COVID-19 in Québec, Canada

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 48-4, April 2022: First Nations Health
Date published: April 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-4, April 2022: First Nations Health
Epidemiologic Study
Impact of the first vaccine dose on COVID-19 and its complications in long-term care facilities and private residences for seniors in Québec, Canada
Élise Fortin1,2,3, Philippe De Wals1,2, Denis Talbot2, Manale Ouakki1, Geneviève Deceuninck1,4, Chantal Sauvageau1,2, Rodica Gilca1,2,4, Marilou Kiely1,4, Gaston De Serres1,2,4
Affiliations
1 Direction des risques biologiques et de la santé au travail, Institut national de santé publique du Québec, Québec, QC
2 Département de médecine sociale et préventive, Faculté de médecine, Université Laval, Québec, QC
3 Département de microbiologie, infectiologie et immunologie, Faculté de médecine, Université de Montréal, Montréal, QC
4 Centre de Recherche du CHU de Québec - Université Laval, Québec, QC
Correspondence
Suggested citation
Fortin É, De Wals P, Talbot D, Ouakki M, Deceuninck G, Sauvageau C, Gilca R, Kiely M, De Serres G. Impact of the first vaccine dose on COVID-19 and its complications in long-term care facilities and private residences for seniors in Québec, Canada. Can Commun Dis Rep 2022;48(4):164–9. https://doi.org/10.14745/ccdr.v48i04a07
Keywords: COVID-19, vaccination, impact, public health, long-term care
Abstract
Background: Residents of long-term care facilities (LTCFs) and private residences for seniors (PRSs) were given priority for vaccination against coronavirus disease 2019 (COVID-19). Given the shortage of vaccine in the winter of 2021, the Comité sur l'immunisation du Québec recommended postponing the administration of second doses to ensure more rapid and widespread administration of first doses. The objective of this study was to measure the impact of first-dose vaccination on 1) the incidence of cases and complications in LTCFs and PRSs and 2) the frequency of outbreaks in LTCFs.
Methods: In this ecological study, COVID-19 incidence and complications in residents of LTCFs and PRSs in Québec were compared with the general (community) population at a point in time when there was still only limited eligibility for vaccination.
Results: After vaccination in LTCFs, the incidence rate of COVID-19 decreased by 92% compared with 49% in the community, and deaths decreased by 95%. By six weeks post-vaccination, almost no facility reported five or more cases per 100 beds per week. The incidence rate decreased by 91% in PRSs compared with 2% in the community. Hospitalizations and deaths in PRSs decreased by 94% and 90%, respectively.
Conclusion: As a result of 1) vaccination of residents with one dose, 2) natural immunity already acquired in LTCFs and PRSs, 3) vaccination of healthcare workers and 4) other non-pharmaceutical prevention measures implemented, the circulation of the coronavirus in these settings was largely interrupted.
Introduction
Between March 1, 2020, and February 15, 2021, coronavirus disease 2019 (COVID-19) affected more than 2,500 long-term care facilities (LTCFs) or private residences for seniors (PRSs) in Canada, causing more than 55,000 infections in residents (over approximately 830,000 total cases in Canada), of which nearly 15,000 died (over approximately 21,000 total deaths in Canada, all ages)Footnote 1Footnote 2. In Québec, elderly or frail people frequently move into PRSs or LTCFsFootnote 3. This population has been particularly affected by COVID-19, representing only 2% of the Québec population but accounting for 12% of all cases (n=19,838/163,744), 32% of hospitalizations (n=4,248/13,280) and 56% of deaths related to COVID-19 (n=4,292/7,631) as of December 12, 2020 (data from the Ministère de la Santé et des Services sociaux; Infocentre de santé publique).
