Haemophilus influenzae disease
Health Professionals
Haemophilus influenzae (Hi) is a bacterium which can cause serious invasive disease primarily in young children. Before the vaccine was developed in 1988, Hi serotype b (Hib) was the most common cause of bacterial meningitis in Canada. The National Advisory Committee on Immunization (NACI) recommends immunization against Hib disease.
Consult the national case definitions for additional information:
Agent of disease
Hi disease is caused by a gram-negative coccobacillus that is either encapsulated (typeable) or non-encapsulated (non-typeable). Encapsulated strains are divided into serotypes a through f, depending on the antigenic characteristics of their polysaccharide capsule. These strains are more likely to invade normally sterile sites, causing invasive disease, while non-encapsulated strains generally cause milder infections. Hib is the most pathogenic strain, which caused 95% of the disease before vaccine programs were introduced.
Reservoir
Humans.
Spectrum of clinical illness
Hi can cause a variety of infections, which range from mild to severe. Infections of the respiratory tract may result in pneumonia and bronchitis, and can lead to infections in the ear, sinuses and eyes.
About 55–65% of affected children developed meningitis. The remaining patients suffered from:
- epiglottitis,
- bacteremia,
- cellulitis,
- pneumonia, or
- septic arthritis.
Symptoms of meningitis usually develop 2 to 4 days after infection, and may include:
- sudden onset of fever,
- changes in mental status or behaviour,
- severe headache, or
- stiff neck and back.
In infants, the fontanelle may bulge.
Long-term Hib infection effects resulting in meningitis may include:
- permanent hearing loss,
- paralysis,
- seizures, and
- brain damage.
The case-fatality rate of Hib meningitis is about 5%. Severe neurologic sequelae occurred in 10–15% of survivors. Deafness occurred in 15–20% of survivors.
Transmission
Hi is transmitted by infected persons through the nasopharynx by contact with respiratory droplets, or nasal or throat discharges. Such contact includes:
- kissing,
- sharing drinks, or
- sharing contaminated objects (such as toys).
The incubation period is unknown, but is probably about 2 to 4 days. Infected persons can transmit disease for as long as Hi bacteria are still present, which may be for a prolonged period. Hi is non-communicable within 24 to 48 hours of starting effective antibiotics.
Disease distribution (global)
Hib infections occur worldwide, with a peak incidence in children less than 6 months old in developing countries. In industrialized countries, the peak age is between 6 and 12 months.
Before the widespread use of Hib vaccine, resource-poor countries were most at risk of illness and death from the disease. In the year 2000, the World Health Organization estimates that Hib was responsible for about 8.13 million cases of serious disease in children under 5, and for about 371,000 deaths. The number of countries using the vaccine more than doubled in 2008. As a result, the Hib mortality estimate dropped to 199,000 deaths in children under 5.
For more information on the global distribution of Hib, refer to the World Health Organization.
Risk factors
Globally, invasive Hib disease is most prevalent in children aged 2 months to 2 years. Those most at risk are children who:
- have splenic dysfunction (such as sickle cell disease or asplenia),
- have antibody deficiency,
- attend child-care centres,
- are from an Inuit community, or
- have a cochlear implant.
Hib vaccine is recommended for individuals 5 and older who are at increased risk for invasive Hib disease. Those at increased risk may have the following chronic conditions:
- congenital (primary) immunodeficiency,
- malignant hematologic disorders,
- HIV, or
- anatomic or functional asplenia (including sickle cell disease).
Other individuals at increased risk include all transplant and cochlear implant recipients.
Prevention and control
Hib infections can be prevented by routine immunization of all children, which NACI recommends at 2, 4 and 6 months old. A fourth dose should be administered between 12 and 23 months of age, and is generally given at 18 months. Hib vaccine is not generally recommended for healthy children after 59 months (5 years). Children 5 and older should receive a single dose of the vaccine if they are at increased risk of invasive Hib disease due to chronic conditions. The same applies to adults.
For further information about the Hib vaccine and its use, refer to the most recent version of the Canadian Immunization Guide and the NACI statements on Haemophilus influenzae type b.
Epidemiology of Haemophilus influenzae disease in Canada
Figure 1 demonstrates the decrease in annual incidence of reported invasive Hib disease in Canada since the introduction of Hib vaccines. Reported cases have decreased by 95% from an average of 1.76 cases per 100,000 population (range 0.92 to 2.98) in pre-vaccine era (1979–1988). The average in recent years (2006–2012) is 0.08 cases per 100,000 population (range 0.05 to 0.14).
Incidence of invasive Hib disease is age-dependent. Between 2006 and 2012, 38% of reported invasive Hib cases occurred among children younger than 5. Of these cases, 64% of children were younger than a year old. Most reported paediatric cases occurred in:
- unimmunized children,
- children too young to have received their primary series,
- children with an immunodeficiency illness, or
- children with other chronic illnesses.
