Chronic Diseases and Injuries in Canada
Chronic Diseases and Injuries in Canada
Volume 31 · Supplement 1 · Fall 2011
Patterns of Health Services Utilization in Rural Canada
R.W. Pong, PhD (1); M. DesMeules, MSc (2); D. Heng, MSc (1); C. Lagacé, MSc (2); J.R. Guernsey, PhD (3); A. Kazanjian, PhD (4); D. Manuel, MD, MSc (5); J.R. Pitblado, PhD (1); R. Bollman, PhD (6); I. Koren, MSc (1); M.P. Dressler, MSc (2); F. Wang, MSc (2); W. Luo, MSc (2)
Author References
- Centre for Rural and Northern Health Research, Laurentian University
- Public Health Agency of Canada
- Dalhousie University
- University of British Columbia
- Institute for Clinical Evaluative Sciences
- Statistics Canada
Correspondence: Raymond Pong, Centre for Rural and Northern Health Research, Laurentian University, 935 Ramsey Lake Road, Sudbury, Ontario, Canada P3E 2C6; Tel.: (705) 675-1151 ext. 4357; Fax: (705) 675-4855; Email: rpong@laurentian.ca
Introduction
Context of this study
Canadians value ease of access to their health services. Although many studies have focused on accessibility to health services in Canada, few have examined rural-urban differences in this aspect, particularly from a national perspective. Yet disparities in access to health services exist between rural and urban populations, as do the challenges of delivering health care to more remote areas or to those with small populations.
"Canada's Rural Communities: Understanding Rural Health and Its Determinants" is a three-year research project co-funded by the Canadian Population Health Initiative (CPHI) of the Canadian Institute for Health Information (CIHI) and the Public Health Agency of Canada (PHAC). It involves investigators from the Public Health Agency of Canada, the Centre for Rural and Northern Health Research (CRaNHR) at Laurentian University, and other researchers. The first publication of the research project was How Healthy Are Rural Canadians? An Assessment of Their Health Status and Health Determinants;Footnote 1a1a this, the second publication, is a descriptive analysis of the utilization patterns of a broad range of health services by rural residents compared to their urban counterparts.
Framework for analyzing health services utilization
Where we live influences our health through environmental and climatic conditions, socio-economic factors, occupational activities, ethnic composition, culture and community features. The characteristics of places and of the individuals within them are interrelated in complex ways, and these, as well as the health care system itself, must be considered in any analysis of health outcomes. A theoretical model developed by AndersenFootnote 2a2a was used to guide the research and analysis behind this report. This "Emerging Behavioural Model" includes predisposing factors, enabling factors and needs that are important in influencing the utilization of health services (Figure 1).Footnote 2b2b Predisposing factors include age, sex and social status; enabling factors include external conditions that facilitate or inhibit the use of health services (such as distance to physicians' offices); needs, which might be viewed from either the individual's or the health care provider's perspective, are the individual's medical conditions or disabilities.
The task for researchers is to determine which of these factors are important in a particular situation and how they interact to facilitate or hinder the use of health services.
Figure 1
An adaptation of the Emerging Behavioural Model of people's use of health services
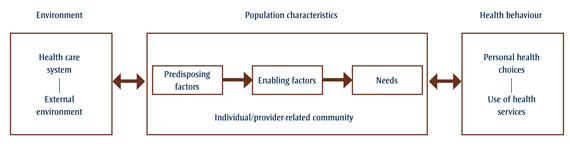
Figure 1 - Text equivalent
An adaptation of the Emerging Behavioural Model of people’s use of health services
A theoretical model developed by Andersen2a was used to guide the research and analysis behind this report. This “Emerging Behavioural Model” includes predisposing factors, enabling factors and needs that are important in influencing the utilization of health services.
Adapted with permission from Andersen.Footnote 2c2c
The framework's elements
Environment
Universal health care is meant to ensure that all Canadians have access to essential medical and hospital care. However, geographically isolated communities or those with small populations tend to have fewer providers and services. For instance, even though 21.1% of the Canadian population lived in rural areas in 2004 only 9.4% of all physicians (16% of family physicians and 2.4% of specialists) practiced in those areas.Footnote 3a3a A study that examined factors affecting referrals to physician specialists in Ontario found that the type of community in which a physician practices—rural area, small town, a community with only primary care physicians or an urban centre with or without teaching hospitals—is the most accurate predictor of referral rates to specialists and that rural areas have the lowest rates of these four types of community.Footnote 44
The external environment refers to such factors as economic conditions, relative wealth, politics and the prevailing norms of the society. For instance, rural communities face a number of economic and employment challenges: technological changes and resource depletion can change employment opportunities in some rural communities, and centralization of services can undermine the economic and social viability of others. Evidence suggests that unemployment and economic insecurity are associated with physical illness, mental stress and higher mortality, which, in turn, may lead to greater need for and use of health services.Footnote5 In addition to economic changes, many health services depend increasingly on sophisticated and expensive technologies that can only be justified in larger hospitals serving larger communities. This may result in a lack of local health care resources and services.
