Archived - Syphilis 2010‑2015

 Download this article as a PDF
Download this article as a PDF Published by: The Public Health Agency of Canada
Issue: Volume 44-2: Sexually transmitted infections
Date published: February 1, 2018
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 44-2, February 1, 2018 Sexually transmitted infections
Surveillance
Infectious and congenital syphilis in Canada, 2010–2015
Y Choudhri1, J Miller1, J Sandhu1, A Leon1, J Aho1*
Affiliation
1 Centre for Communicable Diseases and Infection Control, Public Health Agency of Canada, Ottawa, ON
Correspondence
Suggested citation
Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Infectious and congenital syphilis in Canada, 2010-2015. Can Commun Dis Rep. 2018;44(2):43-8. https://doi.org/10.14745/ccdr.v44i02a02
Abstract
Background: Syphilis is the third most commonly reported notifiable sexually transmitted infection (STI) in Canada, following chlamydia and gonorrhea, respectively. Rates of this STI have been rising rapidly in Canada since 2001.
Objective: To summarize trends observed in syphilis rates for 2010 to 2015 in Canada.
Methods: Laboratory-confirmed cases of infectious syphilis and early congenital syphilis were reported to the Public Health Agency of Canada by all of the Canadian provinces and territories. National infectious syphilis rates were computed, as were rates per sex, age group and province/territory. Rates of congenital syphilis were also calculated.
Results: From 2010 to 2015, the rate of infectious syphilis in Canada increased by 85.6%, from 5.0 to 9.3 cases per 100,000 population. In 2015, a total of 3,321 cases of infectious syphilis were reported, mainly in males (93.7%), among whom the rate was 17.5 cases per 100,000 males versus 1.2 per 100,000 females. The rate also rose faster among males in 2010–2015, a 90.2% increase versus 27.8% among females. Individuals aged 20–39 years had the highest rates. Across the provinces and territories, the highest rates of infectious syphilis were in Nunavut, British Columbia and Manitoba.
The rate of congenital syphilis decreased from 2010 to 2014 (1.6 to 0.3 cases per 100,000 live births) before increasing to 1.5 cases per 100,000 live births in 2015, which corresponds to six reported cases.
Conclusion: Rates of syphilis continue to rise in Canada, especially among young men, and this is consistent with trends in the United States of America and European Union. Based on data from Canada and from these regions, the sexual behaviour of men who have sex with men (MSM) is thought to be a major risk factor for syphilis.
Introduction
Syphilis, caused by the bacterium Treponema pallidumFootnote 1 is the third most commonly reported notifiable sexually transmitted infection (STI) in Canada, after chlamydia and gonorrhea, respectively. If left untreated, a primary syphilis infection can progress through secondary, latent and tertiary disease stagesFootnote 2. Out of the four stages of syphilis, only three are infectious and therefore of public health significance: primary, secondary and early latent syphilisFootnote 1. Neurological symptoms can occur at any stage. Symptoms of infection in the earlier stages include chancres, condyloma lata and generalized lymphadenopathy. Cardiologic and musculoskeletal manifestations may occur if the infection remains untreated and reaches the tertiary stage. There is a synergy between HIV and syphilis as syphilis infection increases HIV viral load and HIV transmissionFootnote 2. Moreover, for exposed individuals, HIV acquisition is two- to five-fold higher among those infected with syphilis than those without syphilis infectionFootnote 2.
Congenital syphilis occurs through mother-to-child transmission, mainly in utero but also at birth. Congenital syphilis may have severe consequences for the newborn, such as cerebral palsy, hydrocephalus, sensorineural hearing loss, musculoskeletal deformity or deathFootnote 3. The risk of transmission varies from 10% to more than 70% depending on the mother's stage of diseaseFootnote 3. Transmission may be prevented with timely diagnosis and adequate treatment.
After years of low incidence among both males and females, there has recently been a large increase in the number of syphilis cases, mainly among malesFootnote 1. This rate increase coincides with the growing number of outbreaks reported in several cities and provinces across Canada among men who have sex with men (MSM), and especially among HIV-infected MSM, the heterosexual population and some Indigenous communitiesFootnote 1.
