Original quantitative research – Characteristics of vulnerable women and their association with participation in a Canada Prenatal Nutrition Program site in Toronto, Canada

HPCDP Journal Home
Published by: The Public Health Agency of Canada
Date published: December 2021
ISSN: 2368-738X
Submit a manuscript
About HPCDP
Browse
Previous | Table of Contents | Next
Jane Francis, PhDAuthor reference footnote 1Author reference footnote 2; Samantha Ismail, BScAuthor reference footnote 1; Alison Mildon, MScAuthor reference footnote 1; Stacia StewartAuthor reference footnote 3; Bronwyn Underhill, MHScAuthor reference footnote 3; Valerie Tarasuk, PhDAuthor reference footnote 1Author reference footnote 4Author reference footnote 5; Erica Di Ruggiero, PhDAuthor reference footnote 4; Alex Kiss, PhDAuthor reference footnote 6; Daniel W. Sellen,Author reference footnote * PhDAuthor reference footnote 1Author reference footnote 4Author reference footnote 5Author reference footnote 7; Deborah L. O’Connor,Author reference footnote * PhDAuthor reference footnote 1Author reference footnote 2Author reference footnote 5Author reference footnote 8
https://doi.org/10.24095/hpcdp.41.12.02
This article has been peer reviewed.
Author references
Correspondence
Deborah L. O’Connor, Department of Nutritional Sciences, University of Toronto, Medical Sciences Building, Room 5253, 1 King’s College Circle, Toronto, ON M5S 1A8; Tel: 416-978-7235; Email: deborah.oconnor@utoronto.ca
Suggested citation
Francis J, Ismail S, Mildon A, Stewart S, Underhill B, Tarasuk V, Di Ruggiero E, Kiss A, Sellen DW, O’Connor DL. Characteristics of vulnerable women and their association with participation in a Canada Prenatal Nutrition Program site in Toronto, Canada. Health Promot Chronic Dis Prev Can. 2021;41(12):413-22. https://doi.org/10.24095/hpcdp.41.12.02
Abstract
Introduction: The Canada Prenatal Nutrition Program (CPNP) supports community organizations to provide maternal–infant health services for socially/economically vulnerable women. As part of our research program exploring opportunities to provide postnatal breastfeeding support through the CPNP, we investigated the sociodemographic and psychosocial characteristics of clients enrolled in a Toronto CPNP site and explored associations with participation.
Methods: Data were collected retrospectively from the charts of 339 women registered in one southwest Toronto CPNP site from 2013 to 2016. Multivariable regression analyses were used to assess associations between 10 maternal characteristics and three dimensions of prenatal program participation: initiation (gestational age at enrolment in weeks), intensity (number of times one-on-one supports were received) and duration (number of visits).
Results: The mean (SD) age of clients was 31 (5.7) years; 80% were born outside of Canada; 29% were single; and 65% had household incomes below the Statistics Canada family size-adjusted low-income cut-offs. Income was the only characteristic associated with all dimensions of participation. Compared to clients living above the low-income cut-off, those living below the low-income cut-off enrolled in the program 2.85 weeks earlier (95% CI: −5.55 to −0.16), had 1.29 times higher number of one-on-one supports (95% CI: 1.03 to 1.61) and had 1.29 times higher number of program visits (95% CI: 1.02 to 1.63).
Conclusion: Our findings show that this CPNP site serves vulnerable women, with few differences in participation based on maternal characteristics. This evidence can guide service provision and monitoring decisions at this program site. Further research is needed to explore new program delivery models to enhance perinatal services for vulnerable women.
Keywords: vulnerable populations, prenatal program, program evaluation, Canada Prenatal Nutrition Program, CPNP, pregnant women
Highlights
- Clients registered at one Canada Prenatal Nutrition Program (CPNP) site in Toronto reported a variety of vulnerabilities. For example, 80% were not born in Canada and 65% were living in low-income households.
- Of 10 maternal characteristics investigated, household income was the only one associated with all three prenatal participation measures; women living in low-income households enrolled in the program earlier in pregnancy, had a higher number of one-on-one contacts with program staff and a higher number of visits to the program.
- Integrating additional supports at this program site could be explored as a way to extend perinatal services to vulnerable women.
Introduction
The federally funded Canada Prenatal Nutrition Program (CPNP) was established in 1995 to support community-based organizations in developing or expanding health interventions for vulnerable pregnant women across the country.Footnote 1 The CPNP specifically aims to increase healthy birth weights and promote and support breastfeeding among socially and/or economically vulnerable women, including those with lower income and education and/or who are substance users, newcomers, lone parents and adolescents.
There are over 240 CPNP sites serving about 45 000 women annually across Canada.Footnote 2 All the sites are unique as the range of services they provide depend on local needs, but all the services are implemented based on the overarching CPNP guiding principles, program objectives and core services. Core services include group education on nutrition and health; provision of food/grocery gift cards; one-on-one support; and community referrals.
