting from under-vaccination and waning vaccine-induced immunity in the absence of natural boosting from exposure to mumps virus. It is important to maintain high two-dose coverage with mumps-containing vaccines. A third dose of mumps-containing vaccine in future outbreaks may be considered.
Introduction
Mumps is an illness caused by the mumps virus, of the Paramyxoviridae family. Symptoms of mumps infection include fever, headache and the characteristic swelling and tenderness of the parotid or other salivary glands. Aseptic meningitis, encephalitis, orchitis, oophoritis, deafness and pancreatitis are some rare complications due to mumps infectionFootnote 1Footnote 2Footnote 3. In Manitoba, laboratory-confirmed and probable cases are required to be reported to Manitoba Health, Seniors and Active Living (MHSAL) under The Manitoba Public Health ActFootnote 4.
A single dose of the measles–mumps–rubella (MMR) vaccine, at 12 months of age, was added to the routine childhood immunization schedule in Manitoba in 1983. A second dose of the MMR vaccine, for children aged 4–6 years, was added to the routine schedule in 1996Footnote 5. This is consistent with the most recent recommendation of 2007, from the National Advisory Committee on Immunization (NACI) for mumps-containing vaccine. After reviewing mumps outbreaks in Canada and internationally, NACI recommended two-dose routine mumps immunization in infants and children as well as in certain high-risk adult groups including secondary and postsecondary students, military personnel and health care workersFootnote 6.
Historically, the incidence of mumps has been continually low in Manitoba, with 0–9 cases each year between 2000 and 2015 or 0.3 cases per 100,000 population, on averageFootnote 7. Disease is most common in people aged 18–45 years. In recent years, the average incidence rate of mumps in Canada was 0.3 cases per 100,000 population from 2011 to 2015Footnote 8.
On October 18, 2016, routine surveillance detected a cluster of six cases of mumps with symptom onset between September 25 and October 12, 2016, in Winnipeg, the capital city of Manitoba. All six were University of Manitoba students aged 18–24 years; three were on university athletic teams. All had documented receipt of two doses of MMR vaccine in childhood. MHSAL declared a mumps outbreak and established an outbreak response team on the same day. Five regional health authorities deliver publicly funded health services in five geographic regions in Manitoba: one urban region, the Winnipeg Regional Health Authority, and four rural regions, Interlake–Eastern Regional Health Authority, Southern Health–Santé Sud, Prairie Mountain Health and Northern Regional HealthFootnote 9. All regional health authorities participated on the response team.
In this report, we describe the investigation of this province-wide mumps outbreak between September 2016 and December 2018. We also present the details of public health measures implemented and challenges encountered. Possible contributing factors to the sustained transmission are also provided.
Methods
A provincial outbreak of mumps was declared on October 18, 2016, and was confirmed over on December 31, 2018, when activity level returned to baseline. This outbreak originated in a university population, but spread quickly, evolving into a large and sustained outbreak across the entire province. The outbreak response team planned and implemented control measures including prompt contact tracing, recommendations of self-isolation after symptom onset, communication (including dissemination of educational materials) and the offer of MMR vaccine to susceptible contacts.
Epidemiologic investigation
Case definitions were derived from the provincial communicable disease management protocol for mumpsFootnote 10. A probable case was defined as the occurrence of symptoms compatible with mumps (acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland) that lasted two days or more, on or after September 1, 2016. A confirmed case was defined as a laboratory confirmation of recent mumps infection in a probable case or a probable case with an epidemiologic link to a laboratory-confirmed case and in the absence of recent vaccination with mumps-containing vaccines. The MHSAL’s Communicable Disease Management Protocol recommends that investigators consult the current Canadian Immunization Guide for information on age-specific reactions and timeframes when determining if symptoms were possibly due to a recent dose of mumps-containing vaccine.
An outbreak investigation form was developed to collect information on demographics, occupation, symptoms, complications and severity, vaccination status and activities during the incubation period (12–25 days before the onset of parotitis) and communicability period (seven days before until five days after the onset of parotitis). Regional health authorities implemented outbreak investigation and control measures immediately. Regional public health nurses interviewed cases and completed investigation forms before submitting to MHSAL.