The objective of this article is to summarize observed trends in reported laboratory-confirmed infectious syphilis and congenital syphilis rates in Canada in the period 2010 to 2015. Rates were analyzed by sex, age and geographic distribution.
Methods
Data sources
Provincial and territorial health authorities provide non-nominal data on laboratory-confirmed cases to the Public Health Agency of Canada (PHAC) through the Canadian Notifiable Disease Surveillance System (CNDSS)Footnote 4. Confirmed case definitions of infectious syphilis and congenital syphilis are presented in the AppendixFootnote 5.
Variables submitted along with the diagnosis include sex, age at time of diagnosis, year of diagnosis and province/territory of diagnosis. All stages are notifiable but only infectious stages (primary, secondary and early latent) were included in this report. The received data were validated in collaboration with the corresponding province or territory. Data from January 1, 2010 to December 31, 2015 were available from all provinces and territories and were extracted from the CNDSS in July 2017.
Data analysis
Descriptive analysis was performed using Microsoft Excel. National annual reported case rates of infectious syphilis were computed per 100,000 population (or per males or females) for all years using number of cases from the CNDSS as numerators, and Statistics Canada yearly population estimates as denominators. Sex, age group and province/territory-specific rates were also calculated. For congenital syphilis, rates were computed per 100,000 live births. For 2014 and 2015, preliminary numbers of live births drawn from Statistics Canada were used, as final numbers were not yet available. No statistical procedures were used for comparative analyses. Small numbers are more susceptible to change and so corresponding rates should be interpreted with caution. Previous reports may provide different rates for some years due to reporting delays and data updating.
Results
From 2010 to 2015, the rate of reported laboratory-confirmed cases of infectious syphilis in Canada increased from 5.0 to 9.3 cases per 100,000 population (Figure 1). This represents an increase of 85.6% over this time period.
