The impact of the COVID-19 pandemic on select travel-acquired enteric illnesses

 Download this article as a PDF (242 KB)
Download this article as a PDF (242 KB)Published by: The Public Health Agency of Canada
Issue: Volume 51-5, May 2025: Travel Health
Date published: May 2025
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 51-5, May 2025: Travel Health
Epidemiologic Study
Assessing the impact of the COVID-19 pandemic on trends of select travel-acquired enteric illnesses in Canada
Lauren Rusk1, Russell Forrest1, Meghan Hamel1
Affiliation
1 Centre for Food-Borne, Environmental and Zoonotic Infectious Diseases, Public Health Agency of Canada, Guelph, ON
Correspondence
Suggested citation
Rusk LN, Forrest RO, Hamel M. Assessing the impact of the COVID-19 pandemic on trends of select travel-acquired enteric illnesses in Canada. Can Commun Dis Rep 2025;51(5):160–6. https://doi.org/10.14745/ccdr.v51i05a02
Keywords: COVID-19, enteric illness, travel-acquired illness, travel, trends
Abstract
Background: Millions of Canadians contract enteric illnesses each year, many of which are acquired during, or are otherwise associated with, international travel. As the number of Canadians travelling fluctuates throughout the year, a corresponding change in the number of travel-acquired enteric illnesses was expected. A change in the number of travel-acquired enteric illnesses was also expected during the COVID-19 pandemic restrictions.
Objective: This study aims to explore trends in the number and distribution of select travel-acquired enteric infections in Canada, from May 2017 to April 2023.
Methods: To evaluate trends, Student’s t-tests and negative binomial regression modelling were conducted. Percent changes and relative risks were calculated to assess the impact of the pandemic on travel-acquired enteric illnesses.
Results: Findings demonstrated a seasonal peak in the number of reported travel-acquired enteric illnesses during the winter and spring pre- and post-pandemic travel restrictions (May 2017–February 2020 and September 2021–April 2023). Additionally, there was a decrease in the number of travel-acquired enteric illnesses added to enteric illness travel clusters with cases in more than one province or territory (multi-jurisdictional) during and after the lifting of COVID-19 travel restrictions. However, cases reported post-travel restrictions had a higher risk of being added to a multi-jurisdictional enteric illness travel cluster compared to the pre-travel restriction phase.
Conclusion: Nonessential travel restrictions and changes in the healthcare-seeking behaviours due to the pandemic likely account in part for the change in the number of travel-acquired enteric illnesses observed while travel restrictions were implemented and after they were lifted. Further research is required to explain the increased risk of illnesses being added to multi-jurisdictional enteric illness travel clusters after the lifting of travel restrictions compared to pre-COVID-19.
Introduction
Each year, millions of Canadians experience enteric illnesses, of which approximately 25% are acquired during international travel Footnote 1. Research suggests that the incidence of travel-acquired enteric illness correlates with the number of travellers, peaking during periods of high travel activity Footnote 2Footnote 3. In Canada, this tends to occur during the winter months and previous studies in Ontario and British Columbia have confirmed this increase at the provincial level Footnote 4Footnote 5Footnote 6.
In March 2020, the World Health Organization declared the SARS-CoV-2 virus outbreak a pandemic. This led to countries implementing various public health measures to try and curb its spread Footnote 7. These measures also impacted the transmission of other infectious diseases. For example, multiple countries reported a decrease in the observed incidence of enteric infections Footnote 8Footnote 9Footnote 10Footnote 11. One explanation for this decrease may be a corresponding decline in the number of travel-acquired cases of enteric illness due to the implementation of nonessential travel restrictions Footnote 8Footnote 9Footnote 11Footnote 12. In Canada, nonessential travel restrictions were in effect from March 2020–August 2021 Footnote 13Footnote 14. During this period, a reduction in the number of reported travel-acquired enteric illness cases was observed Footnote 8. However, trends and a more detailed analysis of the changes in the risk of travel-acquired enteric infections before, during and after this period remain insufficiently studied.