MHSAL coordinated data collection and data entry. General information about all mumps reports were captured in the routine surveillance database. An outbreak-specific database was implemented to capture information from the outbreak investigation forms. Due to the high volume of mumps reports, only confirmed cases were entered into the outbreak investigation database. Confirmed cases were linked to the provincial immunization registry to calculate vaccination coverage rates. We conducted descriptive analyses to identify the epidemiologic and geographic characteristics of the outbreak. Data linkage and analysis were conducted using SAS Enterprise Guide, version 7.1 [SAS Institute Inc., Cary, North Carolina, United States (US)].
Laboratory investigation
The Cadham Provincial Laboratory in Winnipeg performed standard laboratory testing on specimens, including tests to detect mumps virus immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies in acute and convalescent serum specimens approximately 7–10 days apart; tests for mumps virus RNA through reverse transcription polymerase chain reaction (RT-PCR); and attempts to isolate mumps virus in culture. Samples of positive cultures were sent to the National Microbiology Laboratory (NML) for viral genotyping.
Vaccination coverage
Vaccinations for cases were extracted from the population-based provincial immunization registry within the Public Health Information Management System (PHIMS). The registry was implemented in 1988 to record vaccinations for those born in Manitoba on or after January 1, 1980. Vaccinations received outside of Manitoba are not entered without an official document. As a result, vaccination records are generally more complete for people younger than 30 years or born after 1986 who grew up in Manitoba.
Interventions
Control measures included prompt contact tracing, with regional public health nurses conducting case and contact management. Self-isolation for five days after symptom onset was recommended to symptomatic cases. Contacts who might have been exposed during the period of communicability were notified. They also received mumps-related education, including information about early signs and symptoms, and were advised to see a health care provider if they developed symptoms.
MMR vaccines were offered to susceptible contacts (people with zero documented doses of mumps-containing vaccine born between 1970 and 1984 and those with less than two documented doses born after 1984), based on Manitoba’s eligibility criteriaFootnote 11 and the most recent NACI recommendationFootnote 6. Health care facilities were encouraged to ensure that all staff were vaccinated. In correctional facilities with cases, vaccination clinics were held to offer vaccines to susceptible staff and inmates.
MHSAL disseminated educational materials to universities, schools and the general public. A series of letters were sent to Manitoba universities, schools, daycare centres and sports organizations to increase public awareness. MHSAL also responded to media requests and issued news releases to provide updates on the outbreak and emphasize the importance of vaccination. A public website maintained by MHSAL provided weekly updates. Health care providers received letters to guide prevention and control practices. MHSAL issued public health alerts through the Canadian Network for Public Health Intelligence (CNPHI) to notify other provincial and federal public health counterparts.
The outbreak response team considered the possibility of offering a third dose of MMR as an intervention in Northern Regional Health in January 2018 after the US Advisory Committee on Immunization Practices published updated recommendationsFootnote 12. Northern Regional Health provides service to approximately 75,000 residents in northern Manitoba, the smallest population in five regions, but distributed across the largest geographic area. Many live in remote and isolated communities, and some communities can only be accessed by plane or boat. MHSAL decided not to recommend a third dose of MMR due to operational feasibility in northern areas. As the virus had been circulating regionally for an extended period of time, it was not possible to define an eligible population who would have benefited from a third dose.