Sex and age
In 2015, a total of 3,321 cases of infectious syphilis were reported, of which 93.7% were males. This was reflected in the much higher rate of infectious syphilis among males than among females (17.5 cases per 100,000 males versus 1.2 cases per 100,000 females). The rate of infectious syphilis also increased faster among males than among females in 2010-2015 (90.2% among males versus 27.8% among females) (Figure 1).
Figure 1: OverallFigure 1 footnote a and sex-specific rates of reported laboratory-confirmed infectious syphilis cases, 2010–2015, Canada
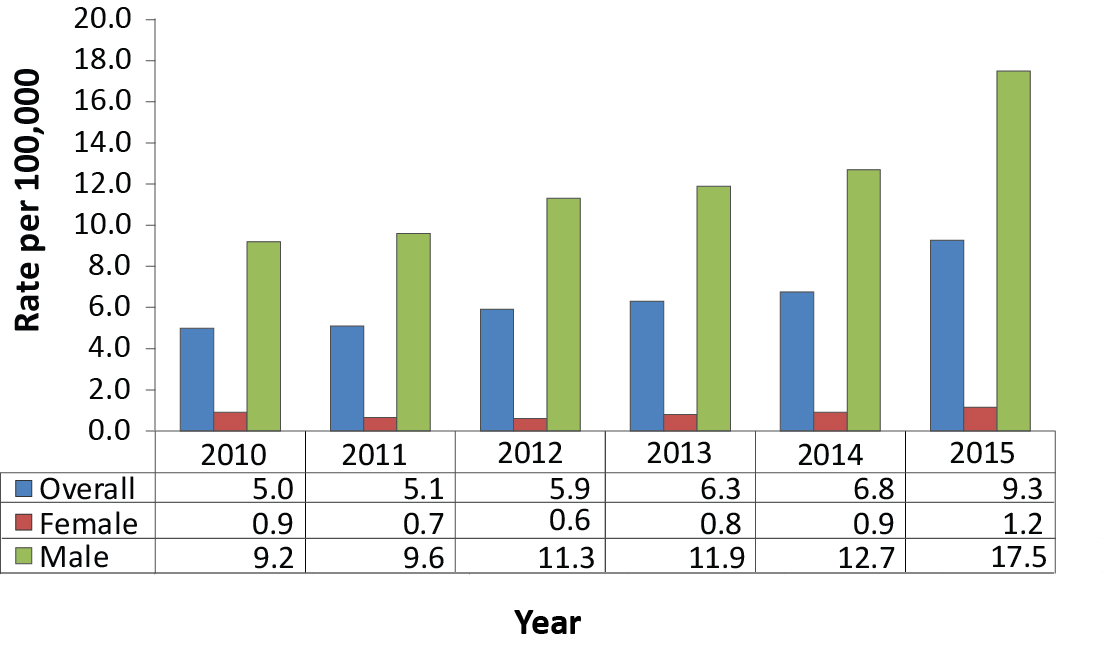
Text description: Figure 1
Figure 1: OverallFigure 1 footnote a and sex-specific rates of reported laboratory-confirmed infectious syphilis cases, 2010–2015, Canada
| Year | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|
| Overall | 5.0 | 5.1 | 5.9 | 6.3 | 6.8 | 9.3 |
| Female | 0.9 | 0.7 | 0.6 | 0.8 | 0.9 | 1.2 |
| Male | 9.2 | 9.6 | 11.3 | 11.9 | 12.7 | 17.5 |
Table 1 footnotes
|
||||||
From 2010 to 2015, all age cohorts had a rate increase (data not shown). The highest rates in 2015 (Figure 2) and highest rate increases from 2010 to 2015 were in those aged 25-29 years (a 133% increase from 2010 to 21.2 cases per 100,000 in 2015) and 30-39 years (a 109% increase from 2010 to 18.2 cases per 100,000 in 2015). For those two age groups, the increases were particularly pronounced between 2014 and 2015, accounting for more than half of the increase over 2010-2015. The increase in rate was also high during this period among those aged 60 years and above (a 91.7% increase, from 1.2 to 2.3 cases per 100,000). These three age cohorts (25-29, 30-39 and 60+) had the highest increase of all cohorts among both males and females.
Figure 2: Rates of reported laboratory-confirmed infectious syphilis by sex and age group, 2015, Canada
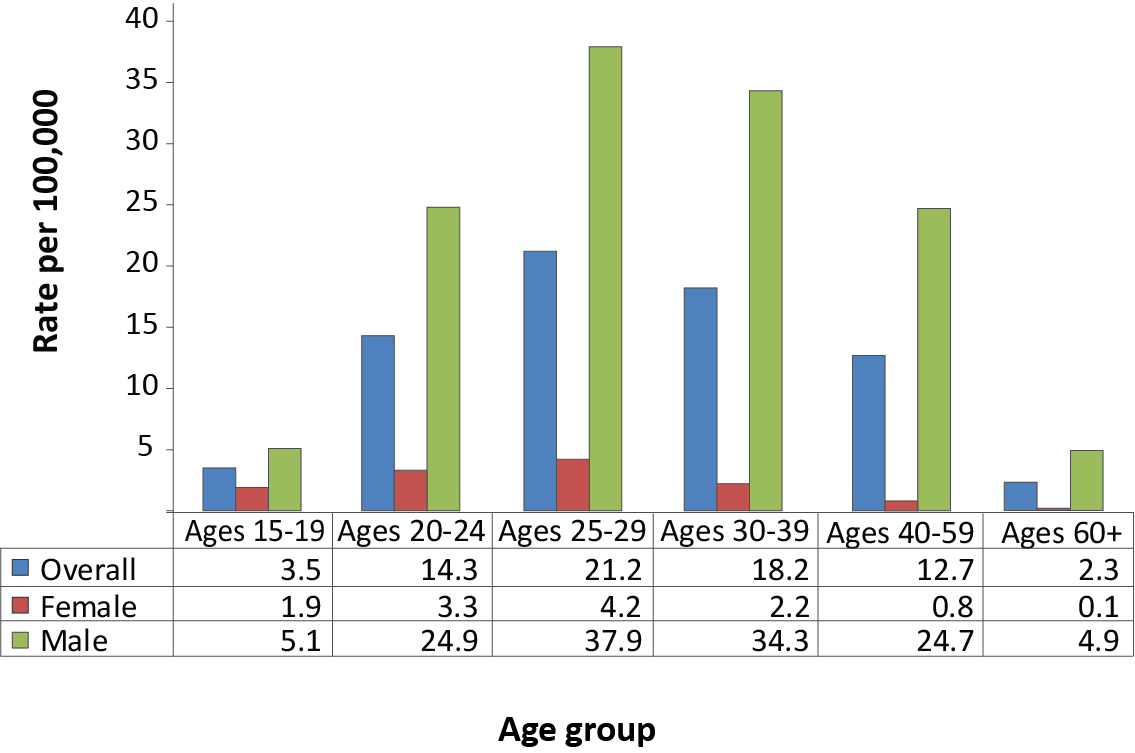
Text description: Figure 2
Figure 2: Rates of reported laboratory-confirmed infectious syphilis by sex and age group, 2015, Canada