After nonessential travel restrictions were lifted, the phrase “revenge travel” emerged to describe the expected surge in travel activity as people rescheduled cancelled plans Footnote 15. It was hypothesized that this might lead to an increase in travel-acquired enteric infections. Currently, little is known about the extent of the “revenge travel” phenomenon and its potential effects on the number of travel-acquired enteric illness cases in Canada.
This study aims to analyze trends in travel-acquired enteric infections in Canada at the national level and assess how travel-acquired enteric infections were influenced by the imposition and removal of nonessential travel restrictions during the COVID-19 pandemic.
Methods
Data sources
Since 2017/2018, whole-genome sequencing (WGS) has been routinely performed in Canada on various enteric pathogens, including Salmonella, Listeria, Escherichia coli and Shigella, at the National Microbiology Laboratory or by a PulseNet Canada-certified provincial laboratory. Whole-genome sequencing data is shared with PulseNet Canada and compared nationally using whole-genome multi-locus sequencing typing (wgMLST) within a central BioNumerics v7.6.3 database (Applied Maths, United States). PulseNet Canada assigns cluster codes to Salmonella, Listeria, E. coli and Shigella clusters when two or more isolates (where at least one is clinical) group together within 10 wgMLST allele differences within a specified period. The criteria for common Salmonella serotypes (including S. Enteritidis, S. Heidleberg and S. Typhimurium) is three or more isolates grouping together within 10 wgMLST allele differences with at least two isolates within five alleles within a specified period. Clusters can be either single jurisdictional, with cases occurring in only one province/territory, or multi-jurisdictional, if cases occur in multiple provinces/territories. Any case that does not group within 10 wgMLST allele differences of another case is considered sporadic. As single-jurisdictional clusters and sporadic cases are not routinely investigated at the national level, these were excluded from our analyses.
Epidemiologists at the Public Health Agency of Canada (PHAC) review all multi-jurisdictional clusters and classify them to aid with follow-up. Only clusters classified as travel-related were included in our analyses. A cluster was deemed travel-related if 1) there was strong epidemiological evidence to suggest the illnesses were acquired while outside of Canada (i.e., people acquired an enteric illness while outside Canada but were tested in Canada upon their return), 2) the cluster was genetically related (i.e., within 10 wgMLST allele differences) to another previously classified travel cluster or 3) the serotype is not endemic to Canada (i.e., S. typhi and S. enterica serovar Paratyphi A) Footnote 16. At the time of our study, no multi-jurisdictional travel-related clusters of Listeria had been identified in Canada at the federal level. Therefore, only Salmonella, E. coli and Shigella were considered.
Using these criteria, we analyzed cases added to multi-jurisdictional Salmonella travel clusters in Canada from May 2017 to April 2023 and E. coli and Shigella travel clusters from June 2018 to April 2023 as a representation for all travelled-acquired cases of enteric illness. The date used for cases was the earliest of the following dates: 1) the isolation date, 2) the date the isolate was received for WGS or 3) the date the case was reported to PHAC.
Data for the number of Canadians travelling internationally was retrieved from a publicly available Statistics Canada dataset Footnote 17. These data were collected by the Frontier Counts program, which counts the number of individuals entering Canada. For this study, the number of Canadian residents returning from countries other than the United States was used. Travel to the United States was excluded due to the similarities in the Canadian and American food supply and because, to date, there has not been a multi-jurisdictional enteric illness cluster solely associated with travel to the United States identified in Canada.
Statistical analyses
Three time periods were analyzed: pre-COVID-19 pandemic travel restrictions (before travel restrictions related to the COVID-19 pandemic were issued; May 2017–February 2020), COVID-19 pandemic travel restrictions (March 2020–August 2021) and post-COVID-19 pandemic travel restrictions (after the travel restrictions were revoked; September 2021–April 2023). Cases were assigned to these phases based on the earliest available date described above.
