Addressing vaccine hesitancy in the context of COVID-19: A primer for health care providers
On this page
- Purpose of this primer
- The "need-to-know" about vaccine hesitancy
- Strategies for building vaccine confidence
- Recognizing and responding to vaccine hesitancy
- Additional reading and resources
Purpose of this primer
This primer is intended to support health care providers in better understanding and addressing COVID-19 vaccine hesitancy, in their practice and beyond.
COVID-19 vaccines are one of the many important tools that will help put an end to this pandemic in Canada and globally. However, the success of Canada's COVID-19 vaccination program hinges on Canadians' acceptance and uptake of these vaccines.
Health care providers play a critical role in shaping their patients' decisions around vaccination. Many Canadians have questions about COVID-19 vaccines and may be hesitant to get vaccinated when they have the opportunity. The information and advice that health care providers share with patients around the vaccines - and how they share it - can be a determining factor in patients' decision to get vaccinated against COVID-19.
The "need-to-know" about vaccine hesitancy
About vaccine hesitancy
The World Health Organization defines vaccine hesitancy as "the reluctance or refusal to vaccinate despite the availability of vaccines".
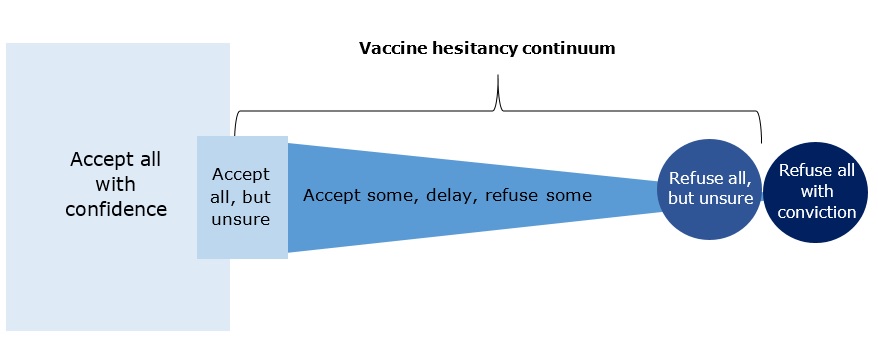
Adapted from MacDonald and the SAGE Working Group on Vaccine Hesitancy (2015).
Figure 1 - Text equivalent
This figure shows the continuum of vaccine acceptance. The continuum includes five groups, represented by five shapes along the continuum. The relative size of these shapes, and their order on the continuum, reflects each group's level of vaccine acceptance and their demand for vaccines. Within the vaccine acceptance continuum is a smaller continuum of vaccine hesitancy.
On the left hand of the continuum is the first group: those who accept all vaccines with confidence. This group is represented by a large square. The size of the shape represents this group's high acceptance of and demand for vaccines. This group is not within the vaccine hesitancy continuum.
Next to this group, represented in a smaller square, is the second group: those who accept all vaccines, but are unsure of or not fully confident with this decision. This group has less of a demand for vaccines compared to the first group, hence its smaller shape. This "accept all, but unsure" group is the first of three groups on the vaccine hesitancy continuum.
The third group represents those who accept some vaccines while refusing others and those that delay vaccination. This group is represented by a triangle on its side, its apex pointing right, representing a spectrum within this distinct group. This third group is also on the vaccine hesitancy continuum, and more hesitant than those in the "accept all, but unsure group".
Next to this group is the fourth group: those who refuse all vaccines, but are unsure of or not fully confident with this decision. This group is represented by a small circle near the far right of the continuum, representing their low acceptance of and demand for vaccines. This is the last of the three groups on the vaccine hesitancy continuum.
Finally the fifth group, furthest on the right of the continuum: those that refuse all vaccines with conviction. Their position on the furthest end of the continuum, and the small size of the circle used to represent them, reflects their low acceptance of and demand for vaccines. This fifth group does not appear on the vaccine hesitancy continuum given their conviction in their decision to refuse all vaccines.
Vaccine hesitancy exists on a continuum, shown in Figure 1, ranging from "accept all vaccines, despite being unsure" to "refuse all vaccines, despite being unsure". In between those two ends of the continuum exist those who accept some vaccines, delay vaccinations and/or refuse certain vaccines. Examples include individuals who refuse COVID-19 vaccines while being generally pro-vaccination and those who intend to wait a few months before getting vaccinated, despite being eligible to do so sooner.