Limited quantities of the first COVID-19 vaccines were delivered to Canada in early December 2020. On January 12, 2021, the National Advisory Committee on Immunization recommend delaying the administration of the second dose of vaccine until 42 days after the first dose, rather than the 21–28 days advocated by manufacturersFootnote 4. On March 3, 2021, the National Advisory Committee on Immunization increased their recommended timeframe for administration of second dose to four months, bringing all provinces and territories into complianceFootnote 5. In Québec, the COVID-19 vaccination campaign began on December 14, 2020 and an unlimited interval extension between vaccinations was adopted as of December 31, 2020Footnote 6. The first priority group for vaccination was LTCF residents, followed by healthcare workers and people living in PRSsFootnote 7. Additional non-pharmaceutical measures were implemented, including another lockdown for the general population and tightening of measures in isolated and confined living environmentsFootnote 8Footnote 9Footnote 10.
The objective of the study is to measure the impact of first-dose vaccination on the incidence and complications of COVID-19 in LTCFs and PRSs and on the frequency of outbreaks in LTCFs.
Methods
Study design and population
This ecological study involved all residents of LTCFs (42,002 beds registered in the M02 Directory of Institutions of the Ministère de la Santé et des Services sociaux) and PRSs (129,626 residents), who were compared with the rest of the Québec population ("general" or "community" population, excluding healthcare workers) based on the registry of persons insured by the Régie de l'assurance maladie du Québec (comprising 7,991,678 inhabitants)Footnote 11Footnote 12. Healthcare workers (n=354,038) excluded from the community population included physicians and employees from the health and social services network, on the payroll of public and private institutions; community pharmacists and research personnel were not excluded. Thirty-six LTCFs (with a total of 2,510 registered beds) which mission was not focussed on seniors were excluded from the analyses as they were not given priority in the vaccination campaign. The observation period was from August 23, 2020 to April 10, 2021.
Variables
Data on COVID-19 cases (symptomatic and non-symptomatic cases, hospitalizations and deaths, date of episode, living environment, name of the LTCF of residence and healthcare worker status) were extracted from the provincial electronic file of confirmed COVID-19 cases (Trajectoire de santé publique platform, accessed at the Infocentre de santé publique) on April 25, 2021 for the LTCF analyses and on June 15, 2021 for the PRS analysis. The Trajectoire de santé publique platform is the only database documenting all laboratory-confirmed and epidemiologically-linked cases of COVID-19 in Québec and is therefore the gold standard. It is supported by surveys conducted by regional public health departments, which report, among other things, basic demographic data on cases, their living environment (home/LTCF/PRS/other, name of facility and address) and whether they are healthcare workers. The platform has not undergone validity studies; however, cases occurring in LTCFs and PRSs are investigated on a priority basis and are therefore very well documented, whereas non-severe cases in the rest of the population are underestimated since their reporting depends on individuals' propensity to consult or be screenedFootnote 13. In contrast, hospitalized or deceased COVID-19 cases are much better captured. The list of facilities with a LTCF mission was developed from the Ministère de la Santé et des Services sociaux directory of institutions, which contains the number of licenced beds for each LTCFFootnote 11. Information on the progress of vaccination coverage in each of the three groups was extracted from the Registre de vaccination du Québec—a population-based registry consulted at the Infocentre de santé publique, which is the only source for such dataFootnote 12. Doses must be entered into the registry within hours of administration. The LTCF and PRS residents were identified by their address as declared to the Régie de l'assurance-maladie du Québec and by the justification for their vaccination.
First-dose vaccination of LTCF residents began in December 2020, but occurred primarily in January 2021, with coverage increasing from 17% to 80% between January 5 and 20, 2021. Similarly, the majority of PRS residents were vaccinated between February 10 and 28, 2021, when coverage increased from 18% to 80%. The administration of second doses in LTCFs and PRSs began on April 22, 2021. As of April 10, 2021, 91% of LTCF residents and 92% of PRS residents were vaccinated with at least one dose. Vaccination with a first dose for the community population began sequentially in March 2021, but as of April 10, 2021, only a minority of this group (19%) had been reached.