Trends in the number of cases of enteric illness added to multi-jurisdictional enteric illness travel clusters were assessed using two-sided Student’s t-tests to compare the mean monthly number of cases between phases. A negative binomial regression model was also employed. Negative binomial regression is suitable for modelling discrete count data that is left-censored at zero, which is common in epidemiological studies Footnote 18. Variables included in model building were time (in one-month increments), meteorological season (winter=December–February, spring=March–May, summer=June–August, fall=September–November), the monthly number of Canadians travelling internationally and the presence of travel restrictions. Two-way interactions between independent variables were also assessed. Model selection was preformed using stepwise selection along with the Akaike Information Criterion (AIC) and likelihood-ratio test.
Percent changes in the number of travellers and cases between phases were evaluated. Relative risks (RR) were calculated to assess changes in the risk of cases being added to multi-jurisdictional enteric illness travel clusters, comparing the COVID-19 travel restrictions and post-travel restrictions phases to a pre-COVID-19 reference period of equal length.
All statistical analyses were conducted in Stata/MP 15 (Stata Corporation, United States) and utilized an alpha value of 0.05.
Results
Trends in travel-acquired enteric infections
From May 2017 to February 2020, the number of travel-acquired Salmonella infections added to multi-jurisdictional enteric illness travel clusters in Canada was significantly higher in February and March (p=0.0436 and p=0.0312, respectively; Figure 1) compared to other months. Travel-acquired cases of Shigella and E. coli did not exhibit any significant seasonal trends between June 2018 and February 2020. No seasonal trends were observed from March 2020 to August 2021 for all three pathogens while nonessential travel restrictions were in effect. From September 2021 to April 2023, the total number of monthly travel-acquired enteric infections added to multi-jurisdictional enteric illness travel clusters in Canada was significantly higher in March and April (p=0.0053 and p=0.0017, respectively). These increases correspond with increased international travel by Canadians during the winter and spring (Figure 1).
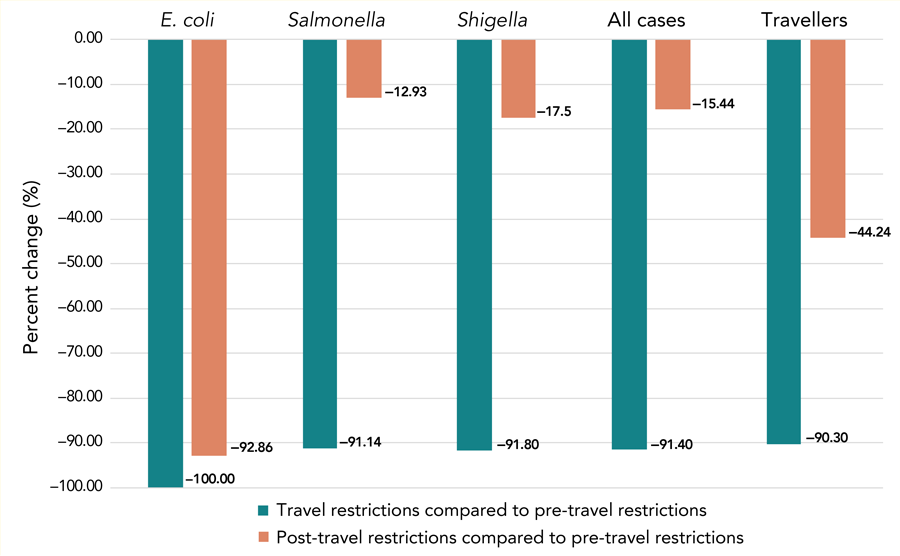
Figure 1: Descriptive text
Figure 1A shows the number of cases of enteric illness added to multi-jurisdictional travel-related clusters between May 2017 and April 2023. From May 2017 to February 2020, the average number of cases of enteric illness added to multi-jurisdictional travel-related clusters was 87.9 cases per month. There is a clear seasonal trend with a monthly average of 159.4 cases being reported from February to April compared to a monthly average of 69.1 cases reported from May to January. The number of cases added to multi-jurisdictional travel-related clusters decreased sharply after March 2020 coinciding with the implementation of non-essential travel restrictions during the COVID-19 pandemic. While travel restrictions were in effect from April 2020 to August 2021, the average monthly number of travel-acquired cases of enteric illness added to multi-jurisdictional travel-related clusters was 9.1 cases per month, with no clear seasonal trend. Following the lifting of non-essential travel restrictions in August 2021, the number of cases of enteric illness added to multi-jurisdictional travel-related clusters slowly increased. The average monthly number of cases of enteric illness added to multi-jurisdictional travel-related clusters from September 2021 until the end of the study period (April 2023) was 85.1 cases per month. Case activity returned to approximately the same level and seasonal pattern seen prior to the travel restriction in March 2022.