Hi non-b invasive disease became nationally notifiable in 2007. However, not all provinces and territories report invasive Hi non-b disease to the Public Health Agency of Canada, which collects national data. Between 2009 and 2012, the limited national data on Hi non-b show an average incidence of 1.24 per 100,000 population (range 0.96 to 1.40) per year.
Figure 2 demonstrates that the incidence was highest in 2012 among infants younger than a year old (9.56 per 100 000 population). The next highest incidence is among children under 5 (3.15 per 100 000 population). This is followed by individuals aged 60 years and over (3.14 per 100 000 population).
Figure 1: Reported cases and incidence (per 100,000 population) of invasive disease of Haemophilus influenzae type b (Hib) in Canada by year, 1979 to 2012Figure 1 - Footnote *.
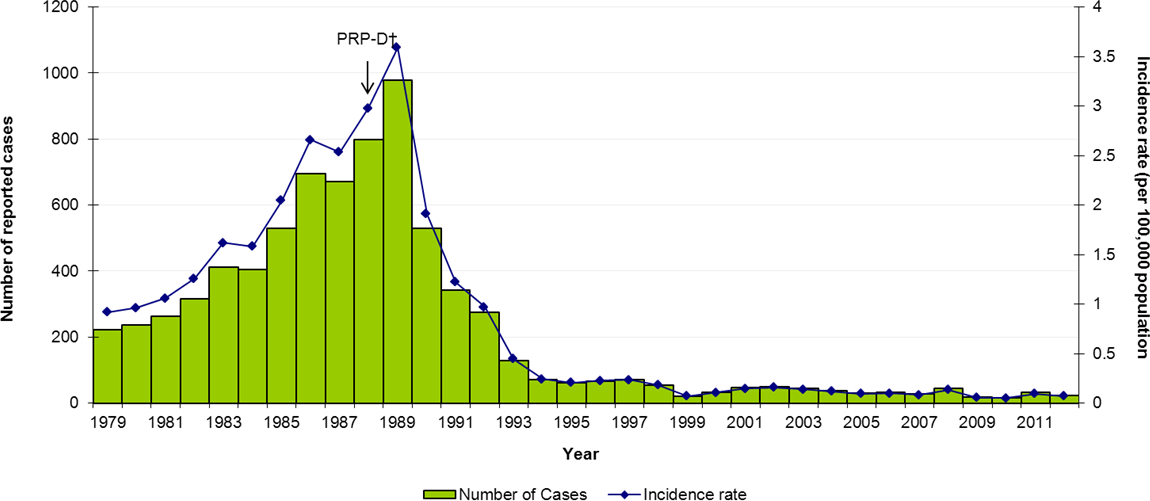
Text Equivalent - Figure 1
This image is a histogram showing the reported number of cases of Haemophilus influenzae type b (Hib) in Canada over time. A superimposed graph shows the incidence rates of Hib in Canada over time. The x axis represents the time between 1979 and 2012. The y axis on the left represents the reported number of cases starting from 0 at the bottom to 1200 at the top. The y axis on the right represents incidence rates per 100,000 population, starting with 0 at the bottom to 4 at the top. The bars represent the reported number of cases, and the line shows the Hib incidence rates. In 1979, the reported number of Hib meningitis cases was 220. The Hib meningitis cases steadily increased to 510 by 1985. The reported number of invasive Hib cases hit a peak of almost 900 by 1989. The PRP-D vaccine was introduced in 1988. The reported number of cases sharply declined to about 530 in 1990. Then it steadily declined to a low of about 30 in 1999. The number of cases remained stable around that level until 2012.
The incidence rate of Hib meningitis was close to 1 per 100,000 population in 1979, rising steadily to 2 per 100,000 population in 1985. All invasive disease caused by Hib reached an incidence rate of 2.7 by 1986. By the time the Hib conjugate vaccine PRP-D was introduced in 1988, the incidence rate was 3 per 100,000 population. The peak incidence rate of all invasive disease caused by Hib in Canada was about 3.7 in 1989. Since then, the incidence declined sharply and steadily over the years. The rate was about 1 in 1992, dropping below 0.5 per 100,000 population by 1993. The rate fell close to 0.1 in 1999. It stayed below 0.2 per 100,000 from 2000 to 2008, and below 0.1 per 100,000 from 2009 to 2012.
Figure 2: Reported cases and incidence (per 100,000 population) of invasive disease of Haemophilus influenzae (Hi) non-b type in Canada in 2012 by age groupFigure 2 - Footnote †.