Results
Descriptive epidemiology
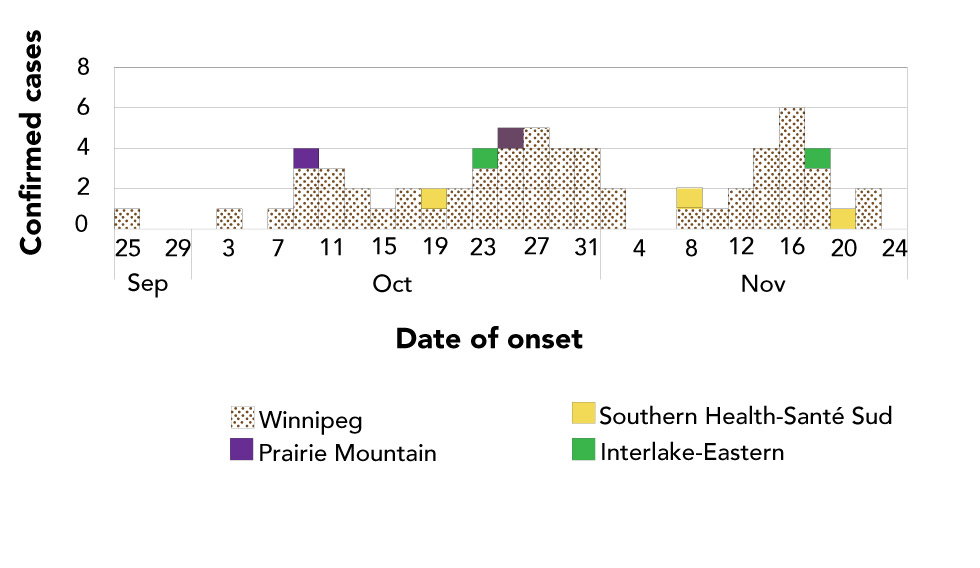
This mumps outbreak started among university students in the Winnipeg Regional Health Authority. This region serves approximately 57% of the 1.4 million residents of Manitoba. Three peaks in the early months of the outbreak corresponded to three important exposure events: multiple homecoming celebrations at the University of Manitoba (September 19–25, 2016); Thanksgiving weekend (October 8–10), which might have resulted in infectious people travelling; and Halloween (October 31) (Figure 1a). During this period, cases included young adults in Winnipeg who were linked to universities, schools, sports gatherings and/or holidays.
Figure 1a: Confirmed cases of mumps (N=65) by date of symptom onset and health region, Manitoba, September 25–November 26, 2016
Text description: Figure 1a
Figure 1a: Confirmed cases of mumps (N=65) by date of symptom onset and health region, Manitoba, September 25–November 26, 2016
| Months in 2016 | Number of confirmed cases | Winnipeg Regional Health Authority | Prairie Mountain Health | Southern Health-Santé Sud | Interlake-Eastern Regional Health |
|---|---|---|---|---|---|
| September | 25 | 1 | 0 | 0 | 0 |
| 27 | 0 | 0 | 0 | 0 | |
| 29 | 0 | 0 | 0 | 0 | |
| October | 1 | 0 | 0 | 0 | 0 |
| 3 | 1 | 0 | 0 | 0 | |
| 5 | 0 | 0 | 0 | 0 | |
| 7 | 1 | 0 | 0 | 0 | |
| 9 | 3 | 1 | 0 | 0 | |
| 11 | 3 | 0 | 0 | 0 | |
| 13 | 2 | 0 | 0 | 0 | |
| 15 | 1 | 0 | 0 | 0 | |
| 17 | 2 | 0 | 0 | 0 | |
| 19 | 1 | 0 | 1 | 0 | |
| 21 | 2 | 0 | 0 | 0 | |
| 23 | 3 | 0 | 0 | 1 | |
| 25 | 4 | 1 | 0 | 0 | |
| 27 | 5 | 0 | 0 | 0 | |
| 29 | 4 | 0 | 0 | 0 | |
| 31 | 4 | 0 | 0 | 0 | |
| November | 2 | 2 | 0 | 0 | 0 |
| 4 | 0 | 0 | 0 | 0 | |
| 6 | 0 | 0 | 0 | 0 | |
| 8 | 1 | 0 | 1 | 0 | |
| 10 | 1 | 0 | 0 | 0 | |
| 12 | 2 | 0 | 0 | 0 | |
| 14 | 4 | 0 | 0 | 0 | |
| 16 | 6 | 0 | 0 | 0 | |
| 18 | 3 | 0 | 0 | 1 | |
| 20 | 0 | 0 | 1 | 0 | |
| 22 | 2 | 0 | 0 | 0 | |
| 24 | 0 | 0 | 0 | 0 |
Over 80% of those university students who were born in Manitoba had received two doses of mumps-containing vaccines (data not shown).