Analyses
The number of cases occurring in each group (LTCF, PRS, and general population) was calculated and presented according to the episode date (the date of onset of symptoms when available, otherwise the sampling date or the reporting date if neither of these two dates was available). Differences in daily pre/post-vaccination incidence rates were calculated by comparing the period December 1 to 31, 2020 vs February 17 to April 10, 2021 for LTCFs and January 1 to 31, 2021 vs March 28 to April 10, 2021 for PRSs. The buffer period between the pre/post-vaccination periods included both the vaccination and the subsequent 28 days required for the vaccines to reach their full effect. The same analysis was done for hospitalizations and deaths; however, because LTCF residents had access to health care in their living environments, we did not analyze the hospitalization trends in this population. Finally, the number of cases per 100 beds was calculated by LTCF and by CDC week before or after the start of vaccination in the LTCF to identify the number of "affected" (defined as at least one case per week) and "more severely affected" (defined as at least five cases per 100 beds) LTCFs per week. This calculation was used as an approximation of outbreaks. This calculation was not possible for PRSs since the information was not available.
Results
Long-term care facilities
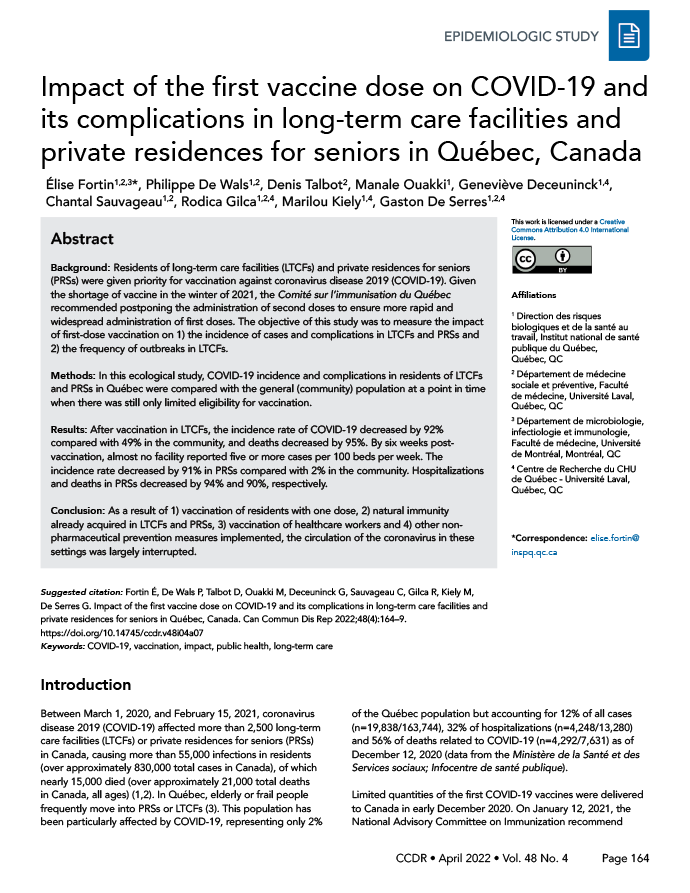
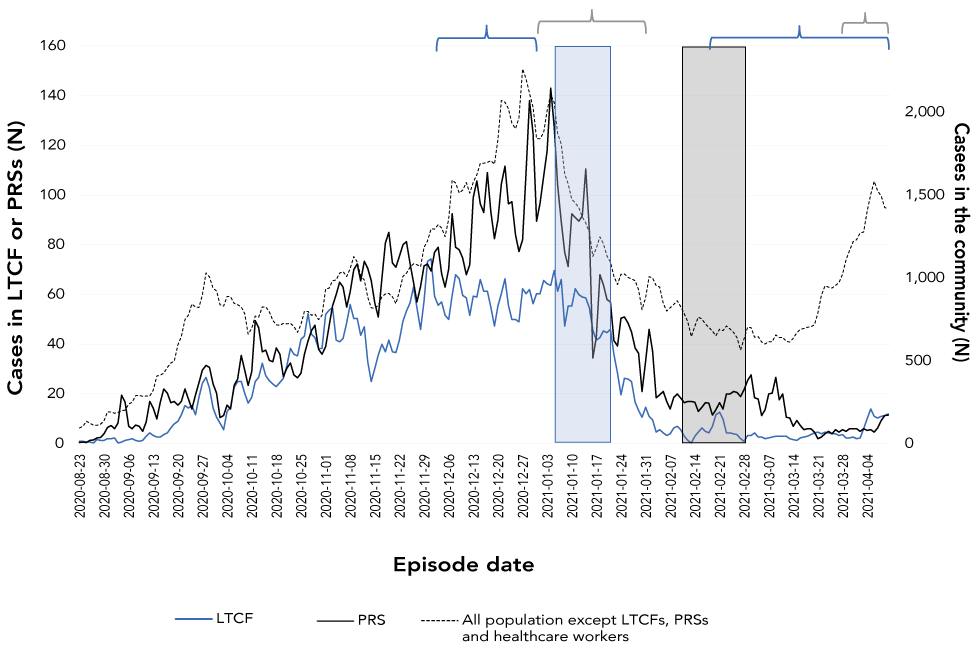
Between August 23, 2020 and April 10, 2021, 6,027 cases of COVID-19 were reported among residents in the 418 LTCFs that were tracked; 1,723 (29%) of these cases died. There was a gradual increase in the incidence of cases during the fall of 2020, both in LTCFs