| Age group | Ages 15-19 | Ages 20-24 | Ages 25-29 | Ages 30-39 | Ages 40-59 | Ages 60+ |
|---|---|---|---|---|---|---|
| Overall | 3.5 | 14.3 | 21.2 | 18.2 | 12.7 | 2.3 |
| Female | 1.9 | 3.3 | 4.2 | 2.2 | 0.8 | 0.1 |
| Male | 5.1 | 24.9 | 37.9 | 34.3 | 24.7 | 4.9 |
Geographic distribution
The three provinces with the highest reported rates of laboratory-confirmed syphilis in 2015 and the highest rate increases from 2010 to 2015 were Nunavut, British Columbia and Manitoba (Table 1). The greatest rate decreases were seen in the Northwest Territories, Saskatchewan and New Brunswick.
| Province or territory | Laboratory-confirmed cases by year of diagnosis (rate per 100,000) | |||||
|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| Alberta | 173 (4.6) |
94 (2.5) |
129 (3.3) |
124 (3.1) |
157 (3.8) |
369 (8.8) |
| British Columbia | 92 (2.1) |
128 (2.8) |
266 (5.9) |
454 (9.9) |
432 (9.3) |
607 (13.0) |
| Manitoba | 17 (1.4) |
16 (1.3) |
25 (2.0) |
59 (4.7) |
118 (9.2) |
205 (15.8) |
| New Brunswick | 34 (4.5) |
50 (6.6) |
21 (2.8) |
34 (4.5) |
27 (3.6) |
31 (4.1) |
| Newfoundland and Labrador | 4 (0.8) |
5 (1.0) |
9 (1.7) |
8 (1.5) |
24 (4.5) |
34 (6.4) |
| Northwest Territories | 3 (6.9) |
0 (0.0) |
2 (4.6) |
0 (0.0) |
0 (0.0) |
1 (2.3) |
| Nova Scotia | 18 (1.9) |
36 (3.8) |
63 (6.7) |
83 (8.8) |
64 (6.8) |
43 (4.6) |
| Nunavut | 0 (0.0) |
0 (0.0) |
29 (83.6) |
57 (161.0) |
82 (227.6) |
56 (153.3) |
| Ontario | 774 (5.9) |
770 (5.8) |
835 (6.2) |
744 (5.5) |
879 (6.4) |
1,052 (7.6) |
| Prince Edward Island | 0 (0.0) |
0 (0.0) |
0 (0.0) |
5 (3.4) |
9 (6.2) |
9 (6.1) |
| Quebec | 546 (6.9) |
630 (7.9) |
673 (8.3) |
631 (7.7) |
584 (7.1) |
737 (8.9) |
| Saskatchewan | 36 (3.4) |
23 (2.2) |
6 (0.6) |
17 (1.5) |
28 (2.5) |
24 (2.1) |
| Yukon | 0 (0.0) |
0 (0.0) |
1 (2.8) |
2 (5.5) |
0 (0.0) |
0 (0.0) |
| Canada | 1,697 (5.0) |
1,752 (5.1) |
2,059 (5.9) |
2,218 (6.3) |
2,404 (6.8) |
3,321 (9.3) |
Congenital syphilis
The number of laboratory-confirmed cases of congenital syphilis reported in Canada varied from one to six cases per year in 2010–2015 (Table 2).