This continuum demonstrates that vaccine hesitancy can take many forms. Individuals can also move across the continuum over time, as their vaccine-related knowledge, attitudes and behaviours change.
Impact of vaccine hesitancy on public health
Vaccination is the most effective way to protect against vaccine-preventable diseases. Over the past 50 years, vaccination has saved more lives in Canada than any other health intervention, making vaccination programs a significant public health success.
Vaccine hesitancy represents a key barrier to vaccination success. When vaccine uptake is low or decreases, it undermines the strength and public health impact of vaccination programs that exist to keep individuals and communities safe from vaccine-preventable diseases. As a result, communities in which vaccine uptake is low are at a greater risk of localized outbreaks of vaccine-preventable diseases.
In early 2019, prior to the COVID-19 pandemic, the World Health Organization listed vaccine hesitancy among the top ten threats to global health. The pandemic has since brought even more attention to the issue of vaccine hesitancy and reinforced the need to address this public health challenge.
How common is COVID-19 vaccine hesitancy
Most Canadians indicate that they intend to get vaccinated against COVID-19 when a vaccine is available to them.Footnote 1 Additionally, many studies indicate that public confidence in COVID-19 vaccines has increased since COVID-19 vaccines were first authorized, and vaccination of priority groups began in December 2020.Footnote 2
However, research from the initial months of COVID-19 vaccine availability in Canada shows that many Canadians express some level of hesitancy in the vaccines. Surveys conducted during this time by the Government of Canada and various polling firms suggest that while a small portion of Canadians do not intend to get a COVID-19 vaccine, others intend to either wait before getting vaccinated or have not yet made up their minds about vaccination.
Certain sub-groups in Canada are more likely to report COVID-19 vaccine hesitancy. These include Black Canadians, Indigenous peoples, newcomers, and younger adults, among others. Some of these sub-groups are also more likely to experience other social and structural barriers to accessing vaccinations.
While it can be helpful to understand how vaccine attitudes and intentions vary across different groups, it is important to remember that every person is different. Individuals are shaped by their various identities, experiences and unique contexts, all of which can influence their confidence in vaccines.
Vaccine hesitancy is not restricted to the general population; some health care providers report apprehension about COVID-19 vaccines. A survey of health care providers conducted by the Public Health Agency of Canada in December 2020 identified that 15% of respondents indicated that they would not get a COVID-19 vaccine when one became available or were unsure.
Taken together, these findings suggest that while most Canadians are confident in and accepting of COVID-19 vaccines, COVID-19 vaccine hesitancy - among health care providers and the general public alike - remains prevalent. It is with patients/clients who are taking a "wait and see" approach to COVID-19 vaccination, or are undecided about vaccination, where health care providers' advice and encouragement can make the largest positive impact on vaccine uptake.
Why some people are vaccine hesitant
The reasons for vaccine hesitancy are varied and complex. The following '5C' model summarizes the key factors that can influence vaccine hesitancy:
Confidence: level of trust in the effectiveness and safety of vaccines, the systems that delivers vaccines and the motives of those who establish vaccine policies.
Complacency: perception that risks of vaccine-preventable disease are low and vaccines are not necessary.
Convenience: extent to which vaccines are available, affordable, accessible, and individuals' ability to understand (as a reflection of language and health literacy) the need for vaccinations.
Calculation: individual engagement in extensive information searching and evaluation of risks of infections vs. vaccination.
Collective responsibility: extent to which one is willing to protect others by one's own vaccination.
These 5Cs can play out at individual and community levels and reflect historical, cultural and contextual factors. For example, COVID-19 vaccine hesitancy among Indigenous peoples and Black Canadians must be considered in the context of the history and ongoing experiences of colonialism, racism and discrimination against these communities, including within government, public health and health care institutions. Colonial structures have directly contributed to Indigenous Peoples having reduced access to adequate health care, healthy food and clean water, while also experiencing much greater levels of overcrowded housing, homelessness and incarceration. These factors have made them more vulnerable to illness, including COVID-19.Footnote 3 Moreover, trust in medical institutions has been eroded by a history of medical experimentation on these population groups, as well as the use of racially segregated medical facilities during the postwar years.Footnote 4 Experiences of racism and discrimination can erode individuals and communities' trust in these institutions, which in turn can erode trust in vaccines.