and in the community (Figure 1). In the community, incidence began to decline in very early January 2021, reaching a low point between mid-February and mid-March 2021 and rising again during the third wave. The pattern was significantly different in the LTCFs, where a much steeper decline began on January 10, 2021, reaching a very low plateau during the entire month of March before increasing only slightly again during the first two weeks of April 2021. The same trend was observed for deaths (Figure 2). During the post-vaccination period (February 17–April 10, 2021), the incidence rate had decreased by 91.8% in the LTCF and 48.9% in the community (general population; excluding LTCFs, PRSs and healthcare workers) compared with December 2020 (Table 1).
Figure 1: Cases in long-term care facilities, private residence for seniors and among the general populationFigure Footnote a, August 23, 2020–April 10, 2021
Text description: Figure 1
Three-day moving average. The blue window shows the intensive vaccination period in CHSLDs and the grey window shows the period in RPAs. The blue brackets show the pre- and post-vaccination periods used to measure the impact in CHSLDs; for RPAs, these periods are indicated by the grey brackets.
Figure 2: Deaths in long-term care facilities, private residences for seniors and among the general populationFigure Footnote a, August 23, 2020–April 10, 2021
Text description: Figure 2
Three-day moving average. The blue window shows the intensive vaccination period in CHSLDs and the grey window shows the period in RPAs. The blue brackets show the pre and post-vaccination periods used to measure the impact in CHSLDs; for RPAs, these periods are indicated by the grey brackets.