| Indicator | Year of diagnosis | |||||
|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
| Number of cases | 6 | 5 | 3 | 2 | 1 | 6 |
| Rate per 100,000 live births | 1.59 | 1.32 | 0.79 | 0.53 | 0.26 | 1.54 |
Discussion
In Canada, the rates of reported cases of infectious syphilis markedly increased from 2010 to 2015. The burden of syphilis seems to be disproportionately placed on men. Other high-income countries such as the United States of America (USA), Australia and the United Kingdom have reported similar increases in numbers of cases and ratesFootnote 6Footnote 7Footnote 8.
The very high number of cases among males is thought to be mainly because of an increase in cases among MSMFootnote 1. Newfoundland and Labrador and Manitoba are among the provinces with the highest increases over 2010–2015. These provinces have reported that increased diagnoses among MSM was the main factor driving rates upwardsFootnote 9Footnote 10. This is of concern as syphilis contraction increases the probability of acquiring and transmitting HIVFootnote 1. A greater increase of reported syphilis cases has been observed among MSM living with HIV than among noninfected MSM in both Western Europe and the USAFootnote 11.
The causes of the increase in the rate of syphilis among MSM are multifactorial and complex. Changing community norms and behaviours as well as new preventive interventions such as pre-exposure prophylaxis (PrEP) might explain this rise. Many MSM have adopted behaviour patterns such as serosorting (choosing to have condomless sex with partners with the same HIV status) or having condomless oral sex, with the intention of decreasing HIV transmissionFootnote 12Footnote 13. However, the lowered condom use might increase the risk of contracting other STIsFootnote 13Footnote 14. In a Toronto-based study, condomless anal sex with casual partners in the previous six months was associated with syphilis infection among MSM living with HIVFootnote 15. Also of concern is the fact that Internet-based social media are increasingly being used to easily find sex partners. This may promote concurrent partnerships and rates of acquisition of new partners and decrease intervals between sex partnersFootnote 16. The social mixing patterns with the use of saunas, and the consumption of recreational drugs that may impair judgment in making decisions about sexual acts are also risk factors for acquisition and transmission of syphilis and other STIsFootnote 16Footnote 17. Lastly, increased risk-taking behaviours and a rise in STI incidence have been reported among HIV-negative MSM using PrEPFootnote 18Footnote 19Footnote 20. In Canada, PrEP was not significantly used in 2010–2015. However, data from other countries and from research studies highlight the importance of frequent STI screening of MSM on PrEP to ensure that symptomatic and asymptomatic STIs are treated in a timely way to halt transmission, as PrEP use increases over timeFootnote 21.
This finding highlights the importance of public health action to mitigate transmission of syphilis and identify new risk groups, such as MSM on PrEP.
The rate increase in women is also worrying as congenital syphilis tends to increase with rates of primary and secondary syphilis among women of childbearing age. A recent study on the epidemiology of syphilis in Winnipeg reported that one quarter of women with syphilis were pregnant at diagnosisFootnote 22. No cases of congenital syphilis were found in the study.
This finding highlights the importance of universal screening of pregnant women in a context of syphilis resurgence in Canada, as recommended by the Canadian Guidelines on Sexually Transmitted InfectionsFootnote 1.
Strengths and limitations
This surveillance report presents a national portrait of the current infectious syphilis epidemiology and was based on data from all provinces and territories. It describes sex, age and province/territory-specific rates over a six-year period.