Vaccine hesitancy is neither new nor unique to COVID-19 vaccines. However, certain aspects of the COVID-19 context have prompted some people to have concerns about COVID-19 vaccines, including those who are typically pro-vaccine. These factors include the widespread availability and sharing of mis/disinformation about COVID-19 and COVID-19 response measures (including COVID-19 vaccines in particular), the rapid timelines in which vaccines were developed, and the new vaccine technologies used in certain COVID-19 vaccines. These factors are explored in the 'Recognizing and responding to vaccine hesitancy' section.
Strategies for building vaccine confidence
This section outlines practical, evidence-informed strategies that health care providers can use to address vaccine hesitancy within their practices. They include communication techniques for interactions with patients who may be vaccine hesitant (Table 1), as well as concrete actions that health care providers can take to foster a supportive vaccine work environment for staff, patients and visitors alike (Table 2).
| Strategy | Rationale |
|---|---|
| Use presumptive statements when initiating a discussion with patients about vaccines that convey the social norm of vaccination and the expectation that patients will vaccinate. Examples include "We'll give you your COVID-19 vaccine today" or "I will set some time aside for your COVID-19 vaccination during your appointment next week". | Research shows that presumptive statements such as these are more effective at encouraging vaccination among hesitant patients than a more participatory approach (i.e., asking what someone would "like to do" about vaccines). |
| Cultivate a "safe space" for discussions about vaccination. This includes relatively simple, but important things like engaging in active listening and creating opportunities to learn about patients' questions, values and experiences related to vaccination. It also means sharing information about vaccines using accessible plain language, such as by using analogies to communicate how vaccines work and avoiding technical jargon, and communicating in a culturally safe manner, taking into account patients' cultural, linguistic, social, political and economic backgrounds. | Individuals' distinct values, worldviews, experiences and identities shape their feelings and decisions about vaccines. Being in tune with these factors in your patients can help to enhance their comfort, establish common ground and build trust. It will also enable you to connect vaccination with something your patient sees to be "right", values or holds close to them (e.g., the desire to be a good mother, to regain personal freedoms limited by the pandemic, to remain healthy). |
| Open up about your own experiences getting vaccinated, vaccinating other patients and/or how you have chosen or encourage vaccination for your loved ones (e.g., children, elderly parents). Make it memorable by using storytelling to share these experiences and perspectives. | As a trusted source of health information, your expressions of vaccine confidence can build vaccine confidence in your patients. Research shows that storytelling is a highly engaging method for speaking with patients about vaccines, and that even short personal anecdotes can help minimize vaccine concerns. Facts and figures are helpful, but stories are what stick and are shared. |
| Activate the "right" emotions. When discussing vaccines with patients, be intentional about tapping into positive emotions like hope, love, pride and the concern for others, rather than evoking shame, sadness or guilt. For example, you can affirm someone's decision and positive feelings about vaccination with a simple statement like "you're doing an important thing to help protect yourself during this pandemic" or "thanks for doing your part; vaccination is an important way of helping us stop this pandemic". | Connecting vaccination to positive emotions is an effective way of motivating people to get vaccinated. Conversely, activating negative emotions to encourage vaccination can backfire. Research shows that fear can disempower and immobilize us, while shame can prompt some people to "double down" on pre-existing beliefs and decisions, rather than consider new information or perspectives. |
| Avoid judgment and labels. Some patients may voice hesitation or concerns about vaccines (including fear of needles) in clinical contexts. In these instances, it is important not to express judgement, assign negative labels or belittle/express frustration at fears and anxieties. | For some people who are vaccine hesitant, vaccine beliefs and decisions are deeply personal and a core part of their identity. For these patients, perceived attacks on these beliefs and decisions can be felt as attacks on them as individuals. For the many children and adults with needle phobias, negative experiences in vaccination contexts (e.g., perceptions of being mocked or punished for fears) can further entrench phobias and increase reluctance to get vaccinated in the future. Refer to Immunize Canada's guidance on immunization pain management for clinicians, for more compassionate, effective ways of managing needle fear and anxiety. |