Outcome |
LTCFs (rate per 100,000 person-days) |
General population (rate per 100,000 person-days) |
||||
|---|---|---|---|---|---|---|
| Pre-vaccination | Post-vaccination | Difference (%) |
Pre-vaccination | Post-vaccination | Difference (%) |
|
| Cases | 138.6 | 11.4 | -91.8 | 21.4 | 10.9 | -48.9 |
| Deaths | 37.6 | 1.9 | -94.9 | 0.2 | 0.1 | -73.0 |
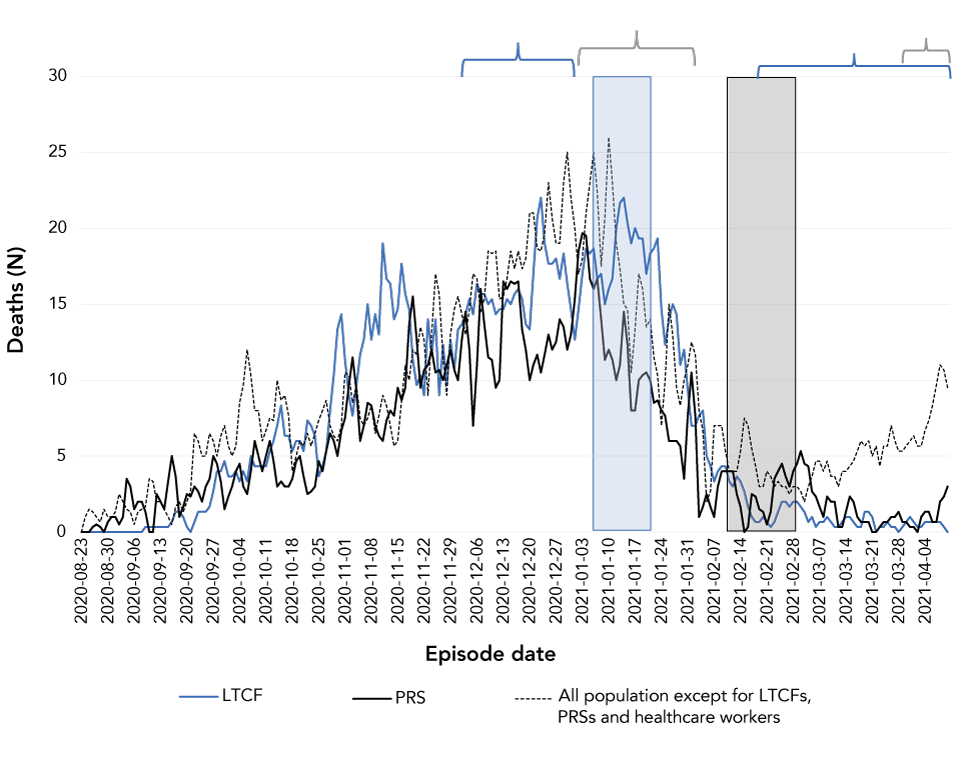
For the same periods, the mortality rate decreased by 94.9% in LTCFs and 73.0% in the community. The number of LTCFs affected (defined as at least one case) or reporting at least five cases per 100 beds decreased beginning in the second and third weeks after the vaccination blitzes (Figure 3); these numbers stabilized beginning in the sixth week after vaccination, when approximately 10 LTCFs were affected each week, with none or only one LTCFs more severely affected.
Figure 3: Number of long-term care facilities affected, based on the number of cases per 100 users, per week before or after the start of the vaccination
Text description: Figure 3
Week zero corresponds to the week in which vaccination began in a CHSLD, in calendar time; this week is not the same for all CHSLDs.
Private residences for seniors
Over the entire observation period, 9,396 cases of COVID-19 were reported in PRSs; of these cases, 2,412 (26%) were hospitalized and 1,359 (14%) died. The decrease in PRS cases occurred in two stages (Figure 1). The largest decrease occurred from early January to mid-February, when few vaccines had been administered. A resurgence of cases occurred from late February to early March, then declined again to levels not seen since the very beginning of September 2020. The cases in the comparison group followed approximately the same pattern up to that point. The impact of vaccination in PRSs became more apparent toward the end of March, as cases increased substantially in the comparison population, while cases in PRSs reached a low plateau, without a substantial increase at the end of the period. Hospitalizations and deaths followed the same temporal trends as cases (Figure 2 and Figure 4). The incidence rate in PRSs decreased by 91% between January 2021 and the post-vaccination period (March 28–April 10, 2021), whereas the decrease was only 2% in the general population (Table 2). Post-vaccination hospitalization and mortality rates for PRS residents had decreased by 94% and 90% compared to January, while these decreases were 7% and 53%, respectively, in the community.