Some limitations of the data should be noted. First, some numbers of cases of infectious and congenital syphilis were low. This leads to less stable rates, especially for congenital syphilis for which less than 10 cases were reported annually in Canada in 2010–2015. Therefore, variations in rates over time should be interpreted with caution. Second, these figures likely underestimate the incidence rate of syphilis from 2010 to 2015 as some infections may be asymptomatic, unscreened, undiagnosed or unreported. Screening, laboratory testing and reporting practices are heterogeneous across provinces and territories, and reports to the PHAC of syphilis cases by stage vary between provinces/territories. Therefore, we were not able to calculate valid stage-specific rates or to report on the number of cases of specific conditions such as neurosyphilis. Likewise, although age structures may vary across provinces and territories, we did not perform standardization by age. Therefore, direct comparison between provinces should be made with caution.
Trend analysis on the data was not performed, which is a limitation of this report. Lastly, risk factors and clinical presentation are not available in this surveillance system, preventing identifying risk factors associated with the observed increased rates.
Conclusion
In conclusion, syphilis rates in Canada have risen markedly over time. Males make up the vast majority of syphilis cases, and based on data from Canada, USA, Australia and other countries, MSM are one of the groups at highest risk. A better understanding of transmission dynamics and social and sexual networking is needed to guide prevention efforts.
Authors' statement
YC – Conceptualization, methodology, writing - original draft
JM – Software, data collection and curation, validation, formal analysis, visualization, writing – review and editing
JS – Writing – original draft, visualization
AL – Validation, formal analysis, visualization, writing – review and editing
JA – Conceptualization, writing – original draft
Conflict of interest
None.
Contributors
Chris Archibald: Supervision, writing – review and editing, resources, project administration
Jennifer Siushansian: writing – review and editing
Acknowledgements
It would not have been possible to publish this report without the continuous and greatly appreciated contribution of all provinces and territories.
Funding
This work was supported by the Public Health Agency of Canada.
Appendix: Case definitions of confirmed cases of infectious and congenital syphilisFootnote a
Laboratory confirmation of early congenital syphilis infection (within two years of birth):
- Identification of Treponema pallidum by dark-field microscopy, fluorescent antibody or equivalent examination of material from nasal discharges, skin lesions, placenta, umbilical cord or autopsy material of a neonate (up to four weeks of age)
OR - Reactive serology (non-treponemal and treponemal) from venous blood (not cord blood) in an infant/child with clinical, laboratory or radiographic evidence of congenital syphilis whose mother is without documented evidence of adequate treatment
OR - Detection of T. pallidum DNA in an appropriate clinical specimen
Laboratory confirmation of primary syphilis infection:
- Identification of T. pallidum by dark-field microscopy, fluorescent antibody, nucleic acid testing or equivalent examination of material from a chancre or a regional lymph node
OR - Presence of one or more typical lesions (chancres) and reactive treponemal serology, regardless of non-treponemal test reactivity, in individuals with no previous history of syphilis
OR - Presence of one or more typical lesions (chancres) and a fourfold or greater increase in the titre over the last known non-treponemal test in individuals with a past history of syphilis treatment
Laboratory evidence of infection for secondary syphilis:
- Identification of T. pallidum by dark-field microscopy, fluorescent antibody, nucleic acid testing or equivalent examination of mucocutaneous lesions, condylomata lata and reactive serology (non-treponemal and treponemal)
OR - Presence of typical signs or symptoms of secondary syphilis (e.g. mucocutaneous lesions, alopecia, loss of eyelashes and lateral third of eyebrows, iritis, generalized lymphadenopathy, fever, malaise or splenomegaly) AND either a reactive serology (non-treponemal and treponemal) OR a fourfold or greater increase in titre over the previous known non-treponemal test
Laboratory confirmation of early latent syphilis infection (<1 year after infection):
An asymptomatic patient with reactive serology (treponemal and/or non-treponemal) who, within the previous 12 months, had one of the following:
- nonreactive serology
- symptoms suggestive of primary or secondary syphilis
- exposure to a sexual partner with primary, secondary or early latent syphilis