The only national CPNP impact evaluation was based on 48 184 participants between 2002 and 2006. The evaluation utilized an exposure index created by combining three dimensions of participation: gestational age at program enrolment (initiation); number of contacts with program staff (intensity); and number of program visits (duration).Footnote 3 Each dimension was split at the median to create a “high” and “low” category (i.e. participants who enrolled at an earlier gestational age versus a later one; had a higher number of contacts with staff versus a lower number of contacts; and had a higher number of visits versus a lower number of visits). CPNP participants in the “high” category for at least two dimensions were considered to have high CPNP exposure.
This evaluation found that, compared with low CPNP exposure, high exposure improved maternal health behaviours, including breastfeeding initiation and duration to 6 weeks, and prenatal supplement use.Footnote 3 High CPNP exposure was also associated with a reduction in preterm, low-birth-weight and small-for-gestational-age infants.Footnote 3
Although these data suggest benefits of CPNP participation, breastfeeding remains an ongoing public health issue. According to the 2017/2018 Canadian Community Health Survey, 91% of mothers start breastfeeding, but only 34% exclusively breastfeed for the recommended six months.Footnote 4 Breastfeeding practices (initiation, duration, exclusivity) are influenced by a range of determinants (e.g. individual factors, such as age, education, income; the health system; sociocultural attitudes) and are lowest among vulnerable women.Footnote 5Footnote 6Footnote 7Footnote 8 As an example, national data indicate that women with lower income and education are less likely to breastfeed exclusively for 6 months.Footnote 7Footnote 8 These data suggest there remains unmet potential for the CPNP to support vulnerable women to breastfeed, and thereby, contribute more to reducing disparities in breastfeeding practices. Currently, the CPNP does not have a formal framework or funding for sites to provide postnatal lactation support.
Our research program aims to evaluate opportunities to improve breastfeeding practices among vulnerable women in Canada by strengthening the delivery of skilled postnatal lactation support (e.g. emotional, practical, informational and social support provided by trained individuals) through the CPNP, primarily through in-home visits by International Board Certified Lactation Consultants.Footnote 9 Although high CPNP exposure has been associated with improved perinatal health behaviours and outcomes,Footnote 3 little is known on the vulnerability profile of clients at specific sites or how maternal characteristics may affect program participation. A better understanding of who is participating in CPNPs, and how engaged they are, is a necessary step towards strengthening the program, including the delivery of proactive postnatal lactation support.
Our aim for this study was to (1) describe the sociodemographic and psychosocial characteristics of clients enrolled in one Toronto CPNP site; and (2) determine which maternal sociodemographic and psychosocial characteristics were associated with dimensions of CPNP participation at this site.
Methods
We conducted a chart review of routinely collected data from a CPNP site in Toronto, Ontario, implemented by Parkdale Queen West Community Health Centre (the Parkdale Parents’ Primary Prevention Project, or 5Ps), which has served families in the southwest area of Toronto for over 25 years. We retrospectively extracted data from archived intake forms, support logs and attendance records of clients who registered in the 5Ps CPNP between 2013 and 2016 and signed the program consent for their de-identified data to be used for evaluation purposes.
For clients who enrolled in the 5Ps CPNP for more than one pregnancy during the study timeframe, only their first pregnancy at the program was included in the study. Clients were also excluded if they were ineligible for the 5Ps CPNP due to miscarriage or referral to another CPNP site, or if their intake form was incomplete.
Description of the 5Ps CPNP
The 5Ps CPNP catchment area included densely populated, ethnically diverse neighbourhoods, one of which was designated a “neighbourhood improvement area” by the City of Toronto.Footnote 10Footnote 11 The site was staffed with individuals experienced in community programming and working with vulnerable families. The sole family support and outreach worker identified pregnant women in the catchment area by distributing flyers to medical walk-in clinics, family physician offices, the local hospital, obstetrics and gynecology offices and residential buildings over 2 days per month. Based on anecdotal reports, a large proportion of women learned about the program by word of mouth.
Weekly services at the 5Ps CPNP included group education sessions, individualized support from public health nurses and dietitians, community referrals, and a self-serve food bank. Participants were given one $10 grocery store gift card and two public transit tokens per visit and offered snacks and onsite childcare. Professional interpreters were available in-person for non-English speaking clients; previous studies conducted at this CPNP site reported that 7–10% of women required an interpreter.Footnote 12Footnote 13 Women could register at any point during their pregnancy, and there was no limit on the number of times they could attend during their pregnancy.
Data sources
Routine intake forms, administered by program staff at enrolment, collected data on clients’ sociodemographic and psychosocial characteristics. Each client’s chart also contained a log of one-on-one supports provided by 5Ps CPNP staff each week during the program. Examples of one-on-one supports included community referrals (e.g. public health program, shelter), health counselling and nutrition counselling. Clients could seek out program staff for one-on-one support, or staff could approach clients based on information provided during intake or when they attended the program. Individual attendance was tracked electronically each week.
Ethics approval
Ethics approval was obtained from the Office of Research Ethics at the University of Toronto (34482). Upon enrolment in the 5Ps CPNP, clients were asked if their de-identified information could be used for program evaluation. Data for the current study were only extracted from the charts of clients who signed this consent form.