| Be transparent during a discussion on the risks and benefits of vaccination, and inform patients of the risks of not getting vaccinated. You can discuss what is currently known about the authorized COVID-19 vaccines, how the effects and safety of these authorized vaccines continue to be studied and monitored, as well as the mechanisms behind common side effects (e.g., by stating that transient side effects like fever, headache or chills reflect our immune systems working to build protection against the disease). Whenever possible, use positive framing to describe risk of adverse events, such as by highlighting the large proportion of people who do not have serious side effects vs. the relatively small number who do. On the other hand, be sure to manage expectations about the social and health benefits of vaccination. For example, be clear that COVID-19 vaccination is not a "free pass" to resume all social activities immediately and that public health measures like wearing masks and handwashing will remain essential while scientists continue to study the COVID-19 virus and vaccines and monitor how the pandemic evolves. | Transparency is a key part of building trust, particularly in the current era of widespread conspiracy theories and mis/disinformation about COVID-19 and vaccines. Discussing the risks and benefits using a positive frame is more likely to inspire vaccine confidence compared to sharing the same information with a negative frame. Preparing patients for the possibility of common but transient side effects like pain at the injection site is an important part of their informed consent. These discussions can be a timely, effective opportunity to describe the ways that vaccines engage the immune system and prepare the body to fight disease. This example shows the importance of going beyond simple communication of the facts on vaccines (e.g., listing side effects and stating unknowns around how long people are protected from the virus post-vaccination) to include insights on why these things are true. This type of deeper, "behind the scenes" look at the clinical and research evidence can go a long way in building patients' confidence in COVID-19 vaccines. |
| Strategy | Rationale |
|---|---|
Spearhead or take part in a "pledge" within your workplace in support of COVID-19 vaccination. A pledge is simply a commitment to a particular action or behaviour (in this case, to get vaccinated). When public, a pledge communicates your personal views and intentions to those around you, including colleagues and patients. Pledges can take various forms. Here are some simple ways you can carry out a COVID-19 vaccine pledge in your workplace:
|
Behavioural science research shows that pre-commitment, which is a central part of a pledge, increases a person's likelihood of taking action, especially when the commitment is made publicly. Furthermore, public pledges also convey the message that vaccination is a social norm and something to celebrate. Both the "pledgers" and those who witness pledges are more likely to get vaccinated themselves. |
| Facilitate and take part in training on COVID-19 vaccines to support your and your colleagues/staffs' vaccine-related knowledge and skills. Training can range from the fundamentals on how the vaccines work and vaccine safety to technical instruction on COVID-19 vaccine handling, storage and administration (depending on staffs' scope of practice). | Engaging, comprehensive training for health care providers on COVID-19 vaccines is essential, regardless of the extent to which providers administer or advise patients on vaccines in their practice. This is because health care providers can have the same questions and concerns about the vaccines as members of the general public. Training can create opportunities for these questions and concerns to be heard and addressed and can help to build vaccine confidence and support health care providers in being champions for the vaccines for their patients and within their communities. |
| Celebrate success by broadcasting the number of COVID-19 vaccinations administered in your workplace to staff and patients. You can do this through physical signage (e.g., a vaccine counter), on your organization's website, via social media or simply sharing the good news verbally with those you encounter while at work. | These actions send a positive, empowering message about COVID-19 vaccination and communicate that organizations and individual health care providers are proud of their role in making them happen. These messages help to normalize COVID-19 vaccination and can also create openings for informed discussions about vaccines. |
| Make vaccination as convenient as possible for staff. Those who manage or are responsible for staff in health care settings should do what they can to make it easy for staff to get vaccinated. This might include giving staff paid time off to get their vaccine during work hours, offering vaccination on-site and allowing multiple opportunities for staff to get vaccinated. | Studies of health care workers show that employment and financial barriers like having to take unpaid time off work for COVID-19 vaccination are associated with a lower intention to vaccinate. Convenience can help facilitate vaccine uptake. Making it easy for staff to get vaccinated also sends the message that taking this health measure is an important part of their job vs. an "add-on". |
Recognizing and responding to vaccine hesitancy
This section is intended to support health care providers, particularly those who administer vaccines, in addressing patients' vaccine-related questions and concerns with confidence. Doing so will help to increase patients' confidence in vaccination decisions. The section outlines examples of what hesitancy can "look" like in practice, organized by the '5Cs' of vaccine hesitancy (described in the '"need-to-know" about vaccine hesitancy section), as well as guidance on how health care providers can respond in ways that support vaccine confidence and uptake.
