Acute histoplasmosis in four immunocompetent Canadian travellers to a cenote in Yucatán

 Download this article as a PDF (127 KB)
Download this article as a PDF (127 KB)Published by: The Public Health Agency of Canada
Issue: Volume 51-5, May 2025: Travel Health
Date published: May 2025
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 51-5, May 2025: Travel Health
Case Series
Acute histoplasmosis in four immunocompetent Canadian travellers to a cenote in Yucatán, Mexico
Elspeth MacBain1, Michael Hawkes1, David Goldfarb2, Jan Hajek3
Affiliations
1 Department of Pediatrics, University of British Columbia, Vancouver, BC
2 Department of Pathology and Laboratory Medicine, University of British Columbia, Vancouver, BC
3 Department of Infectious Diseases, University of British Columbia, Vancouver, BC
Correspondence
Suggested citation
MacBain E, Hawkes M, Goldfarb D, Hajek J. Acute histoplasmosis in four immunocompetent Canadian travellers to a cenote in Yucatán, Mexico. Can Commun Dis Rep 2025;51(5):187–90. https://doi.org/10.14745/ccdr.v51i05a05
Keywords: histoplasmosis, travel medicine, fever in returned traveler, endemic fungi
Abstract
A group of four healthy Canadian travellers visited a cenote in the Yucatán peninsula in April 2024 and subsequently developed symptomatic histoplasmosis. Diagnosis was made in the acute period with a positive urine Histoplasma antigen test in three of the cases. Two developed severe presentations and were treated with itraconazole, including a three-year-old child with disseminated disease. The sensitivity of different modalities for diagnostics depends on the timing and severity of illness, with Histoplasma urine antigen being most sensitive in early infection, serology converting 4–8 weeks following exposure and cultures generally of low sensitivity. Treatment depends on the disease manifestations and host immunologic status. Many patients have relatively mild, self-limited, influenza-like illness and the diagnosis may be overlooked. Given the number of Canadian tourists travelling to the Yucatán peninsula and the popularity of visiting cenotes, awareness of the risk of histoplasmosis associated with this exposure should be promoted.
Introduction
Histoplasmosis is a fungal infection caused by inhalation of the microconidia of Histoplasma capsulatum. It is endemic in various regions across the world and is classically associated with exposure to bat and bird excrement. In Canada, Histoplasma is endemic along the St. Lawrence Seaway in Ontario and Québec and recent case reports have described local acquisition in Alberta and Saskatchewan Footnote 1. Histoplasma is well known to be regionally endemic in the Ohio and Mississippi River Valleys of central and eastern United States and common in Mexico, Central and South America, several regions in Africa and South East Asia Footnote 1.
Infection is often asymptomatic, with population seroprevalence in some endemic areas as high as 80% Footnote 2; however, histoplasmosis can have a spectrum of clinical manifestations ranging from mild self-limited influenza-like-illness, to severe pneumonia and disseminated disease Footnote 3. Symptoms typically begin 1–3 weeks following exposure Footnote 4. Young children, immune-compromised hosts and the elderly are at higher risk of severe disease. A number of cases of histoplasmosis have been described in immunocompetent travellers to endemic areas, often in association with exposure to bat-caves Footnote 5. Histoplasmosis is not a nationally notifiable disease in Canada, so the true incidence of infection nationally is unknown and it is possible that many cases go and/or unreported.
Case series
In April 2024, four (three confirmed, one suspected) Canadian travellers, two 37-year-old males, a 36-year-old female and a three-year-old male, developed symptomatic histoplasmosis after swimming in Cenote Aktunzots near Tres Reyes in the Yucatán peninsula of Mexico. They recalled seeing bats inside the cenote. Two other members of their party, a 33-year-old woman and a two-year-old male, stayed at the resort rather than attending the cenote and remained asymptomatic. Patient consent was obtained to share the following information.
Case 1
Approximately 18 days after visiting the cenote, the 37-year-old male developed fevers, myalgia, fatigue and then cough. He was found to have bilateral pulmonary nodules with cavitation and ground-glass opacities on computed tomography scan (Figure 1) and underwent bronchoalveolar lavage on day 14 of illness. Bacterial, fungal and mycobacterial bronchoalveolar lavage cultures were negative. Leptospirosis, dengue, syphilis and HIV serologies were negative. At day 11 of illness H. capsulatum serology was negative, but urine Histoplasma antigen was positive (MiraVista Diagnostics, Indianapolis, Indiana).