Figure 1B shows the number of Canadians returning from international travel between May 2017 and April 2023. Between May 2017 and February 2020, there is a seasonal trend with travel activity peaking during the winter months. From February to April, on average 1.2 million Canadian returned from international travel each month, while there was an average of 937,000 Canadians travelling each month throughout the remainder of the year. After the implementation of the non-essential travel restrictions in March 2020, there was a drastic decrease in the number of Canadians travelling international. The average monthly number of Canadians returning from international was 88,000 Canadians per month between April 2020 to August 2021 with no seasonal increases. Following the lifting of non-essential travel restrictions in August 2021, international travel by Canadians slowly increased from September 2021 to April 2023 and a seasonal pattern returned. However, the average number of monthly travellers remained below the numbers seen prior to the COVID-19 pandemic. During this time an average of 603,000 Canadians were returning from interactional travel each month with a seasonal peak in travellers observed during the months of March and April.
Abbreviations: E. coli, Escherichia coli; US, United States
- Figure 1 Footnote a
-
Data were collected by the Frontier Counts program, which counts the number of individuals entering Canada. Data from countries other than the United States were used
The negative binomial regression model that best fit the data (AIC=619.62) included all independent variables and the interaction term between time and nonessential travel restrictions (Table 1). The RR for a reported case of enteric illness being added to a multi-jurisdictional enteric illness travel cluster was higher during the winter (RR 1.32; 95% CI: 1.03–1.7) and spring (RR 2.26; 95% CI: 1.77–2.9) compared to the summer, with no significant difference in RR between the summer and fall.
| Variable | β | Standard error | 95% CI | Z value | p-value | |
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Intercept | −192 | 57.87 | −300.88 | −86.64 | −3.32 | <0.001 |
| Meteorological season | ||||||
| Summer | Referent | - | - | - | - | - |
| Fall | −0.041 | 0.13 | −0.29 | 0.2 | −0.33 | 0.74 |
| Spring | 0.82 | 0.13 | 0.57 | 1.06 | 6.52 | <0.001 |
| Winter | 0.28 | 0.13 | 0.031 | 0.53 | 2.25 | 0.025 |
| Number of travellers (centred at 668,199.4) | 1.36e-6 | 2.10e-7 | 9.31e-7 | 1.8e-6 | 6.49 | <0.001 |
| Time (measured in one-month intervals) | 0.097 | 0.029 | 0.043 | 0.15 | 3.38 | <0.001 |
| Restrictions on nonessential travel | ||||||
| No | Referent | - | - | - | - | - |
| Yes | 3,273 | 529.7 | 2,261.5 | 4,327.81 | 6.18 | <0.001 |
| Interaction term between time and travel restrictions | −1.62 | 0.26 | −2.14 | −1.12 | −6.18 | <0.001 |
Abbreviations: CI, confidence interval; LL, lower limit; UL, upper limit; -, not applicable |
||||||
Impact of COVID-19 pandemic travel restrictions
Between June 2020 and August 2021, the number of Canadians returning from countries other than the United States decreased by 90.3% compared to the same period in 2018–2019 (1,447,595 travellers vs. 14,924,122 travellers). This decline in travellers corresponded with a 91.4% decrease in the number of reported cases of enteric illness added to multi-jurisdictional travel clusters (100 cases vs. 1,163 cases), which was observed across all three pathogens (Figure 2). Despite the overall decrease, the RR of reported cases of enteric illness being added to multi-jurisdictional travel clusters during the COVID-19 travel restriction phase did not change compared to the pre-COVID-19 travel restrictions phase (Table 2).