Figure 4: Hospitalizations in private residences for seniors and in the general population excluding long-term care facilities, private residences for seniors and healthcare workers, August 23, 2020–April 10, 2021
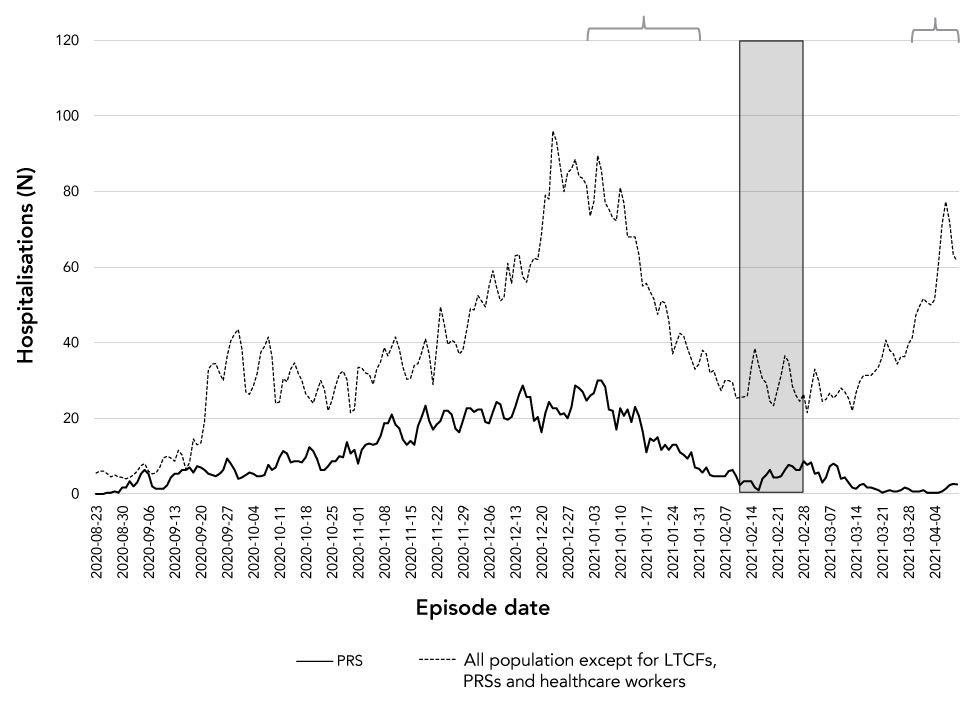
Text description: Figure 4
Three-day moving average. The gray window shows the intensive vaccination period in RPAs; the gray brackets show the pre- and post-vaccination periods used to measure impact in RPAs.
| Outcome | PRS (rate per 100,000 person-days) |
General population (rate per 100,000 person-days) |
||||
|---|---|---|---|---|---|---|
| Pre-vaccination | Post-vaccination | Difference (%) |
Pre-vaccination | Post-vaccination | Difference (%) |
|
| Cases | 56.0 | 5.0 | -91.0 | 16.9 | 16.7 | -1.6 |
| Hospitalizations | 13.6 | 0.8 | -93.8 | 0.8 | 0.7 | -6.5 |
| Deaths | 8.6 | 0.8 | -90.2 | 0.2 | 0.1 | -52.6 |
Discussion
This study measured the impact of the first-dose of the vaccination campaign in Québec LTCFs and PRSs, that is, a combination of vaccine efficacy, vaccine coverage and an additional reduction in virus transmission via herd immunity. Rapid vaccination of residents was followed by a significant decrease in cases (91% in LTCFs and 92% in PRSs), hospitalizations (94% in PRSs), deaths (95% in LTCFs and 90% in PRSs) and outbreaks related to COVID-19 in these settings. The decrease was maintained until the administration of the second and even the third dose in October 2021 (data from the Trajectoire de santé publique platform). Improvement in the community case counts, hospitalizations and deaths also occurred in January and February 2021, but to a lesser extent, and were followed by increases during the third wave of COVID-19 in April 2021.