| Patient | Health care provider |
|---|---|
| Confidence | |
| "There is a lot that worries me about these vaccines. I feel like they were rushed, and we don't really know if they are actually safe. I'm really scared of getting COVID, especially given my lung condition and age, but don't really trust these vaccines." | "I appreciate you sharing this with me. The rapid development of the vaccines is definitely remarkable. As a health care provider, I was among the first to get vaccinated. I got my second shot last week here at the clinic and feel really good about that decision. I can say with confidence that Health Canada has very high standards for vaccine safety. Decisions to authorize vaccines for use in Canada are based on scientific and medical evidence showing that vaccines are safe and effective. Because of the pandemic, countries and scientists have been working very closely together with more funds from governments to make COVID-19 vaccines a top priority. This has made it possible to develop effective vaccines in record time without compromising safety. The safety and efficacy of the authorized COVID-19 vaccines was also evaluated in thousands of individuals who volunteered to receive the vaccine in clinical trials. Since the vaccines have been authorized for public use, millions of people around the world have been vaccinated against COVID-19 and now are much more protected from the disease because of it. I strongly recommend the vaccine for you, especially given your lung condition and, conveniently, you can get the vaccine while you're here today." |
| Complacency | |
| "I'm not really worried about getting sick. Because I'm young, my risk of dying from COVID-19, if I ever got it, is super low. I don't think there is much benefit in me getting a vaccine." | "You're right that people your age are more likely to have fairly mild symptoms when diagnosed with COVID-19. However, unfortunately, that's not always the case. And while death rates are one way of looking at the impact of COVID-19 on different age groups, I can tell you that some people, including people your age, have long-term complications after getting the disease. I would never want that for you or any of my patients. That's why I'd recommend you get the vaccine when it becomes available to you. Even for people your age, the benefits of vaccination far outweigh the potential risks of getting COVID-19." |
| "I do a lot of things to protect myself. I eat well, wash my hands, exercise regularly and all that good stuff. I am generally a healthy person. I don't really think I need to get vaccinated." | "It's great to hear you're doing those things to keep healthy. Definitely keep it up. I like to think of vaccines as a personal trainer for your immune system, something to make it even stronger and more effective than it is right now. If you're ever exposed to the COVID-19 virus, being vaccinated will allow your immune system to fight the virus faster and more efficiently so that you're less likely to get sick. This is why I recommend vaccines for nearly all of my patients, including the healthy ones like you. We can all benefit from a personal trainer for our immune systems." |
| Convenience | |
| "I've heard that for some of these vaccines, you need to go back to get a second dose a specific amount of time later. I don't drive, so I have to take the bus everywhere, and I work really irregular shifts. It just seems like it might be tricky for me to get the vaccine. Maybe I shouldn't even bother...." | "You're right about the two doses for some vaccines and that there's a recommended waiting period in between. That said, there is a bit of wiggle room there to accommodate your schedule. If it's helpful, we can book your first and second dose visits today so it's all set and in your calendar. One thing off your plate. I can walk you through the hours when we're offering the vaccines so you can compare that with your work schedule, and we can find at time that suits you best. I know your job is really important to you. Getting vaccinated will help keep you protected and healthy to continue working and will also make it safer for you when you're on the bus. It's a good investment in yourself." |
| Calculation | |