Figure 2: Descriptive text
This figure shows the percent change in the number of enteric illnesses added to multi-jurisdictional travel-related clusters and the number of Canadians returning from international travel during and after non-essential travel restrictions compared to a pre-travel restriction reference period. While travel restrictions were in effect, the number of Escherichia coli cases added to multi-jurisdictional travel-related clusters decreased by 100.00%, Salmonella cases by 91.14% and Shigella cases by 91.80%. Overall, the number of enteric illnesses added to multi-jurisdictional travel-related clusters decreased by 91.40% compared to the pre-travel restriction reference period. Similarly, the number of Canadians returning from international travel was 90.30% lower while non-essential travel restrictions were in place compared to the pre-travel restriction reference period. After the lifting of travel restrictions, the total number of enteric illnesses added to multi-jurisdictional travel-related clusters was 15.44% lower compared to the pre-travel restriction reference period, with E. coli cases decreased by 92.86%, Salmonella cases by 12.93% and Shigella cases by 17.50%. A similar trend is seen in the number of Canadians returning from international travel, with a 44.24% decrease in the monthly number of Canadians returning from international travel when comparing the post non-essential travel restrictions period to the pre non-essential travel restrictions period.
Abbreviation: E. coli, Escherichia coli
| Comparison | Pathogen | |||||||
|---|---|---|---|---|---|---|---|---|
| Salmonella | Shigella | Escherichia coli | Overall | |||||
| RR (95% CI) |
p-value | RR (95% CI) |
p-value | RR (95% CI) |
p-value | RR (95% CI) |
p-value | |
| COVID-19 travel restrictions to pre-COVID-19 travel restrictions | 0.91 (0.74–1.13) |
0.44 | 0.85 (0.34–2.10) |
1 | 0 (0.0–0.0) |
0.11 | 0.89 (0.72–1.09) |
0.26 |
| Post-COVID-19 travel restrictions to pre-COVID-19 travel restrictions | 1.57 (1.45–1.70) |
<0.001 | 1.46 (1.11–1.92) |
0.007 | 0.34 (0.16–0.73) |
0.003 | 1.53 (1.42–1.64) |
<0.001 |
Abbreviations: CI, confidence interval; RR, relative risk Footnote
|
||||||||
Post-COVID-19 pandemic nonessential travel restrictions
Following the lifting of international travel restrictions in August 2021, both international travel by Canadians and the reported number of enteric infections added to multi-jurisdictional travel clusters increased, but overall neither had returned to pre-pandemic levels (Figure 1). From September 2021 to February 2023, international travel was 44.2% lower compared to the 2018–2020 reference period (10,206,099 travellers vs. 18,304,311 travellers). Similarly, the number of reported enteric infections added to multi-jurisdictional travel clusters decreased by 15.4% (1,309 cases vs. 1,548 cases). Despite this, the RR of enteric illnesses added to multi-jurisdictional travel clusters was higher during the post-COVID-19 travel restriction phase compared to the pre-COVID-19 travel restriction phase, primarily due to an increased risk of travel acquired salmonellosis (Table 2).