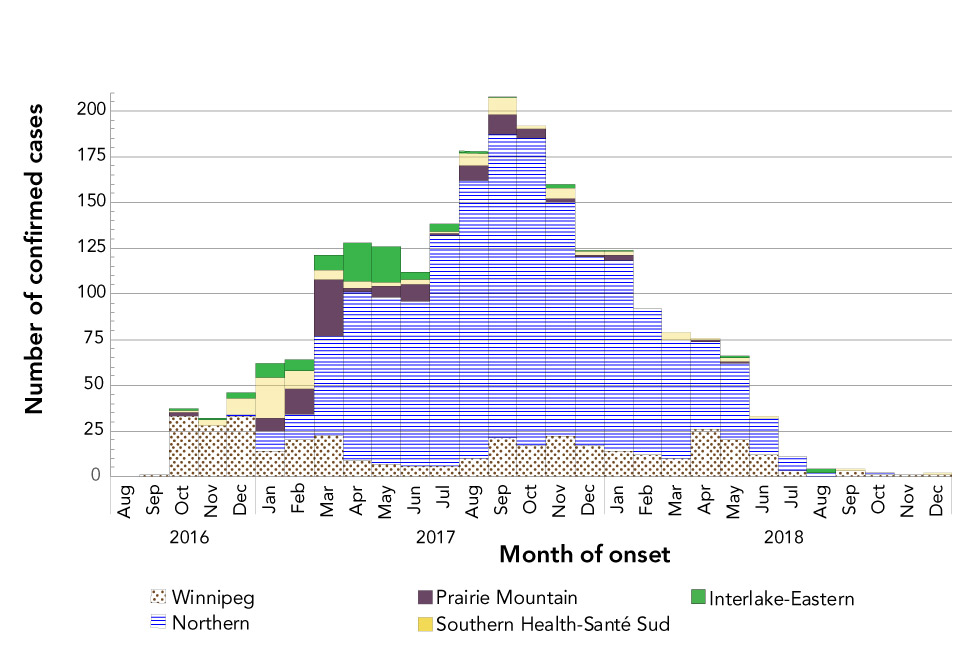
By late November 2016, mumps had spread to three rural health regions, Interlake–Eastern Regional Health, Southern Health–Santé Sud and Prairie Mountain Health, including to correctional facilities in those regions. By January 2017, mumps had spread to the most rural region, Northern Regional Health. The number of mumps cases in this region continued to increase throughout the year, peaking in mid-September 2017. Compared with the other health regions, mumps morbidity in Northern Regional Health was high and prolonged. Even with the geographic isolation of communities, mumps continued to spread throughout the region, ultimately infecting almost 2% of the regional population.
After September 2017, the number of mumps cases in Manitoba began to decline, largely driven by the decline in cases in Northern Regional Health. MHSAL declared the outbreak over at the end of 2018 when it was clear that mumps activity had returned to baseline (Figure 1b).
Figure 1b: Confirmed cases of mumps (N=2,223) by month of symptom onset and health region, Manitoba, September 2016–December 2018
Text description: Figure 1b
Figure 1b: Confirmed cases of mumps (N=2,223) by month of symptom onset and health region, Manitoba, September 2016–December 2018
| Year | Month | Winnipeg | Interlake-Eastern | Prairie Mountain | Southern Health-Santé Sud | Northern | Total number of cases |
|---|---|---|---|---|---|---|---|
| 2016 | August | 0 | 0 | 0 | 0 | 0 | 0 |
| September | 1 | 0 | 0 | 0 | 0 | 1 | |
| October | 33 | 1 | 2 | 1 | 0 | 37 | |
| November | 28 | 1 | 0 | 3 | 0 | 32 | |
| December | 33 | 3 | 0 | 9 | 1 | 46 | |
| 2017 | January | 14 | 8 | 7 | 22 | 11 | 62 |
| February | 20 | 6 | 14 | 10 | 14 | 64 | |
| March | 23 | 8 | 31 | 5 | 54 | 121 | |
| April | 9 | 21 | 2 | 4 | 92 | 128 | |
| May | 7 | 20 | 6 | 2 | 91 | 126 | |
| June | 6 | 4 | 9 | 3 | 90 | 112 | |
| July | 6 | 4 | 1 | 1 | 126 | 138 | |
| August | 10 | 1 | 8 | 7 | 152 | 178 | |
| September | 21 | 1 | 11 | 9 | 166 | 208 | |
| October | 17 | 0 | 5 | 2 | 168 | 192 | |
| November | 22 | 2 | 2 | 6 | 128 | 160 | |
| December | 17 | 1 | 1 | 2 | 103 | 124 | |