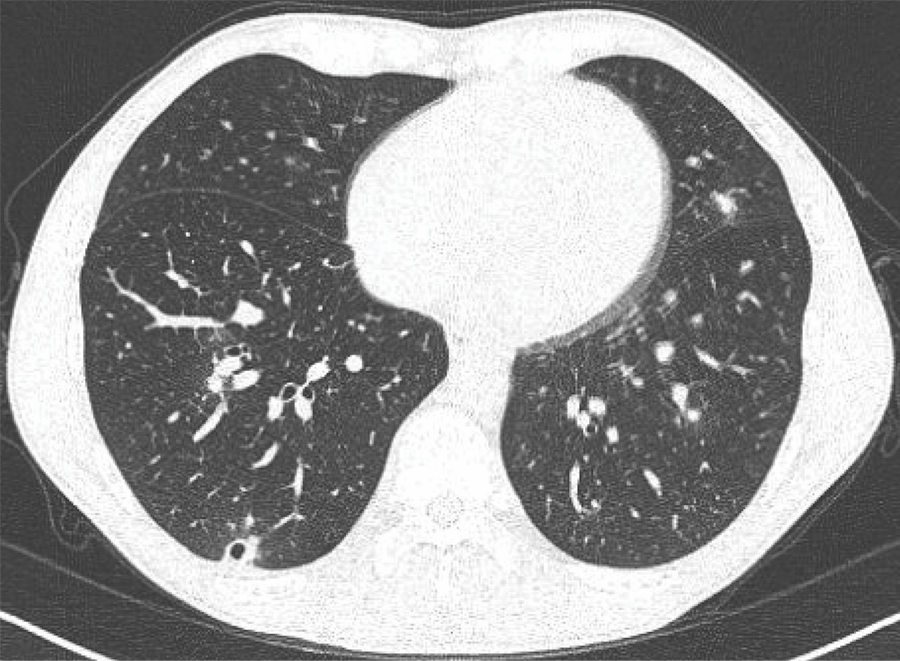
Figure 1: Descriptive text
The computed tomography of chest of Case 1 demonstrated scattered bilateral lung nodules with surrounding ground-glass and micro nodules, as well as two lower lobe nodules with central cavitation in keeping with evolving fungal infection.
Because of ongoing flu-like symptoms significantly impairing his daily function, itraconazole was started on day 14 of the illness. He received a total of six weeks of itraconazole. Following treatment, his fevers abated and symptoms improved. He did not receive antibiotics. A repeat computed tomography scan six weeks after treatment discontinuation showed resolution of the cavitating nodule and reduction of bilateral nodules and ground-glass opacities. Histoplasma capsulatum serology repeated 10 weeks after the initial diagnosis was positive.
Case 2
Two days after Case 1 developed symptoms, his son, a previously healthy three-year-old male developed daily high-grade fevers (39°C), myalgias, abdominal pain and headaches. At time of initial assessment, he had been symptomatic for 10 days. On examination, he was noted to have an oral aphthous ulcer, several small erythematous papules on his trunk, cervical and inguinal lymphadenopathy and hepatomegaly. Alanine aminotransferase was mildly elevated at 58 U/L (normal 10–29 U/L) and lactate dehydrogenase was elevated at 585 U/L (normal 207–383 U/L). Chest X-ray revealed bilateral hilar lymphadenopathy, fine nodularity and trace pleural effusions in the bases. Abdominal ultrasound showed mild hepatomegaly with relatively increased periportal echoes (“starry sky appearance”), a bulky spleen and intra-abdominal adenopathy. Histoplasma capsulatum serology was initially negative and urine was positive for Histoplasma antigen. Human immunodeficiency virus serology was negative.
Itraconazole, dosed at 10 mg/kg/day divided BID, was initiated on day 17 of illness. His fevers resolved within 48 hours of treatment initiation and his energy quickly improved. He received three months total duration of itraconazole. Therapeutic drug monitoring was done two weeks after itraconazole initiation and monthly afterward, targeting levels between 1,420 nmol/L and 4,840 nmol/L. The patient’s itraconazole level was initially in target range, then the dose was decreased to 7.5 mg/kg/day approximately six weeks into therapy, after the repeat level was elevated. He did not experience any adverse medication effects. Repeat H. capsulatum serology drawn approximately eight weeks after the initial diagnosis was positive. Prior to discontinuing treatment at three months, a repeat abdominal ultrasound demonstrated resolution of previous findings and reported as a normal study. Repeat chest X-rays showed interval resolution of the perihilar thickening, decreased fine nodularity bilaterally, with residual perihilar adenopathy. A chest X-ray three months post treatment discontinuation was normal.
Case 3
Several days following symptom onset of Case 1, approximately three weeks following the visit to the cenote, the other 37-year-old male developed a self-limited febrile illness with myalgia and fatigue but without respiratory symptoms. His symptoms lasted approximately 12 days. Urine Histoplasma antigen was positive and initial H. capsulatum serology was negative. Human immunodeficiency virus serology was negative. Due to absence of respiratory symptoms, no chest imaging was done. No antifungal therapy was prescribed and he made a full recovery.