Discussion
Anecdotal evidence suggested that travel-acquired enteric illnesses in Canada peak during the winter months; however, this had not yet been confirmed nationally. This study finds that indeed international travel by Canadians is highest from January to April, corresponding with a peak in the reported number of travel-acquired enteric illnesses added to multi-jurisdictional travel clusters. This seasonal pattern aligns with trends observed in other countries, where travel-acquired enteric infections peak with increased travel activity Footnote 2Footnote 3. In Canada, this peak is primarily driven by an increase in the reported number of Salmonella infections, consistent with provincial-level trends observed in Ontario Footnote 4Footnote 5.
The COVID-19 pandemic prompted the Canadian government to introduce public health measures aimed at reducing the spread of the SARS-CoV-2 virus. These measures helped to reduce the incidence of not only COVID-19 but many other infectious diseases, including enteric diseases Footnote 8Footnote 9Footnote 10Footnote 11. Several hypotheses have been proposed for the reduction in enteric illness incidence rates during the pandemic including changes in exposure-causing behaviours, changes in healthcare-seeking behaviours and a decrease in international travel. In March 2020, Canada imposed restrictions on nonessential international travel, which remained in effect until August 2021 Footnote 13Footnote 14. These restrictions reduced international travel by Canadians by 90.3% compared to the pre-pandemic reference period. As approximately 25% of enteric infections in Canada are travel-related Footnote 1, a reduction in enteric infections was anticipated and confirmed, with a 91.41% decrease in reported travel-acquired enteric infections. However, the absence of a significant change in RR suggests that this decrease was likely due to less international travel rather than changes in the risk of contracting an enteric illness abroad.
As the COVID-19 travel restrictions ended, many expected a spike in travel activity as individuals capitalized on the re-established ability to travel. We hypothesized that there would be an increase in international travel by Canadians and a corresponding increase in the number of travel-acquired enteric infections. Contrary to this, travel by Canadians was slow to rebound completely, with a 44.24% reduction in the number of Canadian travellers compared to pre-COVID-19 levels. Moreover, the number of reported travel-acquired enteric infections added to multi-jurisdictional travel clusters decreased by 14.76%. Despite this decline, the RR of 1.53 (95% CI: 1.42–1.64) suggests a higher risk of travel-acquired cases of enteric illness being added to multi-jurisdictional clusters during this period. It is possible that, due to the COVID-19 pandemic, Canadians are now more health-conscious and aware of the health risks associated with international travel. Furthermore, given that many symptoms of enteric infections mirror those of COVID-19, more ill Canadians may have sought a medical diagnosis upon returning to Canada during this period out of fear that they had contracted COVID-19. This would result in cases of enteric illness being reported that historically may have gone undetected. Another possible explanation is that there were changes in the travel destinations of Canadians after the pandemic. As different countries have differing rates of enteric disease, this also could have contributed to the increased risk observed.
Limitations
There are some limitations to this study that must be taken into consideration. First, the reported number of travel-acquired enteric infections used underestimates the true burden of travel-associated enteric illness in Canada. Our sampling frame consisted of cases of enteric illness for which a specimen was submitted for testing and WGS, and subsequently assigned to a multi-jurisdictional cluster. Cases of enteric illness often go unreported as many individuals never submit a specimen for testing and are therefore not captured by public health surveillance systems. Additionally, during the pandemic, laboratory testing for COVID-19 was prioritized, which may have reduced testing for enteric pathogens and resulted in further underreporting during this period. Furthermore, cases that were not part of a multi-jurisdictional enteric illness cluster were excluded as they are not routinely investigated at the federal level in Canada.
Additionally, when providing potential explanations for the increased risk since the lifting of travel restrictions, we could not assess whether the travel destinations of Canadians had changed. Therefore, it is not possible to conclude whether changes in travel behaviours amongst Canadians may have contributed to the increased RR.