Primary outcome measures
Based on the only previous CPNP impact evaluationFootnote 3 and data availability, we constructed indicators of three key dimensions of prenatal participation in the 5Ps CPNP: initiation, intensity and duration. Initiation was determined by the estimated gestational age in weeks upon program enrolment, as recorded on client intake forms.
Intensity was determined by the number of times clients received one-on-one supports from 5Ps CPNP staff according to their support log. One-on-one support interactions were recorded under 12 categories defined by program staff. Group services provided to all clients (described in “Description of the 5Ps CPNP”) were not recorded in individual support logs and were not counted as one-on-one supports in our analyses.
Duration was determined by the actual number of weeks clients attended the 5Ps CPNP, from enrolment to delivery, according to attendance records.
While there is potential for redundancy over these three dimensions of participation, there is value in exploring participation from different angles given the overall limited evaluation of participation in CPNP programs.
Independent variables
We extracted self-reported maternal sociodemographic and psychosocial characteristics from 5Ps CPNP intake forms. Maternal characteristics common to all versions of intake forms between 2013 and 2016 and that could therefore be extracted included:
- maternal age (years, continuous variable);
- years in Canada (born in Canada or, for those not born in Canada, <1 year, 1–3 years or ≥4 years);
- refugee status (yes/no response to the question, “Did you arrive in Canada as a refugee or refugee claimant?”);
- history of mental illness (yes/no response to the question, “Have you ever experienced or been diagnosed with depression, postpartum depression or a mental health concern?”);
- education (less than high school, high school or postsecondary);
- marital status (single or living with partner);
- number of children (first-time mother or has 1 child or more);
- food deprivation during pregnancy (yes/no response to the question, “During your pregnancy, was there ever a time when you did not have enough food to eat?”);
- abuse during pregnancy (yes/no response to the question, “From the beginning of your pregnancy, has anyone abused you physically, sexually or emotionally?”);
- Ontario Health Insurance Program (OHIP) coverage (yes/no);
- household income (above low-income cut-off, below low-income cut-off or don’t know income; assessed using the Statistics Canada family size-adjusted low-income cut-off values corresponding to clients’ year of program enrolment.Footnote 14Footnote 15Footnote 16 For example, a family of four with a household income less than $39 092 in 2016 would be living below the low-income cut-offFootnote 16);
- ethnicity (East Asian, African, European, South Asian, Latin American, Caribbean, Southeast Asian, West Asian or Other; categorized based on United Nations geographic regions of the worldFootnote 17).
Statistical analysis
We reported sociodemographic and psychosocial characteristics and 5Ps CPNP participation measures using descriptive statistics.
We assessed the association between maternal characteristics and the three dimensions of 5Ps CPNP participation (initiation, intensity and duration) as outcome variables. The continuous initiation variable was analyzed using a multivariable linear regression model. Results were reported using parameter estimates with 95% confidence intervals (CI). Count data (intensity and duration) were analyzed using multivariable Poisson regression models instead of linear regression models as the data did not follow a normal distribution. The Poisson models were adjusted for overdispersion using Pearson scaling, and model fit was assessed using a goodness-of-fit chi-square test. Results were reported using incidence rate ratios (IRR) with 95% CI.
For all analyses, the reference category for each categorical independent variable was the less vulnerable group (e.g. above the low-income cut-off). All independent variables were considered in the analyses except for abuse during pregnancy (frequency less than 10%) and ethnicity (predominance of one ethnic group and frequency less than 10% among the remaining categories). Independent variables used in the analyses were checked for statistical multicollinearity (variance inflation factor >2.5), and none met this criterion.
SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used to conduct the statistical analyses. A p value of less than 0.05 was considered statistically significant.
We used the k-nearest-neighbours (KNN) algorithm to impute missing independent variables using the VIM package in R software version 3.5.1 (R Foundation, Vienna, AT)Footnote 18 and conducted sensitivity analyses for all models using the original dataset (no imputations).
Results
Study sample
We assessed 370 clients for eligibility and excluded 31 for the following reasons: 10 clients did not consent for their charts to be used for program evaluation purposes; 10 had a subsequent pregnancy during the study timeframe and their data were only included once; seven had a pregnancy loss or were not pregnant; three were referred to a CPNP site closer to their place of residence; and one did not have any information on their intake form. A total of 339 clients were included in the analyses (see Figure 1). Of these, 16 consented to partial use of data and were therefore excluded from the intensity analysis.