Case 4
The 36-year-old female also developed cough and flu-like illness upon return to Canada, just over two weeks from exposure to the cenote. She did not have chest imaging, but was diagnosed clinically with probable community-acquired pneumonia by her family physician and was prescribed amoxicillin. Her symptoms were relatively mild and gradually resolved over the next 1–2 weeks. She did not receive antifungal therapy. Urine Histoplasma antigen and histoplasma serology performed approximately three weeks after her symptom onset were negative. Repeat convalescent serology was not available.
Discussion
Cenotes (sinkholes) of the Yucatán Peninsula are flooded caves that are a popular tourist attraction, drawing crowds of local and international visitors Footnote 6; however, these cenotes have previously been implicated in exposure to H. capsulatum. The federal Ministry of Health of Mexico declared an outbreak between July and August 2022 after five tourists were diagnosed with histoplasmosis at a local hospital after visiting a cenote located in the municipality of Homún Footnote 7. Another cenote in same region has been closed since 2019 due to association with cases of histoplasmosis among tourists Footnote 8.
The high attack rate observed in this group of exposed travellers, with two developing more severe disease, suggests they likely encountered high concentrations of H. capsulatum spores at the cenote. On the other hand, the relatively long period of time between exposure to symptom onset (approximately three weeks, on the upper end of the typical 1–3 week incubation period), may be suggestive of a lower inoculum.
The symptoms of histoplasmosis can be non-specific and may lead to delayed diagnosis and unnecessary invasive diagnostic procedures Footnote 9. The sensitivity and specificity of testing modalities depends on the patient’s clinical syndrome, host-immune factors, timing and type of specimen collection. In general, Histoplasma antigen testing (e.g., MiraVista Diagnostics, Indianapolis, Indiana) is considered the most sensitive test in acute illness, but may miss milder infections with lower fungal burden in immunocompetent hosts Footnote 10.
Of our group, three individuals tested positive for urine Histoplasma antigen. Both of our cases who presented with more severe illness were initiated on empiric treatment while waiting for these test results. Our fourth case presented with symptoms of a non-specific influenza-like illness, suggestive of acute pulmonary histoplasmosis because of the epidemiologic context. The diagnosis was not confirmed by available laboratory testing; urine antigen testing was negative. The sensitivity of urine antigen testing is estimated to be 80% in acute pulmonary histoplasmosis, 30% in subacute pulmonary and 90% in progressive disseminated histoplasmosis Footnote 10.
All four cases had negative initial H. capsulatum serologies drawn approximately 2–4 weeks after exposure. In Cases 1 and 2, serologies that were repeated after 8–10 weeks turned positive. Unfortunately, repeat serologies in Cases 3 and 4 were not obtained. Histoplasma antibody testing was performed via immunodiffusion by the Alberta Provincial Laboratory for Public Health and included detection of both H and M antibodies Footnote 11. Histoplasma capsulatum antibodies typically take 4–8 weeks to become detectable in peripheral blood. Serology is estimated to have a sensitivity of approximately 65% in acute pulmonary histoplasmosis, 95% in subacute pulmonary, 83% in chronic pulmonary and 75% in progressive disseminated histoplasmosis. Antibody testing is most useful in subacute and chronic forms of histoplasmosis where sensitivity of urine antigen is decreased Footnote 10. Fungal cultures of the one patient who underwent bronchoalveolar lavage were ultimately negative. Culture-based methods can be challenging for informing acute management as growth typically takes 2–3 weeks and may only be positive in the minority of patients with acute pulmonary histoplasmosis (0%–20%) Footnote 10.
Recent guidelines suggest testing for histoplasmosis in all patients with community-acquired pneumonia without improvement on empiric antibiotics and exposure to an endemic area, or on initial presentation of community-acquired pneumonia in patients with high risk exposure to bird or bat droppings, or epidemiologic link to histoplasmosis outbreak Footnote 12. Practitioners should be aware that local acquisition outside the Great Lakes region is also possible in Canada Footnote 11. The urine Histoplasma antigen test is recommended as first line, with H. capsulatum serology more useful for subacute or chronic presentations Footnote 12.
Conclusion
Given the number of Canadian tourists travelling to the Yucatán peninsula and the increasing popularity of visiting cenotes, awareness of the risk associated with this specific exposure should be promoted. Cenote exposure should raise the index of suspicion for histoplasmosis in symptomatic returning travellers.
