Tuberculosis outbreak in northern Saskatchewan First Nations community

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 47 No. 11, November 2021: Multisystem Inflammatory Syndrome in Children
Date published: November 2021
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 47 No. 11, November 2021: Multisystem Inflammatory Syndrome in Children
Epidemiologic studies
Descriptive analysis of a tuberculosis outbreak from a northern Saskatchewan First Nations community—December 2018 to May 2019
Nnamdi Ndubuka1,2, Braeden Klaver3, Sabyasachi Gupta1, Shree Lamichhane1, Leslie Brooks1, Shirley Nelson1, Grace Akinjobi1
Affiliations
1 Northern Inter-Tribal Health Authority, Prince Albert, SK
2 Community Health and Epidemiology, University of Saskatchewan, Saskatoon, SK
3 First Nations Health Authority, Vancouver, BC
Correspondence
Suggested citation
Ndubuka N, Klaver B, Gupta S, Lamichhane S, Brooks L, Nelson S, Akinjobi G. Descriptive analysis of a tuberculosis outbreak from a northern Saskatchewan First Nations community—December 2018 to May 2019. Can Commun Dis Rep 2021;47(11):479–84. https://doi.org/10.14745/ccdr.v47i11a07
Keywords: tuberculosis, outbreak, investigation, First Nations, Indigenous community, Saskatchewan, reserve, social network analysis, case finding
Abstract
Background: The tuberculosis (TB) incidence rate for northern Saskatchewan First Nations on-reserve is 1.5 higher than the national average. In December 2018 a member of one of these communities was diagnosed with 4+ smear-positive TB, spurring an outbreak investigation.
Objectives: To describe the public health response to TB outbreak investigation and highlight the risk factors associated with TB transmission in northern Saskatchewan; and to highlight the relevance of social network contact investigation tool in outbreak management.
Methods: Descriptive analysis included active TB cases and latent TB infection (LTBI) cases linked by contact investigation to the index case. Data were collected from active TB case files. Statistical analyses were performed and social network analysis conducted using household locations as points of contact between cases.
Results: A total of eight active TB cases and 41 LTBI cases were identified as part of the outbreak between December 2018 and May 2019. Half of the cases (4/8) were 25 to 34 years old, and five were smear negative. One-third of the people with LTBI were 15 to 24 years old, and about a half tested positive to the new tuberculin skin test (TST). The commonly reported risk factors for TB and LTBI cases were alcohol use, cigarette use, marijuana use, previous TB infection and homelessness. Social network analysis indicated a relationship between increased node centrality and becoming an active case.
Conclusion: Real-time social network contact investigation used in active-case finding was very successful in identifying cases, and enhanced nursing support, mobile clinics and mobile X-ray worked well as a means of confirming cases and offering treatment. TB outbreaks in northern Saskatchewan First Nations on-reserve communities are facilitated by population-specific factors. Efforts to implement context-specific interventions are paramount in managing TB outbreaks and preventing future transmission.
Introduction
Worldwide, tuberculosis (TB) is a major health problem with approximately 10 million people diagnosed in 2017 aloneFootnote 1. In response, the World Health Organization (WHO) has outlined a collaborative global effort to reduce TB incidence to less than 10 cases per 100,000 by 2035 Footnote 2. Incidence rates in Canada have remained relatively stable over the last decade, with 1,737 new cases of active TB reported in 2016Footnote 3, equating to an incidence rate of 4.8 per 100,000. However, the national rate does not accurately represent certain subsets of the Canadian populationFootnote 2Footnote 3.
TB incidence rates in Saskatchewan are continually above the national average, at 7.9 active TB cases per 100,000 in 2016Footnote 4. The same year there were 91 active cases of TB in Saskatchewan; 39 (43%) were in northern Saskatchewan, despite that only 3.6% of the province's population lives in this regionFootnote 4Footnote 5. Of the 39 cases in northern Saskatchewan, 31 were on-reserve First Nations; this equates to an incidence rate of 87.1 per 100,000 in this populationFootnote 4Footnote 6.