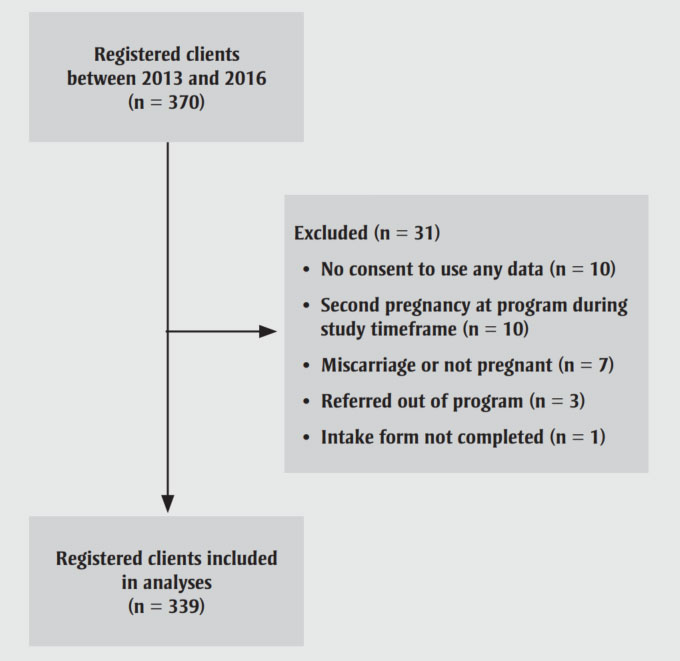
Figure 1 - Text description
This figure shows the process through which clients registered in the Parkdale Parents’ Primary Prevention Project (5Ps), within the Canada Prenatal Nutrition Program (CPNP), were selected for inclusion in the analyses. During the study timeframe (2013–2016, inclusive), 370 available client charts were assessed for eligibility. A total of 31 charts were excluded from the analyses for the following reasons: 10 clients did not consent for their charts to be used for program evaluation purposes; 10 clients had a subsequent pregnancy at the prenatal program during the study timeframe and were only included once; 7 clients had a pregnancy loss or were not pregnant; 3 clients were referred to CPNP site closer to their place of residence; and 1 client did not have any information available on their intake form. A total of 339 clients were included in the analyses.
Abbreviations: 5Ps, Parkdale Parents’ Primary Prevention Project; CPNP, Canada Prenatal Nutrition Program.
The mean (SD) age of clients at enrolment was 31 (5.7) years. Only 16% (54/339) were born in Canada, and 33% (111/339) had lived in Canada for 3 years or less (Table 1). Of all the participants in the analyses, 47% (159/339) had high school education or less and 29% (97/339) were single. Of those who reported household income, 78% (220/281) were below the low-income cut-off.
| CharacteristicsFootnote a | n | % |
|---|---|---|
| Number of years in Canada | ||
| Born in Canada | 54 | 15.9 |
| <1 | 53 | 15.6 |
| 1–3 | 58 | 17.1 |
| ≥4 | 159 | 46.9 |
| Missing | 15 | 4.4 |
| Refugee status | ||
| Yes | 47 | 13.9 |
| No | 263 | 77.6 |
| Missing | 29 | 8.6 |
| History of mental illness | ||
| Yes | 57 | 16.8 |
| No | 263 | 77.6 |
| Missing | 19 | 5.6 |
| Completed education | ||
| <High school | 40 | 11.8 |
| High school | 119 | 35.1 |
| Postsecondary | 170 | 50.1 |
| Missing | 10 | 2.9 |
| Marital status | ||
| Single | 97 | 28.6 |
| With partner | 225 | 66.4 |
| Missing | 17 | 5.0 |
| Number of children | ||
| First-time mother | 169 | 49.9 |
| ≥1 child | 157 | 46.3 |
| Missing | 13 | 3.8 |
| Food deprivation during pregnancy | ||
| Yes | 97 | 28.6 |
| No | 218 | 64.3 |
| Missing | 24 | 7.1 |
| Abuse during pregnancy | ||
| Yes | 24 | 7.1 |
| No | 294 | 86.7 |
| Missing | 21 | 6.2 |
| OHIP coverage | ||
| Yes | 279 | 82.3 |
| No | 46 | 13.6 |
| Missing | 14 | 4.1 |
| Household incomeFootnote b | ||
| Below low-income cut-off | 220 | 64.9 |
| Above low-income cut-off | 61 | 18.0 |
| Don’t knowFootnote c | 50 | 14.7 |
| Missing | 8 | 2.4 |
| Ethnicity | ||
| East Asian | 109 | 32.2 |
| African | 39 | 11.5 |
| European | 32 | 9.4 |
| South Asian | 31 | 9.1 |
| Latin American | 22 | 6.5 |
| Caribbean | 20 | 5.9 |
| Southeast Asian | 14 | 4.1 |
| West Asian | 13 | 3.8 |
| OtherFootnote d | 49 | 14.5 |
| MissingFootnote e | 10 | 2.9 |
Abbreviations: 5Ps, Parkdale Parents’ Primary Prevention Project; CPNP, Canada Prenatal Nutrition Program; OHIP, Ontario Health Insurance Program.
|
||
Initiation
The median gestational age at enrolment in the 5Ps CPNP was 25 weeks (interquartile range [IQR] 17–30). Only 15% (50/336) enrolled during their first trimester of pregnancy (1–12 weeks); 53% (179/336) enrolled during their second trimester (13–28 weeks) and 32% (107/336) during their third trimester (29–40 weeks).