Authors' statement
- EM — Writing–original draft, writing–review & editing
- MH — Writing–review & editing
- DG — Writing–review & editing
- JH — Conceptualization, writing–review & editing
All authors were involved in the clinical care of the patients and review and approval of the final version of the manuscript. The content and view expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
Competing interests
The authors of this paper do not have any competing interests to declare.
ORCID numbers
- Elspeth MacBain — 0009-0009-4097-2641
- Michael Hawkes — 0000-0002-4122-0937
- David Goldfarb — 0000-0003-0835-9504
- Jan Hajek — 0000-0003-1863-4071
Acknowledgements
None.
Funding
None.
References
- Footnote 1
-
Ashraf N, Kubat RC, Poplin V, Adenis AA, Denning DW, Wright L, McCotter O, Schwartz IS, Jackson BR, Chiller T, Bahr NC. Re-drawing the Maps for Endemic Mycoses. Mycopathologia 2020;185(5):843–65. https://doi.org/10.1007/s11046-020-00431-2
- Footnote 2
-
Bahr NC, Antinori S, Wheat LJ, Sarosi GA. Histoplasmosis infections worldwide: thinking outside of the Ohio River valley. Curr Trop Med Rep 2015;2(2):70–80. https://doi.org/10.1007/s40475-015-0044-0
- Footnote 3
-
Wheat LJ, Freifeld AG, Kleiman MB, Baddley JW, McKinsey DS, Loyd JE, Kauffman CA; Infectious Diseases Society of America. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 2007;45(7):807–25. https://doi.org/10.1086/521259
- Footnote 4
-
Akram SM, Koirala J. Histoplasmosis. StatPearls Publishing 2025. [Accessed 2025 Mar 2]. http://www.ncbi.nlm.nih.gov/books/NBK448185/
- Footnote 5
-
Staffolani S, Buonfrate D, Angheben A, Gobbi F, Giorli G, Guerriero M, Bisoffi Z, Barchiesi F. Acute histoplasmosis in immunocompetent travelers: a systematic review of literature. BMC Infect Dis 2018;18(1):673. https://doi.org/10.1186/s12879-018-3476-z
- Footnote 6
-
Enseñat-Soberanis F, Blanco-Gregory R, Mondragón-Mejía J, Simoes N, Moreno-Acevedo E, Ortega I. Crowding standards and willingness to pay at cenotes (sinkholes) of the Yucatan Peninsula: a comparative analysis of local, national and international visitors. J Ecotour 2020;19(1):1–22. https://doi.org/10.1080/14724049.2019.1619747
- Footnote 7
-
The Yucatan Times. An outbreak of Histoplasmosis is detected in a Yucatán cenote. 2023. [Accessed 2024 May 16]. https://www.theyucatantimes.com/2023/05/an-outbreak-of-histoplasmosis-is-detected-in-a-yucatan-cenote/
- Footnote 8
-
Ruíz G. This is the forbidden cenote located in Peto, Yucatán: PHOTO REPORT. Por Esto! 2022. [Accessed 2024 May 19]. https://www.poresto.net/yucatan/2022/1/29/este-es-el-cenote-prohibido-ubicado-en-peto-yucatan-fotorreportaje.html
- Footnote 9
-
Staffolani S, Riccardi N, Farina C, Lo Cascio G, Gulletta M, Gobbi F, Rodari P, Ursini T, Bertoli G, Ronzoni N, Bisoffi Z, Angheben A. Acute histoplasmosis in travelers: a retrospective study in an Italian referral center for tropical diseases. Pathog Glob Health 2020;114(1):40–5. https://doi.org/10.1080/20477724.2020.1716517
- Footnote 10
-
Azar MM, Hage CA. Laboratory Diagnostics for Histoplasmosis. J Clin Microbiol 2017;55(6):1612–20. https://doi.org/10.1128/JCM.02430-16
- Footnote 11
-
Dingle TC, Croxen MA, Fathima S, Shokoples S, Sonpar A, Saxinger L, Schwartz IS. Histoplasmosis acquired in Alberta, Canada: an epidemiological and genomic study. Lancet Microbe 2021;2(5):e191–7. https://doi.org/10.1016/S2666-5247(20)30229-9
- Footnote 12
-
Smith DJ, Free RJ, Thompson GR 3rd, Baddley JW, Pappas PG, Benedict K, Gold JA, Tushla LA, Chiller T, Jackson BR, Toda M; Endemic Mycoses Diagnostic Algorithm Subject Matter Expert Group. Clinical Testing Guidance for Coccidioidomycosis, Histoplasmosis, and Blastomycosis in Patients With Community-Acquired Pneumonia for Primary and Urgent Care Providers. Clin Infect Dis 2024;78(6):1559–63. https://doi.org/10.1093/cid/ciad619