In Saskatchewan, all cases of active TB are reported by the local health authority to TB Prevention and Control Saskatchewan (TBPCS). Following diagnosis of active TB, contact tracing investigations are initiated to identify anyone who has been exposed for assessment and follow-up. Most of the northern Saskatchewan First Nations on-reserve population are managed by the Northern Inter-Tribal Health Authority (NITHA), who works with TBPCS as well as with the First Nations and Inuit Health Branch, Indigenous Services Canada.
In December 2018, a member of a NITHA community was diagnosed with 4+ smear-positive TB after being admitted to the hospital with severe complications related to TB. This person had been symptomatic for approximately eight months. Upon further investigation, it was found that they had been diagnosed with latent TB infection (LTBI) during a prior TB outbreak but had not completed treatment. It was concluded that this was a case of reactivation, not ongoing transmission, and could be considered to be an index case. The NITHA TB nurses immediately initiated contact tracing and social network contact investigation to identify exposed people. As of June 2019, an additional seven active TB cases and 41 LTBI cases with links to the index case had been diagnosed, prompting an outbreak investigation.
The objective of this report is to describe the sociodemographic and clinical characteristics of the outbreak cases as well as their risk factors and social network. The report also intends to highlight the integral public health interventions that helped mitigate the magnitude of this outbreak in a northern Saskatchewan First Nations on-reserve community.
Methods
Case identification
Both active and latent TB cases were included in this analysis. Cases were considered active if TB was confirmed clinically or in a laboratory or if the person had been potentially exposed to someone else with active TB, as identified through contact investigations. Laboratory confirmation required a culture, from sputum, body fluid or tissue that contains Mycobacterium tuberculosis complex. Clinical diagnosis includes a chest radiograph showing pulmonary changes indicative of TB, or histopathologic evidence of active TB, or response to anti-TB treatment, or active non-respiratory TB symptoms.
LTBI cases met the following requirements: a tuberculin skin test (TST) that confirms the presence of M. tuberculosis; no evidence of clinically active disease; no radiographic changes suggestive of active disease; negative microbiologic tests (if performed); and potential exposure to an active TB case from the outbreak.
Data collection
We extracted data from case files completed by TB nurses during case and contact investigations and follow-up assessments. The information in the case files included data on sociodemographic variables, clinical characteristics, risk factors, social networks and public health interventions.
Sociodemographic variables included age and sex, while the clinical characteristics included site of infection, sputum smear status, TST status and treatment status. Risk factors included cigarette use, alcohol use, marijuana use, homelessness and comorbidities. Social network data comprised the connections between active TB cases, LTBI cases and exposed households. We assessed public health interventions using data on case detection methods, numbers of individuals assessed, cases started on treatment and healthcare access.
Data analysis
Descriptive analysis of the outbreak cases was performed using statistical package R version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria), and the epidemic curve was created in Excel version 2019 (Microsoft Corp., Redmond, Washington, United States). Active TB cases and LTBI cases were separated for the purposes of the analysis. The cases were described using proportions for each of the sociodemographic, clinical and risk factor variables assessed.
Social network analysis was conducted using the software program Gephi version 0.9.2 (Gephi Consortium, Compiegne, France). All people with active TB and LTBI were linked to the households they were known to visit, stay with or live with during the periods of infectivity. Averages on the number of edges for households and cases were also calculated.
Interventions were assessed using basic descriptive statistics of relevant indicators, which included both proportions and averages calculated in statistical package R.
Results
Eight active TB cases and 41 LTBI cases diagnosed between December 2018 and May 2019 met the inclusion criteria for the outbreak. The epidemic curve illustrates the amplification in cases following the diagnosis of the index case with a 4+ smear-positive TB infection on December 13, 2018 (Figure 1). All 8 active TB cases had been diagnosed by March 2019, while the number of LTBI cases diagnosed increased steadily to a peak of 15 cases in March and then declined noticeably.