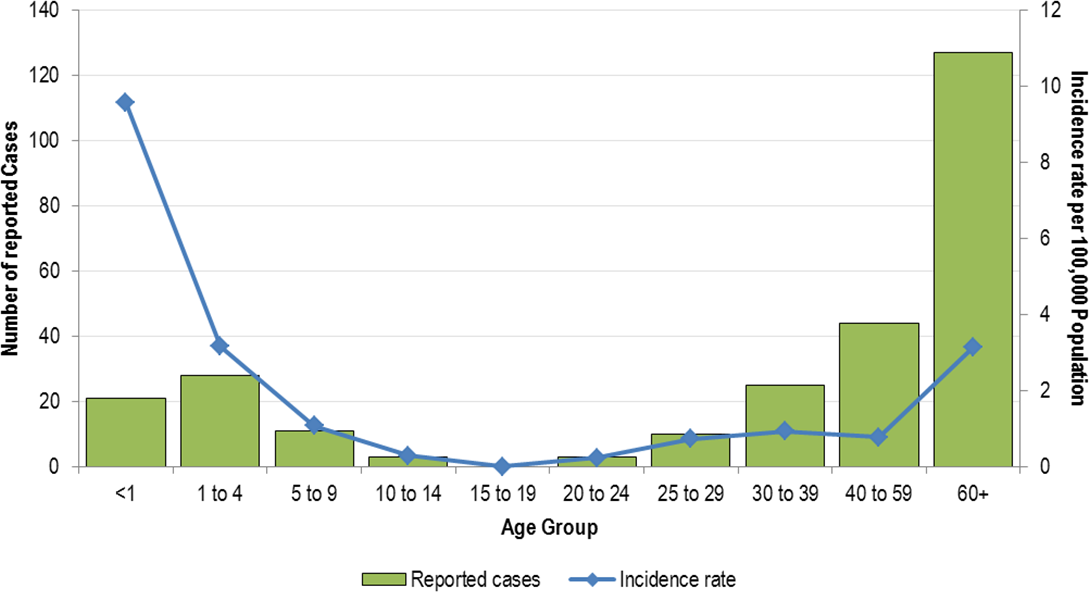
Text Equivalent - Figure 2
This image is a histogram showing the reported number of cases of Haemophilus influenzae (Hi) non-b type in Canada in 2012 by age group. A superimposed graph shows the incidence rates of Hinon-b type in Canada in 2012 by age group. The x axis represents the age group in years, including less than 1, 1-4, 5-9, 10-14, 15-19, 20-24, 25-29, 30-39, 40-49 and 60 and over. The y axis on the left represents the reported number of cases starting from 0 at the bottom to 140 at the top. The y axis on the right represents incidence rates per 100,000 population, starting with 0 at the bottom to 12 at the top. The bars represent the reported number of cases, and the line shows the incidence rates. In 2012, 127 cases were among individuals of age 60 and over, and 0 cases were reported among individuals of age 15 to 19. The incidence rate of 9.6 per 100,000 was highest among infants less than a year old. This is followed by a similarly high incidence among children under 5 of 3.15 per 100,000, and individuals of 60 years and up of 3.14 per 100,000. From age less than 1 to age 15-19, incidence rate decreased when age increased. From age 20-24 to age 60 and over, incidence rate increased when age increased.
Surveillance of Haemophilus influenzae disease in Canada
Health professionals play a critical role in identifying and reporting cases of invasive Hi disease in Canada. See the Surveillance section for more information.
Publications
- Vaccine Preventable Disease Reduction Targets by 2025 (Haemophilius influenzae type B)
- Vaccination Coverage Goals by 2025 (Haemophilius influenzae type B)
- Highlights from the 2019 childhood National Immunization Coverage Survey (cNICS)
- Vaccine Preventable Disease: Surveillance Report to December 31, 2019 (Invasive disease due to Haemophilus influenza serotype b section)
- Invasive bacterial diseases in northern Canada, 1999 to 2018
- Vaccine Preventable Disease: Surveillance Report to December 31, 2017 (Invasive disease due to Haemophilus influenza serotype b section) (archived)
- Vaccine Preventable Disease: Surveillance Report to December 31, 2015 (Invasive disease due to Haemophilus influenza serotype b section) (archived)
- A review of invasive Haemophilus influenzae disease in the Indigenous populations of North America
- The epidemiology of invasive disease due to Haemophilus influenzae serotype a in the Canadian North from 2000 to 2010
- Canadian National Report on Immunization, 2006 (Section 4.1 - Invasive Haemophilus influenzae type b (Hib) disease) (archived)
For more information:
- National case definition: Haemophilus influenzae serotype b, invasive disease
- National case definition: Haemophilus influenzae non-b, invasive disease
- Canadian Immunization Guide
- Provincial/Territorial Immunization Programs
- Canada Communicable Disease Report (CCDR)
- National Advisory Committee on Immunization (NACI)
- Travel Vaccines
- Vaccine Safety
- Additional Information for professionals on Immunization and Vaccines
- Canadian Notifiable Diseases Online