The linear regression model showed no difference in initiation based on maternal age, number of years in Canada, refugee status, marital status, food deprivation or OHIP coverage (Table 2). Clients who reported a history of mental illness enrolled in the 5Ps CPNP earlier than those with no history of mental illness (parameter estimate = −3.19 weeks; 95% CI: −5.71 to −0.67). Clients living below the low-income cut-off, compared to above the low-income cut-off, also enrolled in the program earlier (parameter estimate = −2.85 weeks; 95% CI: −5.55 to −0.16). Clients with less than high school education enrolled in the program later than those with postsecondary education (parameter estimate = 3.48 weeks; 95% CI: 0.20 to 6.76). Lastly, compared to clients with at least one child, first-time mothers also enrolled in the program later (parameter estimate = 3.20 weeks; 95% CI: 1.21 to 5.19).
| Characteristics | InitiationFootnote a | IntensityFootnote b | DurationFootnote b | |||
|---|---|---|---|---|---|---|
| Parameter estimate | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Maternal age, years | 0.10 | −0.08 to 0.28 | 1.00 | 0.98 to 1.01 | 1.00 | 0.98 to 1.01 |
| Number of years in Canada | ||||||
| <1 vs. Born in Canada (ref.) | 1.29 | −2.55 to 5.14 | 1.14 | 0.84 to 1.54 | 1.16 | 0.84 to 1.59 |
| 1–3 vs. Born in Canada (ref.) | 0.90 | −2.65 to 4.44 | 0.98 | 0.74 to 1.32 | 1.06 | 0.79 to 1.43 |
| ≥4 vs. Born in Canada (ref.) | 1.55 | −1.52 to 4.62 | 1.01 | 0.80 to 1.28 | 1.04 | 0.80 to 1.35 |
| Refugee status | ||||||
| Yes vs. No (ref.) | 1.00 | −1.85 to 3.85 | 0.72Footnote * | 0.56 to 0.92Footnote * | 0.93 | 0.73 to 1.18 |
| History of mental illness | ||||||
| Yes vs. No (ref.) | −3.19Footnote * | −5.71 to −0.67Footnote * | 1.16 | 0.95 to 1.42 | 0.93 | 0.75 to 1.16 |
| Completed education | ||||||
| < High school vs. Postsecondary (ref.) | 3.48Footnote * | 0.20 to 6.76Footnote * | 1.05 | 0.82 to 1.34 | 0.87 | 0.66 to 1.15 |
| High school vs. Postsecondary (ref.) | −0.77 | −2.94 to 1.41 | 0.95 | 0.80 to 1.12 | 1.06 | 0.90 to 1.26 |
| Marital status | ||||||
| Single vs. With partner (ref.) | 2.15 | −0.07 to 4.38 | 0.99 | 0.84 to 1.18 | 0.76Footnote * | 0.63 to 0.92Footnote * |
| Number of children | ||||||
| First-time mother vs. ≥1 child (ref.) | 3.20Footnote * | 1.21 to 5.19Footnote * | 0.99 | 0.84 to 1.15 | 0.88 | 0.75 to 1.03 |
| Food deprivation during pregnancy | ||||||
| Yes vs. No (ref.) | 0.40 | −1.88 to 2.68 | 0.96 | 0.80 to 1.14 | 0.99 | 0.82 to 1.19 |
| OHIP coverage | ||||||
| No vs. Yes (ref.) | 1.28 | −1.83 to 2.68 | 1.07 | 0.85 to 1.35 | 0.79 | 0.60 to 1.02 |
| Household incomeFootnote c | ||||||
| Below vs. Above LICO (ref.) | −2.85Footnote * | −5.55 to −0.16Footnote * | 1.29Footnote * | 1.03 to 1.61Footnote * | 1.29Footnote * | 1.02 to 1.63Footnote * |
| Don't knowFootnote d vs. Above LICO (ref.) | −3.48Footnote * | −6.71 to −0.25Footnote * | 1.10 | 0.84 to 1.45 | 1.21 | 0.93 to 1.58 |
Abbreviations: 5Ps, Parkdale Parents’ Primary Prevention Project; CI, confidence interval; CPNP, Canada Prenatal Nutrition Program; IRR, incidence rate ratio; LICO, low-income cut-off; OHIP, Ontario Health Insurance Program; ref., reference.
|
||||||
Intensity
The median number of times clients received one-on-one supports from 5Ps CPNP staff was four (IQR 2–6).