Figure 1: Epidemic curve of a tuberculosis outbreak in a northern Saskatchewan First Nations on-reserve community, between December 2018 and May 2019
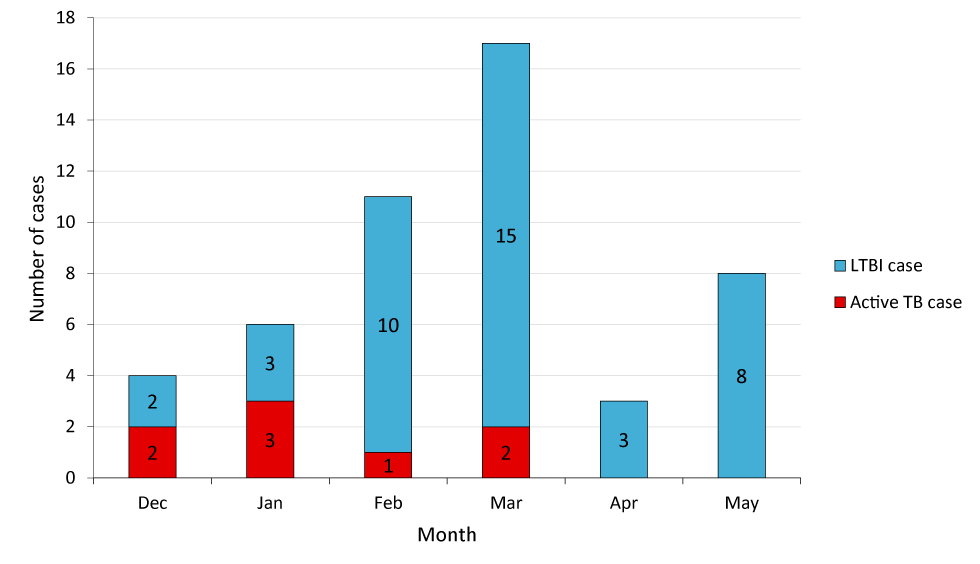
Text description: Figure 1
The graph shows the total number of active TB and LTBI cases reported to Northern Inter-Tribal Health Authority (NITHA) public health between December 2018 and May 2019. An average of two active cases per month were reported between December 2018 and March 2019. The number of LTBI cases increased rapidly from two cases in December 2018 to a maximum of 15 cases in March 2019.
Sociodemographic and clinical characteristics
Six of the eight people with active TB were male, and four were 25 to 34 years old (Table 1). Six were new TST positive test performed for the first time had a positive result, and only two were diagnosed with 4+ smear-positive TB. Six were diagnosed with pulmonary TB; two had TB lymphadenitis. All started the prescribed treatment.
| Variables | Cases with active TB (n=8) | Cases with LTBI (n=41) | |||
|---|---|---|---|---|---|
| Number | %Table 1 footnote a | Number | %Table 1 footnote a | ||
| Sex | Male | 6 | 75 | 20 | 49 |
| Female | 2 | 25 | 21 | 51 | |
| Age group | <5 | 1 | 13 | 2 | 5 |
| 5–14 | 1 | 13 | 5 | 12 | |
| 15–24 | 2 | 25 | 14 | 34 | |
| 25–34 | 4 | 50 | 8 | 20 | |
| 35–44 | 0 | 0 | 5 | 12 | |
| 45–54 | 0 | 0 | 4 | 10 | |
| 55–64 | 0 | 0 | 1 | 2 | |
| 65+ | 0 | 0 | 2 | 5 | |
| TST statusTable 1 footnote b | New TST positive | 6 | 75 | 23 | 56 |
| Past TST positive | 2 | 25 | 18 | 44 | |
| Bacteriological status | Smear positive, culture positive | 2 | 25 | 0 | 0 |
| Smear negative, culture positive | 5 | 63 | 0 | 0 | |
| Smear negative, culture negative | 0 | 0 | 34 | 83 | |
| No bacteriological confirmation | 1 | 13 | 7 | 17 | |
| Site of infection | Pulmonary | 6 | 75 | N/A | N/A |
| Lymphatic | 2 | 25 | N/A | N/A | |
| Treatment | Yes | 8 | 100 | 31 | 76 |
| No/declined | 0 | 0 | 7 | 17 | |
Equal portions of the people with LTBI were males (20/41; 49%) and females (21/41; 51%). The majority were 15 to 24 years old (14/41; 34%), and slightly over half were new TST positive (23/41; 56%). Only a few (7/41; 17%) declined treatment, on the recommendation of physicians, because of potential complications with other medications or pregnancy.