| 2018 | January | 14 | 1 | 3 | 2 | 104 | 124 |
| February | 12 | 0 | 0 | 0 | 80 | 92 | |
| March | 10 | 0 | 0 | 4 | 65 | 79 | |
| April | 26 | 0 | 1 | 1 | 48 | 76 | |
| May | 20 | 1 | 1 | 2 | 42 | 66 | |
| June | 12 | 0 | 0 | 1 | 20 | 33 | |
| July | 3 | 0 | 0 | 0 | 8 | 11 | |
| August | 0 | 2 | 0 | 0 | 2 | 4 | |
| September | 3 | 0 | 0 | 1 | 0 | 4 | |
| October | 1 | 0 | 0 | 0 | 1 | 2 | |
| November | 1 | 0 | 0 | 0 | 0 | 1 | |
| December | 1 | 0 | 0 | 1 | 0 | 2 | |
| Total | 370 | 85 | 104 | 98 | 1,566 | 2,223 | |
Outbreak investigation confirmed 2,223 mumps cases (1.6 cases per 1,000 population). Of the 2,223 mumps cases, 1,566 (70.4%) were reported from Northern Regional Health and 370 (16.6%) from Winnipeg Regional Health Authority. Females accounted for 48.8% (n=1,084) of all provincial cases (Table 1).
| Characteristics | Regional health authority | Total | ||||
|---|---|---|---|---|---|---|
| Northern | Winnipeg | Prairie Mountain | Southern Health–Santé Sud | Interlake–Eastern | ||
| Cumulative incidenceFootnote a of Table 1 | 20.4 | 0.5 | 0.6 | 0.5 | 0.7 | 1.6 |
| Cases, N | 1,566 | 370 | 104 | 98 | 85 | 2,223 |
|
70.4 | 16.6 | 4.7 | 4.4 | 3.8 | 100 |
| Female, N | 809 | 164 | 40 | 28 | 43 | 1,084 |
|
51.7 | 44.3 | 38.5 | 28.6 | 50.6 | 48.8 |
| Median age, years | 26 | 24 | 26 | 24 | 27 | 25 |
|
15 | 18 | 19 | 18 | 18 | 17 |
|
36 | 33 | 36 | 38 | 40 | 36 |
| UnvaccinatedFootnote b of Table 1, N | 51 | 20 | 3 | 5 | 4 | 83 |
|
5.9 | 11.4 | 6.4 | 10.9 | 8.3 | 7.0 |
| Partially vaccinatedFootnote c of Table 1, N | 200 | 42 | 10 | 9 | 17 | 278 |
|
23.1 | 24.0 | 21.3 | 19.6 | 35.4 | 23.5 |
| Fully vaccinatedFootnote d of Table 1, N | 616 | 113 | 34 | 32 | 27 | 822 |
|
71.0 | 64.6 | 72.3 | 69.6 | 56.3 | 69.5 |
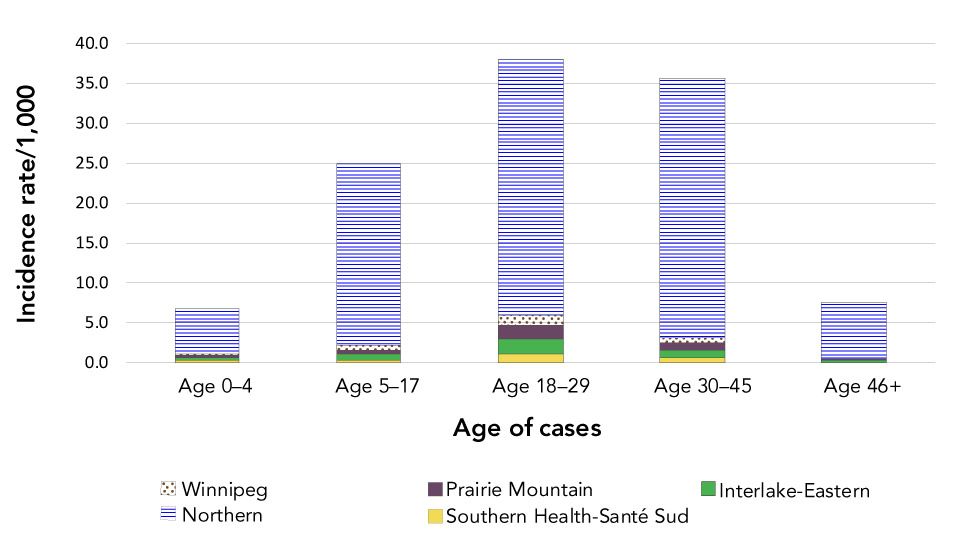
Overall, in Manitoba incidence was highest (3.4 cases per 1,000) in people aged 18–29 years. In Northern Regional Health (Figure 2), incidence in people aged 30–45 years (32.5 cases per 1,000) was similar to that in people aged 18–29 years (32.0 cases per 1,000). Incidence in Northern Regional Health (20.4 cases per 1,000) was substantially higher than in all other regions (range=0.5–0.7 cases per 1,000).