| "I've done a lot of reading online about COVID-19 and the vaccines. From what I've read, if the virus exists at all, it's really no worse than the flu. I think the whole thing is overblown and an attempt at trying to scare and control people. The government isn't going to force me to get one of those vaccines…" | "Thanks for sharing this with me. I wish it were true that the COVID-19 virus isn't real or is harmless, but unfortunately, that's just not the case. In this clinic alone, I've seen dozens of patients that have been diagnosed with COVID-19, many of whom had severe cases. Since the start of the pandemic, people have compared the flu and COVID-19. Here's what we know for sure: COVID-19 seems to spread more easily than flu and causes more serious illnesses in some people. Unlike the flu virus, the virus that causes COVID-19 is new. Because of this newness, before the pandemic began, none of us had ever been exposed to the virus or had a chance to build immunity to protect us from it. This left all of us at risk of getting COVID-19. On the other hand, because of previous infections and our strong flu vaccination programs, a large proportion of Canadians have some immunity to influenza, which helps limit the number of flu cases we see each year. This is a part of why vaccines are so key for limiting the spread and number of deaths caused by COVID-19. The government is not going to force anyone to get the vaccine. That said, as your health care provider, I absolutely recommend you get the vaccine when you can, for yourself and for your loved ones." |
| Collective responsibility | |
| "I know that with 'herd immunity', it's not necessary for everyone to get vaccinated. Since most people are eventually going to get vaccinated, I should be safe, even if I don't get a vaccine myself." | "Think of getting vaccinated a bit like taking precautions around food storage while on camping trips. If everyone at the campground does their part and properly stores their food, nearby bears won't come sniffing around looking for their next snack. If you decide to leave your food out after dinner, you might be okay, since everyone else has been careful, but you've definitely increased the chances of inviting a bear into your campsite. This isn't good for other campers, and it definitely isn't good for you. Choosing not to get vaccinated is very much the same, especially while we're still waiting to learn how much the COVID-19 vaccines can reduce the spread of COVID-19. It's key for each of us to get vaccinated so we can at least ensure our own safety and hopefully decrease the spread of the virus in our communities." |
Additional reading and resources
- Canadian Pediatric Society. (2021). Our best shot at beating COVID-19: Overcoming vaccine hesitancy in 2021. [online education module]. Available at: https://www.cps.ca/en/clinical/immunization-and-vaccines
- Centers for Disease Control and Prevention. COVID-19 Vaccination Communication Toolkit For Medical Centers, Pharmacies, and Clinicians. Retrieved from: https://www.cdc.gov/vaccines/covid-19/health-systems-communication-toolkit.html
- Center for Public Interest Communications and the University of Florida. (2020). A practitioner's guide to the principles of COVID-19 vaccine communications: Principles for building trust. Retrieved from: https://covid19vaccinescommunicationprinciples.org/
- Dubé E, Gagnon D, Vivion M. Optimizing communication material to address vaccine hesitancy. Can Commun Dis Rep 2020;46(2/3):48-52. Retrieved from: /content/canadasite/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2020-46/issue-2-3-february-6-2020/article-5-best-practices-addressing-vaccine-hesitancy.html
- Gagneur A. Motivational interviewing: A powerful tool to address vaccine hesitancy. CanCommun Dis Rep 2020;46(4):93-7. Retrieved from: https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2020-46/issue-4-april-2-2020/article-6-canvax-addressing-vaccine-hesitancy.html
- BC Centre for Disease Control. (2021). Immunization communication tool. A resource for health care providers. Retrieved from: http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Immunization/Vaccine%20Safety/ICT-2021.pdf
- Lewandowsky, S., Cook, J., Schmid, P., Holford, D. L., Finn, A., Leask, J., Thomson, A., Lombardi, D., Al-Rawi, A. K., Amazeen, M. A., Anderson, E. C., Armaos, K. D., Betsch, C., Bruns, H. H. B., Ecker, U. K. H., Gavaruzzi, T., Hahn, U., Herzog, S., Juanchich, M., Kendeou, P., Newman, E. J., Pennycook, G., Rapp, D. N., Sah, S., Sinatra, G. M., Tapper, K., Vraga, E. K. (2021). The COVID-19 Vaccine Communication Handbook. A practical guide for improving vaccine communication and fighting misinformation. Retrieved from: https://hackmd.io/@scibehC19vax/home
- MacDonald, N. E., Desai, S., and Gerstein, B. (2018). Working with vaccine-hesitant parents: An update. Paediatrics and Child Health, 23(8), 561-561. Retrieved from: https://www.cps.ca/documents/position/working-with-vaccine-hesitant-parents
- Public Health Agency of Canada. (2016). Communicating effectively about immunization: Canadian Immunization Guide. Retrieved from: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-1-key-immunization-information/page-5-communicating-effectively-immunization.html