Risk factor analysis
People with active TB had a high prevalence of risk factors; five used cigarettes and alcohol and four used marijuana (Table 2). Two of those who did not use any substances were less than 15 years old. Two were experiencing homelessness; of note, one was the index case. Only two had had previous TB infection.
| Variables | Cases with active TB (n=8) | Cases with LTBI (n=41) | |||
|---|---|---|---|---|---|
| NumberTable 2 footnote a | %Table 2 footnote b | NumberTable 2 footnote a | %Table 2 footnote b | ||
| Experiencing homelessness | Yes | 2 | 25 | 4 | 10 |
| No | 6 | 75 | 37 | 90 | |
| Comorbidity | Diabetes | 0 | 0 | 1 | 2 |
| Previous TB infection | 2 | 25 | 16 | 39 | |
| Both | 0 | 0 | 2 | 5 | |
| None | 6 | 75 | 21 | 51 | |
| Cigarette use | Yes | 5 | 63 | 24 | 58 |
| No | 3 | 38 | 16 | 39 | |
| Alcohol use | Yes | 5 | 63 | 23 | 56 |
| No | 3 | 38 | 17 | 41 | |
| Marijuana use | Yes | 4 | 50 | 16 | 39 |
| No | 4 | 50 | 24 | 59 | |
People with LTBI had prevalence of risk factors similar to the active cases, with more than half (23/41) reporting using cigarettes and alcohol. Over one-third (16/41; 39%) reported using marijuana, and four were experiencing homelessness (10%). Two (5%) had had prior TB infection and diabetes; 16 (39%) had been previously diagnosed with a TB infection.
Social network analysis
Social network contact investigation successfully identified 39 (80%) of the 49 people with TB and LTBI (Table 3). The social network includes 62 nodes altogether: 13 exposed households (21%) and 49 cases (79%). There were an average of 9.4 edges per household and 2.5 edges per case.
| Variables | Case count | ||
|---|---|---|---|
| n | % | ||
| Method of detection of cases | Symptoms | 1 | 2 |
| Traditional contact investigation | 9 | 18 | |
| Social network contact investigation | 39 | 80 | |
| Nodes | Households | 13 | 21 |
| Cases | 49 | 79 | |
| Edges | Total | 122 | 100 |
The social network map (Figure 2) illustrates the many potential TB transmission pathways. The person identified as the index case, who was experiencing homelessness, was highly transient and central to the network, exposing nine different households. Of note, active TB cases have higher connectivity in the network than LTBI cases, with an average of 4.3 edges per node compared to 2.1 edges per node for LTBI cases.
Figure 2: Social network analysis of a tuberculosis outbreak in a northern Saskatchewan First Nations on-reserve community
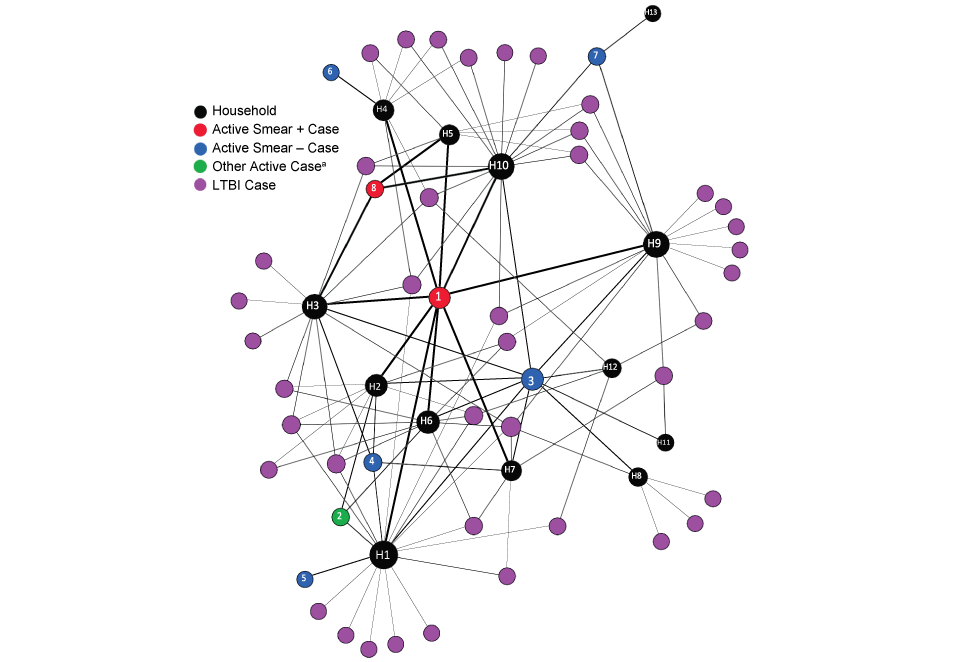
Text description: Figure 2
Figure shows the real time social network analysis of case investigation for this TB outbreak.