The top three one-on-one supports included community referrals (e.g. public health programs such as Healthy Babies Healthy Children), follow-up on referrals and health counselling from a public health nurse (e.g. prenatal care, breastfeeding information; see Table 3). Only 2% (6/323) of clients received no one-on-one supports, 34% (109/323) received one to three different types of one-on-one supports, 52% (167/323) received four to six different types of one-on-one supports and 13% received seven to nine different types of one-on-one supports (41/323).
| One-on-one support type | n (N = 323)Footnote a | % |
|---|---|---|
| Follow-up on referral | 231 | 71.5 |
| Health counselling | 217 | 67.2 |
| Community referral (e.g. public health program, shelter) | 212 | 65.6 |
| Extra food/nutrition or instrumental supports | 168 | 52.0 |
| Participant advocacy | 168 | 52.0 |
| Nutrition counselling | 142 | 44.0 |
| Settlement support | 96 | 29.7 |
| Mental health support | 93 | 28.8 |
| Child development advice | 15 | 4.6 |
| Case management/service coordination | 14 | 4.3 |
| Crisis intervention | 4 | 1.2 |
| Other | 30 | 9.3 |
Abbreviations: 5Ps, Parkdale Parents’ Primary Prevention Project; CPNP, Canada Prenatal Nutrition Program.
|
||
The Poisson regression model showed no difference in intensity (determined by the number of times the client received one-on-one supports from program staff) based on maternal age, number of years in Canada, history of mental illness, education, marital status, number of children, food deprivation or OHIP coverage (Table 2). Refugee clients had fewer one-on-one contacts with program staff than did non-refugees (IRR = 0.72; 95% CI: 0.56 to 0.92). Clients living below the low-income cut-off, compared to above, had a higher number of one-on-one contacts (IRR = 1.29; 95% CI: 1.03 to 1.61).
Duration of attendance
The median attendance in the 5Ps CPNP was 9 weeks (IQR 4–14).
The Poisson regression model showed no difference in duration of attendance based on maternal age, number of years in Canada, refugee status, history of mental illness, education, number of children, food deprivation or OHIP coverage (Table 2). Mothers who were single attended the program for fewer weeks than those with a partner (IRR = 0.76; 95% CI: 0.63 to 0.92). Clients living below the low-income cut-off, compared to above, attended the program for a higher number of weeks (IRR = 1.29; 95% CI: 1.02 to 1.63).
Sensitivity analyses
We conducted sensitivity analyses using the original dataset without imputations for missing data to assess associations between sociodemographic and psychosocial characteristics and 5Ps CPNP initiation (n = 280/339), intensity (n = 282/339) and duration (n = 282/339) (Table 4). These analyses generally showed consistent results with our imputed analyses. Table 1 shows the proportion of missing values for each independent variable.
| Characteristics | InitiationFootnote b | IntensityFootnote c | DurationFootnote c | |||
|---|---|---|---|---|---|---|
| Parameter estimate | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Maternal age, years | 0.14 | −0.06 to 0.33 | 1.00 | 0.99 to 1.02 | 1.00 | 0.98 to 1.01 |
| Number of years in Canada | ||||||
| <1 vs. Born in Canada (ref.) | 0.69 | −3.81 to 5.19 | 1.08 | 0.79 to 1.50 | 1.31 | 0.94 to 1.84 |
| 1–3 vs. Born in Canada (ref.) | −0.12 | −4.26 to 4.01 | 0.91 | 0.67 to 1.25 | 1.16 | 0.84 to 1.59 |
| ≥4 vs. Born in Canada (ref.) | 1.48 | −2.01 to 4.97 | 0.92 | 0.72 to 1.19 | 1.04 | 0.79 to 1.36 |
| Refugee | ||||||
| Yes vs. No (ref.) | 1.13 | −1.97 to 4.22 | 0.73Footnote * | 0.57 to 0.95Footnote * | 0.91 | 0.71 to 1.16 |
| History of mental illness | ||||||
| Yes vs. No (ref.) | −3.27Footnote * | −6.44 to −0.10Footnote * | 1.13 | 0.89 to 1.42 | 0.96 | 0.75 to 1.23 |
| Completed education | ||||||
| <High school vs. Postsecondary (ref.) | 3.52 | −0.003 to 7.05 | 1.06 | 0.82 to 1.37 | 0.83 | 0.63 to 1.10 |
| High school vs. Postsecondary (ref.) | −1.80 | −4.17 to 0.58 | 0.94 | 0.78 to 1.12 | 1.13 | 0.95 to 1.35 |
| Marital status | ||||||
| Single vs. With partner (ref.) | 1.71 | −0.73 to 4.15 | 0.95 | 0.79 to 1.14 | 0.79Footnote * | 0.65 to 0.96Footnote * |
| Number of children | ||||||
| First-time mother vs. ≥1 child (ref.) | 3.49Footnote * | 1.30 to 5.68Footnote * | 0.98 | 0.83 to 1.16 | 0.88 | 0.75 to 1.03 |
| Food deprivation during pregnancy | ||||||
| Yes vs. No (ref.) | −0.10 | −2.63 to 2.42 | 0.93 | 0.78 to 1.13 | 1.04 | 0.86 to 1.25 |
| OHIP coverage | ||||||
| No vs. Yes (ref.) | 0.67 | −2.68 to 4.02 | 1.15 | 0.91 to 1.46 | 0.79 | 0.61 to 1.02 |
| Household incomeFootnote d | ||||||
| Below vs. Above LICO (ref.) | −1.23 | −4.28 to 1.81 | 1.25 | 0.99 to 1.59 | 1.18 | 0.93 to 1.51 |
| Don't knowFootnote e vs. Above LICO (ref.) | −3.08 | −6.68 to 0.52 | 1.11 | 0.83 to 1.47 | 1.19 | 0.90 to 1.58 |
Abbreviations: 5Ps, Parkdale Parents’ Primary Prevention Project; CI, confidence interval; CPNP, Canada Prenatal Nutrition Program; IRR, incidence rate ratio; LICO, low-income cut-off; OHIP, Ontario Health Insurance Program; ref., reference.