Figure 2: Cumulative incidence rate per 1,000 of mumps cases by age group and health region, Manitoba, Canada, September 2016–December 2018
Text description: Figure 2
Figure 2: Cumulative incidence rate per 1,000 of mumps cases by age group and health region, Manitoba, Canada, September 2016–December 2018
| Regional Health Authority | Age group in years | Rate |
|---|---|---|
| Interlake-Eastern | 0–4 | 0.4 |
| Interlake-Eastern | 5–17 | 0.7 |
| Interlake-Eastern | 18–29 | 1.9 |
| Interlake-Eastern | 30–45 | 0.9 |
| Interlake-Eastern | 46+ | 0.2 |
| Northern | 0–4 | 5.6 |
| Northern | 5–17 | 22.8 |
| Northern | 18–29 | 32.0 |
| Northern | 30–45 | 32.5 |
| Northern | 46+ | 7.0 |
| Prairie Mountain | 0–4 | 0.2 |
| Prairie Mountain | 5–17 | 0.5 |
| Prairie Mountain | 18–29 | 1.7 |
| Prairie Mountain | 30–45 | 1.0 |
| Prairie Mountain | 46+ | 0.1 |
| Southern Health-Santé Sud | 0–4 | 0.3 |
| Southern Health-Santé Sud | 5–17 | 0.4 |
| Southern Health-Santé Sud | 18–29 | 1.1 |
| Southern Health-Santé Sud | 30–45 | 0.7 |
| Southern Health-Santé Sud | 46+ | 0.1 |
| Winnipeg | 0–4 | 0.3 |
| Winnipeg | 5–17 | 0.6 |
| Winnipeg | 18–29 | 1.3 |
| Winnipeg | 30–45 | 0.5 |
| Winnipeg | 46+ | 0.1 |
MHSAL received one report of orchitis and one report of meningitis likely due to mumps infection. No deaths were reported.
Laboratory results
The majority of all confirmed cases (97.1%) were laboratory-confirmed, including 87.8% by RT-PCR testing, 9.2% by serology and 0.1% by viral culture; 2.8% of cases in symptomatic patients were confirmed by an epidemiologic link to laboratory-confirmed cases.
Initially, all samples were shipped to NML for genotyping. After the volume of samples exceeded the NML’s capacity, approximately 10% of randomly selected samples were cultured and genotyped. Of these 243 samples, 229 (94.2%) were found to be genotype G, the endemic mumps virus genotype circulating in Canada and the USFootnote 12. The remaining samples could not be sequenced.
Vaccination status
The vaccination history for cases younger than 30 years who had lived in Manitoba since birth was available from the population-based provincial immunization registry. Based on the registry, of the 1,183 (53.2%) cases aged 5–29 years who were eligible for two doses of mumps-containing vaccines in Manitoba and were registered with MHSAL at age younger than two months, 822 (69.5%) had received at least two doses (Table 1). Two-dose mumps vaccination coverage among mumps cases ranged from 56.3% in the Interlake–Eastern region to 72.3% in the Prairie Mountain region. Of the 822 cases vaccinated with at least two doses of mumps-containing vaccine, the median interval between receipt of the last dose and symptom onset was 11.3 years.