Within the diagram, bigger node size represents the centrality of the household involved whereas thickness of the edges reflects the level of infectivity of a case. The index case exposed nine different households, among them household 1 was found linked to the highest number of secondary active TB cases and LTBI cases (n=18) as this location was frequently visited by the homeless and other people of young age group. Households 2, 3, 6, 9 and 10 were identified each linked with over ten individuals as these households served as the places for partying, socialization, and other gatherings. Out of eight active cases, one active case was not bacteriologically confirmed (green).
Certain network households appear to be key points of exposure and transmission from the index case, as Household 1 had connections to four secondary active TB cases and 14 LTBI cases; Household 1 was frequented by people experiencing homelessness and young families. In addition, Households 2, 3, 6, 9 and 10 are each connected to over 10 people within the network; together they have an average of 13.4 connected cases. These households are known to be key gathering points in the social network, serving as places for socialization, partying or card playing.
Public health interventions
Real-time social network contact investigation was used for the first time in a NITHA community to enhance case finding. In total, 136 individuals were involved in this outbreak investigation; 109 (80%) were identified through social network contact investigation while 26 (20%) were found during routine contact tracing interviews.
Integral to the management of the outbreak was follow-up, with TB nurses and TB physicians completing TSTs, symptom inquiries and clinical assessments. A total of 135 contacts were identified over a five-month period. In response to the influx of individuals, NITHA began sending two nurses per community visit, instead of one, until the community hired two part-time TB nurses to support management efforts. Mobile clinics were increased from every two months to monthly to decrease wait times for physician and mobile X-ray assessments.
Seven people (14%) declined treatment due to pregnancy or potential interactions with other medications. For the individuals who accepted treatment, the current practice in NITHA communities was to provide directly observed therapy (DOT) to improve medication adherence. As a result, it was decided to hire one additional full-time TB community worker and one part-time TB community worker to allow all of the new cases to begin treatment upon diagnosis.
In addition, TBPCS required that all children younger than five years old who were identified as potentially exposed be placed on window period prophylaxis (WPP) within two weeks of identification. In this outbreak 22 children in this age group were placed on WPP in this time-frame until final diagnosis.
Discussion
The findings from this outbreak highlighted the important factors related to TB transmission in a northern Saskatchewan First Nations on-reserve community. Of note, the outbreak cases were primarily young adults and most had a new TST positive result. Pulmonary infections were the most common manifestation of active TB, and the majority of cases were smear negative. Outbreak cases had a high prevalence of known risk factors, such as cigarette, alcohol and marijuana use. An important finding was the impact of homelessness on the outbreak, as six outbreak cases identified as being homeless, including the index case.
Social network analysis showed the complexity of the social networks and the importance of shared locations in a northern Saskatchewan First Nations on-reserve community. The high average number of households visited per case indicated the nature of transiency and pronounced socialization behaviour. In addition, there appeared to be a correlation between the level of connectivity to exposed households and having active TB or LTBI. Social network analysis also revealed the substantial amount of transmission between the index case and others.