|
||||||
Discussion
This study investigated the sociodemographic and psychosocial characteristics of clients enrolled in the 5Ps CPNP site in Toronto, Ontario, and the association between these characteristics and dimensions of prenatal program participation. We found that 5Ps CPNP participants included a diversity of women with a range of vulnerabilities. Overall, household income was the only characteristic associated with all three dimensions of program participation. Household income below the low-income cut-off was associated with enrolment earlier in pregnancy, a higher number of one-on-one contacts with program staff and a longer duration of program attendance.
It is encouraging that a history of mental illness was associated with earlier enrolment in the 5Ps CPNP and that a household income below the low-income cut-off was associated with better program engagement overall according to our three dimensions of participation. This suggests that the program’s social and tangible supports may be relevant to women with these characteristics and help meet their needs. Nevertheless, to enhance program participation among all registered clients, several subgroups may need to be targeted. According to our results, having no high school education and being a first-time parent was associated with later program initiation, while single marital status was associated with a shorter duration of program attendance. Further research should explore the needs of enrolled clients and barriers to their participation.
Our results indicate that refugee status was associated with having fewer one-on-one contacts with 5Ps CPNP staff. Staff experience (co-authors SS and BU) suggests that this is likely due to one of two possible reasons. First, many refugee clients are referred to the program from shelters and have access to various supports within the shelter system. Second, there is no in-house settlement support at the 5Ps CPNP; therefore, program staff often refer refugee clients who are not connected to the shelter system to a settlement service that can provide support that is more comprehensive to clients’ needs.
Given the diversity of the Canadian population, the risk profile of program participants likely differs between CPNP sites across the country and across time. Limited published information is available on the characteristics of women enrolled in individual CPNP sites, making it challenging to compare our cohort with CPNP participants at other sites. National data from a 2015 CPNP participant survey found that 66% of clients had incomes below the low-income cut-off; 26% had less than high school education; 27% were single; 16% were recent immigrants (in Canada <10 years); and 41% experienced food insecurity.Footnote 19 Food insecurity was characterized by an affirmative response to not having enough food for themselves/their family and no money to buy more in the previous 12 months.
In comparison to this national profile of CPNP clients, a similar proportion of our study participants had incomes below the low-income cut-off (65%) and were single (29%). Whereas 30% of study participants experienced food deprivation during pregnancy, in comparison to 41% of national CPNP clients who reported food insecurity, our rate refers specifically to the maternal experience.
In our cohort, a smaller proportion of mothers had less than high school education (12%) and a higher proportion were newcomers to Canada (33% lived in Canada ≤3 years).
This analysis focussed on the maternal characteristics of registered 5Ps CPNP clients and on their participation in this prenatal program. No research was conducted among women who were eligible but did not participate and so we were unable to determine the reach or uptake of the 5Ps CPNP. Levels of uptake of the national CPNP by target populations are also unknown. We do know that vulnerable women are participating in the CPNP, based on the demographics of program participants,Footnote 19 but further research on who is not enrolling in the CPNP, locally and nationally, and their reasons for this, would be valuable for strengthening programs and improving program monitoring and evaluation. Other studies have identified gaps in coverage of perinatal services in vulnerable populations, including a population-based study that found 78% of women receiving income assistance did not participate in Manitoba’s Healthy Baby community support programs that attempt to reach vulnerable women.Footnote 20
Overall, study participants engaged with the 5Ps CPNP later in their pregnancy, with a median gestational age at enrolment of 25 weeks and a median duration of attendance of nine visits. There is no known participation “threshold” for the CPNP, that is, it is unknown at what gestational age women should enrol or the number of visits needed to attain a specific health or social outcome. It would be expected that the participation threshold would vary for each woman according to her individual needs and risk profile. Nevertheless, efforts to engage vulnerable women in community programming during pregnancy are needed to improve birth and health outcomes.Footnote 21Footnote 22Footnote 23 In addition, the collection of outcome data across CPNP sites is limited and not standardized, and there is a need for an updated national evaluation.
Although not directly comparable to participation in community prenatal programs, studies have identified a range of maternal risk factors for late or inadequate utilization of available prenatal care. These risk factors typically include characteristics of vulnerability such as having lower education status, lower income or no health insurance or being a refugee or single.Footnote 24Footnote 25Footnote 26Footnote 27Footnote 28 Strategies to further engage vulnerable women in prenatal care and facilitate enrolment and retention in prenatal community support programs are needed. Primary and community health services (e.g. family doctors, obstetricians, social workers, community health centres) should be well connected to, and create partnerships with, CPNP sites in their geographic area to facilitate program referrals.Footnote 29 The experience of 5Ps CPNP staff suggests that an existing and trusting relationship between vulnerable women and community health care and social providers is important so that women who are referred to the CPNP feel comfortable accessing the program, but further research is needed to confirm this.