Predisposing factors
Rural communities have some socio- demographic conditions that affect health care utilization differently from urban communities. For example, many rural communities have a higher dependency ratio because they have larger proportions of children and seniors,Footnote 66 and the very young and the very old tend to use health services to a greater extent than the working- age population.Footnote * Community characteristics can also be an important influence. One study has found a significant relation between women's perceptions of the social quality of their community and their perceived health status and functioning, while men's perceptions of their physical environment were related to their reported functioning and health.Footnote 77 Women living in communities with supportive attitudes towards mammography have been found to make greater use of mammography screening than those living in communities where there is less support for this preventive technology.Footnote 88
Health beliefs are an important determinant of health services utilization. For example, rural Australians tend to regard health in negative terms, i.e. the absence of disease,Footnote 99 and, as a result, the primary focus for rural residents might be to cure illness and to relieve symptoms and discomfort, rather than to prevent illness or to maintain health.Footnote 1010 Traditional rural values such as self-reliance, independence and a preference for informal support networks may also lead to underuse of preventive or other health services unless there is a serious impairment to health.
Enabling factors
Poor transportation is one of rural residents' major concerns in relation to access to health services,Footnote 1111 and in many rural communities across Canada public transport services have been reduced or have become more costly. However, some provincial programs have been introduced to facilitate access to health care. For instance, in Ontario there are physician outreach programs and visiting specialist clinics as part of the Underserviced Area Program. In other provinces and territories, patient travel assistance is offered so that rural residents can access health services that are not available locally. The effects are measurable: for example, rates of mammography screening in rural areas in Manitoba have increased with the use of mobile screening units.Footnote 1212,Footnote 13a13a
Privacy issues may also deter some rural residents from seeking health care if a small population and close-knit community make anonymity less likely. Privacy is more crucial to decisions about whether to seek medical care among young women in rural areas than among their urban counterparts. Footnote 1414
Needs
Health care resources spent on Canadians with chronic disease account for 67% of total direct health care costs and 60% of indirect costs through lost productivity and income.Footnote 1515 In general, the mortality risks due to chronic conditions such as circulatory diseases, respiratory diseases and diabetes are higher among rural residents than among urban ones.Footnote 1b1b Other studies have shown that greater proportions of people in rural or northern areas report poor or fair health status, activity limitations and living with disabilities.Footnote 16a–1816a–18 All else being equal, people with worse health conditions or greater needs are more likely to require medical attention or other health services.
Use of health services
There is a paucity of national data on the patterns of health services use by rural Canadians, though individual provinces have investigated physician visits and hospital admission data. For instance, in 2000, residents of rural and northern regions in Manitoba were found to have lower rates than the provincial average for use of physician services, ambulatory visit rates and ambulatory consultation rates;Footnote 13b13b in Ontario, discharge rates for rural residents from acute care hospitals were almost 50% higher than the provincial average.Footnote 17b17b In Quebec, the rates of hospital discharge have also been found to be higher in rural areas, even though the average length of hospital stay was shorter than for urban residents.Footnote 16b16b Also, rural hospital emergency departments see higher proportions of patients who are deemed to require non-urgent care (i.e. for which interventions could be delayed) than do emergency departments in urban areas.Footnote 1919
Objectives of this study
Building on the framework, this study aims to assess the national patterns of health services utilization by rural Canadians and compare them with those of city dwellers by using the results of both descriptive and bivariate analyses of selected measures of health services use and the findings from multivariate regression analyses of related factors.
We considered the following research questions:
- How do the patterns of utilization of medical and other health services, including in-patient hospital services, differ between rural and urban Canada?
- In addition to urban-rural differences in health services utilization, are there intra-rural variations?
- Are the patterns of utilization by rural and urban Canadians different for different disease categories?
- What are the geographic patterns of utilization of physician and hospital services at the provincial level in Nova Scotia, Ontario and British Columbia?
- Is place of residence a determinant of health services use?