The findings from this outbreak reflect current understanding of TB epidemiology in First Nations populations with regard to age, sex and location of diseaseFootnote 7; however, the rates of smear-positivity among active outbreak cases were much lower than expected. This low rate of smear-positivity likely reflects the enhanced case-finding, which facilitated earlier diagnosis.
The high prevalence of known risk factors among individuals identified as having active TB and LTBI in this outbreak may help explain its size and intensity. Substance use is known to suppress the immune system, increasing the likelihood of acquiring TB infection and progression to active TB diseaseFootnote 7Footnote 8Footnote 9Footnote 10. In addition, homelessness can be a critical factor in some TB outbreaks, as people experiencing housing insecurity are known to have multiple challenges, including access to health care and managing competing priorities that can hinder health-seeking behavioursFootnote 11Footnote 12Footnote 13. Investigations in this outbreak found that the index case had challenges accessing health care as a result of homelessness. The individual couch-surfed in several households, which lead to disease transmission or potential transmission to a number of people who lived or socialized there.
Despite the high rate of diabetes in First Nations populations and the associated increased risk of TB infection, its impact on the outbreak was minimalFootnote 7Footnote 14. Moreover, although prior TB infection is considered to reduce the likelihood of reacquiring TBFootnote 7Footnote 15, in the context of this outbreak, most past-positive individuals were considerably exposed and therefore required reassessment.
Results from the social network analysis echoed other findings, including the relationship between increased TB exposure and the likelihood of TB transmission and progressionFootnote 7Footnote 14. Furthermore, the importance of location of households as it relates to transmission in an on-reserve setting was emphasized in this outbreak, providing further support to previous findingsFootnote 13Footnote 16.
The implementation of social network contact investigation proved highly successful as it identified the majority of exposed individuals. Our results reflect the current understanding that social network contact investigation is a proven tool in settings where social stigma, high transiency, high degree of socialization and/or large numbers of exposed contacts exist Footnote 7Footnote 13Footnote 16. In contrast, traditional methods of contact investigation proved to be poor at identifying exposed individuals.
Despite the large influx of individuals, follow-up and treatment were major strengths during this outbreak. Understaffing and difficulty accessing health care is a common challenge on remote First Nations reservesFootnote 7Footnote 17; however, community capacity was increased following the start of the outbreak. Outbreak management efforts were also able to meet key management indicators outlined in the TB standards; these included all LTBI cases starting or being offered treatment and contact investigations being conducted within seven calendar days and contact follow-ups within 28 calendar daysFootnote 7. Furthermore, all eligible LTBI cases accepted and were placed on treatment immediately following diagnosis, which is well above the current recommendation of 80%Footnote 7Footnote 18. Individuals in the community received DOT, a typical mode of treatment in challenging populationsFootnote 7Footnote 19 The guideline on window prophylaxis, as outlined in the TB standards, was also followed exhaustively with all children younger than five years oldFootnote 7.
Conclusion
TB outbreak interventions in unique populations, such as First Nations reserves, must consider context-specific challenges prior to their implementation, for example, population-specific demographics and risk factors of TB transmission. The high level of transiency between households in First Nations communities is an important factor to consider when conducting case findings, especially with people experiencing homelessness. Proactively tailoring management initiatives allows for greater outbreak management success and ultimately outbreak prevention in the future. Real-time social network contact investigation is an essential tool to enhance active case finding during outbreak investigation.
Authors' statement
- BK — Conceptualization, data extraction and analysis, visualization, writing–original draft, writing–review & editing
- SG — Conceptualization, writing–review & editing
- GA — Conceptualization, writing–review & editing, supervision
- SL — Writing–review & editing
- LB — Investigation
- SN — Investigation
- NN — Conceptualization, investigation, writing–review & editing, supervision
The content and view expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests
None.
Acknowledgements
We would like to thank the Northern Inter-Tribal Health Authority and community tuberculosis (TB) nurses involved in case finding and data collection for this outbreak. We would also like to thank TB Prevention and Control Saskatchewan for their role in providing additional details on missing data from the case files and updating the case status for many of the outbreak individuals. Lastly, we would like to thank the community for allowing us to use their data for the purposes of this report.
Funding
None.