We conducted this research as one step towards gauging whether the CPNP can be leveraged to strengthen access to proactive postnatal lactation support for vulnerable women. Over three-quarters of the study participants (79%) went on to attend some type of postnatal drop-in program at the community health centre at least once, suggesting interest in continuing engagement with this site. Further research is needed to explore program delivery models for integrating in-home lactation support with the 5Ps CPNP as a program enhancement.
Canadian data show that more work needs to be done to align breastfeeding practices with public health recommendations.Footnote 4Footnote 30 Data on infant feeding practices of CPNP participants are limited and should be further explored. Breastfeeding initiation by CPNP clients is comparable to the 91% national rate, but breastfeeding duration and exclusivity are unknown.Footnote 4Footnote 19 Muhajarine et al.Footnote 31 found that, despite an 89% breastfeeding initiation rate by CPNP participants nationally, 60% of the mothers discontinued breastfeeding by 4 weeks postpartum. Systematic reviews confirm the importance of postnatal breastfeeding support for improving breastfeeding practices.Footnote 32Footnote 33 The CPNP’s established program and social support structure and stated aim to support breastfeeding positions it well to address ongoing disparities in breastfeeding rates.Footnote 2Footnote 34 We found that the 5Ps CPNP is serving a diverse group of vulnerable women with few differences in participation based on maternal characteristics. These findings provide information that can be used to support program enhancements at this site, including those that extend to the postnatal period. It would be valuable for other CPNP sites to analyze sociodemographic and psychosocial characteristics of participants and investigate associations with participation to inform program delivery strategies. In-depth assessment of engagement in specific CPNP program components may also be valuable.
Strengths and limitations
To our knowledge, this is the first study to investigate the association between maternal characteristics and participation in a CPNP site. A strength of this research is the focus on vulnerable women’s participation in a community prenatal program targeting this group specifically. Another strength is the use of existing program data sources, resulting in a cost-efficient strategy that can inform service provision at this site and strengthen future monitoring efforts at the community level.
In terms of limitations, all sociodemographic and psychosocial characteristics were self-reported by participants and could not be independently verified. We were also limited by the fact that we could not collect additional details on maternal characteristics beyond what was collected as part of the site’s standard intake form. In addition, no information was available on motivators for attending the 5Ps CPNP or accessing one-on-one support at the program.
Given limitations of our sample size and potential redundancy between the three dimensions of participation, we were unable to create a combined indicator to analyze program participation as a dichotomous high/low exposure variable as others have done.Footnote 3 However, all registered clients in the study period were considered for inclusion in this study and 92% (339/370) were included. Most of those who were excluded were ineligible for the 5Ps CPNP (e.g. they were not pregnant) or were having a repeat pregnancy and were therefore already included in the study on the basis of the previous pregnancy. Thus, selection bias is expected to be minimal.
This study was based on data from one CPNP site and may not be generalizable to other sites. However, the 5Ps CPNP catchment area is in a densely populated, ethnically diverse urban area of Toronto (population >88 000) and is one of the larger CPNP sites in the city.
Conclusion
Our findings confirm that a diversity of women with a range of vulnerabilities enrolled in the 5Ps CPNP site in Toronto, with few differences in participation based on maternal characteristics. Overall, mothers with incomes below the low-income cut-off enrolled in the program earlier in their pregnancy, had a higher number of one-on-one contacts with program staff and attended the program for a longer duration. We found that women with less than a high school education and no previous children may need to be further supported to enrol in the 5Ps CPNP earlier in pregnancy, while lone parents may need additional support to continue attending the program once enrolled.
Our findings contribute evidence to guide perinatal service provision and ongoing monitoring decisions at the 5Ps CPNP. Further research is needed to explore new program delivery models as a means to enhance perinatal services for vulnerable women.
Acknowledgements
We thank all mothers who provided data to the Canada Prenatal Nutrition Program that we evaluated. We would also like to thank Dr. Jingxiong Xu for help with the imputations. This study was funded by The Sprott Foundation and the Joannah and Brian Lawson Centre for Child Nutrition. JF’s graduate stipend was supported by an Ontario Graduate Scholarship and Peterborough K. M. Hunter Charitable Foundation Graduate Award. The sources of funding had no role in the design or conduct of the research study, statistical analysis, data interpretation or writing of the manuscript.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Authors’ contributions and statement
JF, DWS and DLO conceptualized the study. JF, AM, DWS and DLO designed the study with input from SI, SS, BU, VT and EDR. JF and SI performed data collection and analysis. AK provided primary statistical guidance. All authors provided primary guidance on data interpretation. JF wrote the first draft of the manuscript and all authors read and approved the final manuscript.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.