In LTCFs, vaccination blitzes were followed by a 91% reduction in the infection incidence rate among residents compared with a 49% reduction among the community population. This important decrease in cases and disease severity in LTCFs is most likely attributable to vaccination. In addition, while cases increased again in the community during the third wave in Québec, cases in LTCFs remained low. The number of deaths followed the same trend. In Ontario, where second doses were administered promptly in LTCFs, a similar decrease in incidence rates was observed eight weeks after the start of vaccinationFootnote 14. We also note that after vaccination, almost no LTCF was severely affected (five or more cases/100 beds) despite the occurrence of sporadic cases, which suggests the existence of herd immunity generated by the vaccination in a substantial proportion of the residents and the workers in these settings. A study in Catalonia, Spain, showed a maximum decrease of 90% (95% CI: 76–93) between expected and observed cases six weeks after 70% of residents received a second dose Footnote 15. Our data suggest that a comparable outcome was achieved with a single dose of the vaccine.
In PRSs, the large decrease in the number of cases, which started before resident vaccination began, is likely related to the reduction in transmission in the general population resulting from general non-pharmaceutical public health measures implemented in late December 2020, the vaccination of healthcare workers and the tightening of prevention measures instituted in PRSs after the December holiday season. The impact of vaccination of residents seems clear during the third wave, which was caused primarily by the Alpha variant (B.1.1.7). This wave greatly affected unvaccinated persons in the community, leading to another lockdown in some areas; but PRSs were almost completely spared.
Strengths and limitations
A major strength of this study is that it is a population—based study—there was no random error, as the differences reported were those observed in the target population as a whole-and the trends are very clear. Nevertheless, in addition to the other measures and phenomena concomitant with resident vaccination mentioned in the introduction, this ecological study has some limitations. The provincial registry of COVID-19 cases is intended to record all cases reported to public health authorities, but cases that did not result in an epidemiological investigation were not included. An underestimation of cases in LTCFs and PRSs is possible, especially before vaccination when the high incidence of cases led to an overload of work for the teams responsible for the surveys and a prioritization of the information to be captured. The living environment (home/LTCF/PRS/other, name of facility and address), however, continued to be important information. The impact of a first dose may have been underestimated since the post-vaccination period began four weeks after 80% coverage had been achieved, whereas vaccine coverage is now over 95%. Since LTCFs and PRSs were severely affected by COVID-19 prior to vaccination, for many residents, the first dose of vaccine was in addition to natural immunity. The unknown role of these factors may reduce the reproducibility of this study. It should be noted that an ecological design was entirely appropriate for measuring the impact of a vaccination campaign in the target population in order to capture data reflective of herd immunity as well. Finally, while it would have been interesting to measure the impact of age and health status of the residents and type of facility, this information was not available. Furthermore, it was not necessary, since it would be unlikely that the composition of the study population had changed significantly between the pre- and post-vaccination periods.
Conclusion
Although the vaccination of healthcare workers and the enhanced preventive public health measures instigated in early 2021 likely reduced the transmission of COVID-19, administration of the first dose of vaccine to the residents in the LTCFs and PRSs appears to have contributed to the marked decrease in COVID-19 incidence, hospitalizations and mortality in these settings—even before the second dose was administered.
Authors' statement
- EF — Conceptualization, data analysis and interpretation, writing or revising the article
- PDW — Conceptualization, data analysis and interpretation, writing or revising the article
- DT — Conceptualization, data analysis and interpretation, writing or revising the article
- MO — Data analysis and interpretation, writing or revising the article
- GD — Conceptualization, data analysis and interpretation, writing or revising the article
- CS — Conceptualization, writing or revising the article
- RG — Data analysis and interpretation, writing or revising the article
- MK — Conceptualization, writing or revising the article
- GDS — Conceptualization, data analysis and interpretation, writing or revising the article
The contents and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests
GDS was awarded a research grant from Pfizer. RG received an honorarium from McMaster RSV Coordinators Workshop funded by AbbVie. The other authors and reviewers reported no actual, apparent or potential conflicts of interest.
Acknowledgements
None.
Funding
This work was carried out with the support of the Ministère de la Santé et des Services sociaux du Québec. DT is supported by a career grant from the Fonds de recherche du Québec - Santé.