Finally, misclassification is a concern. At the national level, epidemiologists review exposure details for cases, including whether cases travelled outside of Canada during their exposure period. If a number of cases in a multi-jurisdictional enteric illness cluster report international travel to the same destination, the cluster is classified as travel-associated. Subsequent cases added to the cluster are assumed to be travel-acquired based on their genetic relatedness, but this is generally not confirmed via exposure data. Similarly, clusters identified within 10 wgMLST allele differences to a cluster that was previously classified as a travel cluster are classified as travel-acquired without confirmation via exposure data. Therefore, it is possible that some cases included in this study may not be travel-acquired even though they are in a cluster that is classified as travel-associated. Additionally, due to the limited nature of the exposure information available at a national level, the immigration status of cases is often unknown, which may result in some cases of enteric illness being misclassified. Finally, cases were aggregated by month and categorized into phases based on the earliest date available for each case. All the dates used occurred after the cases’ symptom onset date, which may have caused the case to be misclassified into the wrong month. Future studies should apply quantitative methods to evaluate the impact of potential misclassification and other systemic errors.
Conclusion
Identifying peak periods for travel-acquired enteric illnesses in Canada allows for timely deployment of public health resources and targeted messaging to increase awareness and reduce travel-related risks. The findings of this study highlighted seasonal increases in the number of travel-acquired enteric infections added to multi-jurisdictional enteric illness travel clusters during the winter and spring months. The reduction in cases during the pandemic is likely due to fewer people travelling during this time. While this helps clarify the impact of COVID-19 on these infections, further research is needed to understand the heightened risk during the post-pandemic travel restriction phase.
Authors' statement
- LR — Methodology, formal analysis, writing–original draft, writing–review & editing
- RF — Conceptualization, methodology, formal analysis, writing–review & editing
- MH — Conceptualization, methodology, writing–review & editing
Competing interests
None.
ORCID numbers
- Lauren Rusk — 0009-0004-8042-8118
- Russell Forrest — 0000-0003-1875-388X
- Meghan Hamel — 0009-0006-4058-0726
Acknowledgements
The authors would like to thank all the local, provincial and territorial public health partners who contribute to the ongoing follow-up and collection of exposure information for cases of enteric illness in Canada.
Funding
This work was supported by the Public Health Agency of Canada.
References
- Footnote 1
-
Public Health Agency of Canada. FoodNet Canada 2019 integrated findings report. Ottawa, ON: PHAC; 2024. [Accessed 2024 Dec 25]. https://www.canada.ca/en/public-health/services/publications/food-nutrition/foodnet-canada-2019-integrated-findings-report.html#a12
- Footnote 2
-
Choe YJ, Choe SA, Cho SI. Importation of travel-related infectious diseases is increasing in South Korea: an analysis of salmonellosis, shigellosis, malaria, and dengue surveillance data. Travel Med Infect Dis 2017;19:22–7. https://doi.org/10.1016/j.tmaid.2017.09.003
- Footnote 3
-
Koch K, Kristensen B, Holt HM, Ethelberg S, Mølbak K, Schønheyder HC. International travel and the risk of hospitalization with non-typhoidal Salmonella bacteremia. A Danish population-based cohort study, 1999–2008. BMC Infect Dis 2011;11:277. https://doi.org/10.1186/1471-2334-11-277
- Footnote 4
-
Vrbova L, Johnson K, Whitfield Y, Middleton D. A descriptive study of reportable gastrointestinal illnesses in Ontario, Canada, from 2007 to 2009. BMC Public Health 2012;12:970. https://doi.org/10.1186/1471-2458-12-970