Discussion
MHSAL led an outbreak investigation during a provincial mumps outbreak that continued from September 2016 to December 2018. According to the Surveillance and Epidemiology Division at the Public Health Agency of Canada, as of January 2019 the magnitude of this outbreak was the largest in Canada in the last 20 years, based on reported cases. This outbreak began in university students with high two-dose mumps vaccination coverage and spread to other communities across Manitoba, likely facilitated by social events. The activity level was especially high and prolonged in Northern Regional Health, the most rural region of Manitoba with a large number of isolated communities.
This outbreak revealed a large susceptible population, despite the availability of publicly funded mumps vaccinations for 30 years. Low mumps vaccination coverage probably contributed to this outbreak, though the contribution varied by geographic region. Mumps vaccination coverage in Manitoba has remained below the estimated 92% needed to achieve and sustain herd immunityFootnote 13. In 2017, 90% of those aged 17 years who had lived continuously in Manitoba since birth had two doses of mumps-containing vaccines recorded in the provincial immunization registry compared to 31% of those aged 17 years who had not lived continuously in Manitoba since birth, partially due to incomplete records in the registry for residents not born in ManitobaFootnote 14.
Cases included young, vaccinated adults, indicating that waning vaccine-induced immunity was probably a more important contributor to this outbreakFootnote 3. Almost three-quarters (70%) of cases with records in the provincial registry were fully immunized. However, of cases vaccinated with at least two documented doses of mumps-containing vaccine, a median of more than 11 years had elapsed since receipt of the most recent dose. This is consistent with other reports of waning vaccine-induced immunity against mumps diseaseFootnote 15Footnote 16Footnote 17.
This waning immunity might be attributable to the absence of boosting from natural exposure to wild-type mumps virusFootnote 18Footnote 19. Unlike other Canadian provinces and territories that have reported smaller mumps outbreaks since the 1980s, mumps reports were historically rare in ManitobaFootnote 7. In northern Manitoba, where the population density is low and vaccination coverage is high, natural boosting from disease exposure is even less likely than in the other areas in Manitoba.
In addition, the mumps strain in the North American (Jeryl-Lynn) vaccine is genotype A. The replacement of the genotype A mumps virus from the prevaccine era with the genotype G mumps virus currently endemic in Canada and the US may also contribute to waning immunityFootnote 20.
The number of reported mumps-associated complications in this outbreak was low, which might reflect gaps in public health surveillance as case investigation might have been conducted before complications developed. It is possible that previous mumps vaccination conferred some protection against severe diseaseFootnote 21Footnote 22. Because complications were infrequently reported, analysis of vaccine effectiveness against severe mumps complications was not possible.
Limitations
The vaccination history for some cases was not available in the provincial immunization registry; therefore, coverage among cases might have been higher. If so, low coverage might have contributed even less to this outbreak than waning vaccine-induced immunity. In a future study, this research team plans to explore the relationship between time since the last dose of mumps-containing vaccine and mumps disease.
Conclusion
A substantial and sustained public health effort was required during this outbreak, which originated among university students and spread throughout the province. This highlights the importance of achieving and maintaining high two-dose coverage of mumps-containing vaccines in the population. Due to waning of vaccine-induced immunity, a large cohort of susceptible people may remain in the population; a third dose of mumps-containing vaccine may be considered in future outbreaks to boost vaccine-induced immunity if warranted by epidemiologic data.
Authors’ statement
- YW — Conceptualization, methodology, investigation, formal analysis, writing–original draft, writing–review & editing
- KW — Conceptualization, methodology, writing–review & editing
- RR — Methodology, writing–review & editing
- KK — Methodology, writing–review & editing
- CL — Supervision, writing–review & editing
Conflict of interest
No potential conflicts of interest were disclosed.
Acknowledgements
We would like to acknowledge the following individuals for their contribution: N Casaclang, D Race, I Hossack, T Hilderman from Manitoba Health, Seniors and Active Living; K Dust from Cadham Provincial Laboratory, Manitoba; D MacDonald, and M Roy from Public Health Agency of Canada.
Funding
No external funding was received.