- Footnote 5
-
Tighe MK, Savage R, Vrbova L, Toolan M, Whitfield Y, Varga C, Lee B, Allen V, Maki A, Walton R, Johnson C, Dhar B, Ahmed R, Crowcroft NS, Middleton D. The epidemiology of travel-related Salmonella Enteritidis in Ontario, Canada, 2010–2011. BMC Public Health 2012;12:310. https://doi.org/10.1186/1471-2458-12-310
- Footnote 6
-
Taylor M, MacDougall L, Li M, Galanis E; BC Enteric Policy Working Group. The impact of international travel on the epidemiology of enteric infections, British Columbia, 2008. Can J Public Health 2010;101(4):332–6. https://doi.org/10.1007/BF03405297
- Footnote 7
-
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed 2020;91(1):157–60. https://doi.org/10.23750/abm.v91i1.9397
- Footnote 8
-
Dougherty B, Forrest RO, Smith CR, Morton V, Sherk LM, Avery B, Kearney A, Christianson S, Nadon C, Thomas MK. Impact of the COVID-19 pandemic on the reported incidence of select bacterial enteric diseases in Canada, 2020. Foodborne Pathog Dis 2023;20(3):81–9. https://doi.org/10.1089/fpd.2022.0064
- Footnote 9
-
Ray LC, Collins JP, Griffin PM, Shah HJ, Boyle MM, Cieslak PR, Dunn J, Lathrop S, McGuire S, Rissman T, Scallan Walter EJ, Smith K, Tobin-D’Angelo M, Wymore K, Kufel JZ, Wolpert BJ, Tauxe R, Payne DC. Decreased incidence of infections caused by pathogens transmitted commonly through food during the COVID-19 pandemic – Foodborne diseases active surveillance network, 10 U.S. sites, 2017–2020. MMWR Morb Mortal Wkly Rep 2021;70(38):1332–6. https://doi.org/10.15585/mmwr.mm7038a4
- Footnote 10
-
Love NK, Elliot AJ, Chalmers RM, Douglas A, Gharbia S, McCormick J, Hughes H, Morbey R, Oliver I, Vivancos R, Smith G. Impact of the COVID-19 pandemic on gastrointestinal infection trends in England, February-July 2020. BMJ Open 2022;12(3):e050469. https://doi.org/10.1136/bmjopen-2021-050469
- Footnote 11
-
Mughini-Gras L, Chanamé Pinedo L, Pijnacker R, van den Beld M, Wit B, Veldman K, Bosh T, Franz E. Impact of the COVID-19 pandemic on human salmonellosis in the Netherlands. Epidemiol Infect 2021;149:e254. https://doi.org/10.1017/S0950268821002557
- Footnote 12
-
Steffen R, Lautenschlager S, Fehr J. Travel restrictions and lockdown during the COVID-19 pandemic-impact on notified infectious diseases in Switzerland. J Travel Med 2020;27(8):taaa180. https://doi.org/10.1093/jtm/taaa180
- Footnote 13
-
Government of Canada. Government extends international travel restrictions. Ottawa, ON: Government of Canada; 2020. [Accessed 2023 Sept 8]. https://www.canada.ca/en/public-safety-canada/news/2020/10/government-extends-international-travel-restrictions.html
- Footnote 14
-
Government of Canada. Government of Canada announces easing of border measures for fully vaccinated travellers. Ottawa, ON: Government of Canada; 2021. [Accessed 2023 Sept 8]. https://www.canada.ca/en/public-health/news/2021/07/government-of-canada-announces-easing-of-border-measures-for-fully-vaccinated-travellers.html
- Footnote 15
-
Vogler R. Revenge and catch-up travel or degrowth? Debating tourism Post COVID-19. Ann Tour Res 2022;93:103272. https://doi.org/10.1016/j.annals.2021.103272
- Footnote 16
-
Public Health Agency of Canada. Surveillance of typhoid fever. Ottawa, ON: PHAC; 2019. [Accessed 2024 Oct 17]. https://www.canada.ca/en/public-health/services/diseases/typhoid-fever/surveillance.html
- Footnote 17
-
Statistics Canada. Table 24-10-0053-01 International travellers entering or returning to Canada, by type of transportation and traveller type. Ottawa, ON: StatCan; 2024. [Accessed 2023 Sept 8]. https://doi.org/10.25318/2410005301-eng
- Footnote 18
-
Byers AL, Allore H, Gill TM, Peduzzi PN. Application of negative binomial modeling for discrete outcomes: a case study in aging research. J Clin Epidemiol 2003;56(6):559–64. https://doi.org/10.1016/S0895-4356(03)00028-3
