Measles Annual Surveillance Report: 2019

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 47-3: Influenza and Other Respiratory Viruses
Date published: March 2021
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 47-3: Influenza and Other Respiratory Viruses
Surveillance
Measles surveillance in Canada, 2019
Cameron Coulby1, Francesca Reyes Domingo1, Joanne Hiebert2, Susan G Squires1
Affiliations
1 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
2 National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, MB
Correspondence
Suggested citation
Coulby C, Reyes Domingo F, Hiebert J, Squires SG. Measles surveillance in Canada, 2019. Can Commun Dis Rep 2021;47(3):149–60. https://doi.org/10.14745/ccdr.v47i03a05
Keywords: measles, travel health, surveillance, measles elimination, vaccination
Abstract
Background: The Public Health Agency of Canada (PHAC) has conducted enhanced measles surveillance since 1998, the year endemic measles transmission was eliminated in Canada. The objective of this annual national measles surveillance report is to provide an epidemiologic summary of measles activity reported in Canada for 2019 in order to provide evidence to support the continued verification of Canada’s measles elimination status.
Methods: Measles surveillance data are housed in the Canadian Measles and Rubella Surveillance System (CMRSS) database. Descriptive analyses of demographics and risk factors were performed. Outbreak characteristics were summarized and genotypic analyses conducted. Surveillance, laboratory and vaccine coverage data for 2019 were used to assess Canada’s status against the Pan American Health Organization (PAHO) essential criteria for the verification of measles elimination.
Results: In 2019, 113 measles cases were reported in Canada (crude incidence rate of 3.0 cases per 1,000,000 population). Of these cases, 42 (37%) were imported into Canada, and of the imported cases, 12 (29%) resulted in further transmission. Infants younger than one year had the highest age-specific incidence rate at 13.1 cases per 1,000,000 population. Only 29% of cases had one or more documented doses of measles-containing vaccine. One-fifth (19%) of cases were hospitalized; no deaths were reported. Genotype information was available for 100% of outbreaks reported in 2019 and 90% of non-outbreak-related measles cases; of cases with genotype information available, 27% were B3 and 73% were D8.
Conclusion: Despite meeting/partially meeting only three out of four of PAHO’s essential criteria for measles elimination status, there is no evidence that endemic measles transmission has been reestablished in Canada.
Introduction
Although vaccine preventable, measles is still a major cause of morbidity and mortality, especially in children younger than five yearsFootnote 1. In 2018, the last year for which estimates are available, there were approximately 9.8 million measles cases and 142,000 measles-related deaths worldwideFootnote 2. Global efforts to eliminate measles (which is defined as the absence of endemic measles transmission for at least 12 months in a defined geographic area with a well-performing surveillance system) began in 1963 with the introduction of the first measles vaccineFootnote 1Footnote 3.
In 1998, Canada was one of the first countries to eliminate endemic measles transmission following the pan-Canadian introduction of routine two-dose measles-mumps-rubella (MMR) vaccination for children in 1996–1997Footnote 3Footnote 4. However, Canada’s elimination status is threatened by infected travellers importing measles into Canada, particularly into pockets of the Canadian population that have suboptimal measles vaccination coverage ratesFootnote 3Footnote 4Footnote 5. As such, it is critical that Canada has a strong measles surveillance capacity, including laboratory capacity, to rapidly identify measles cases so that public health actions can be taken to reduce spread and prevent the reestablishment of endemic measlesFootnote 6.
The Public Health Agency of Canada (PHAC), including the National Microbiology Laboratory (NML), works with provinces and territories to conduct national measles surveillance. The Agency reports on measles activity weekly both publicly on the canada.ca website and to the Pan American Health Organization (PAHO)Footnote 7Footnote 8.
The objective of this annual national measles surveillance report is to provide an epidemiologic summary of measles activity reported in Canada for 2019 in order to provide evidence to support the continued verification of measles elimination status.
Methods
Surveillance data
The Canadian Measles and Rubella Surveillance System (CMRSS) is an active, enhanced surveillance system supported by all Canadian provinces and territories. Confirmed cases of measles meeting the national case definition were reported weekly to PHAC by provinces and territories and housed in the CMRSS databaseFootnote 7Footnote 8. All confirmed cases of measles with rash onset between January 1, 2019, and December 31, 2019, were included in this report. PHAC assigns epidemiologic weeks of rash onset with week one ending on the first Saturday of the year. A data validation process was conducted with all provinces and territories; this process included querying for missing data, identifying incorrect entries and confirming values with reporting jurisdictions. Cases with missing data were included in the analysis as appropriate. Visitors to Canada who were diagnosed with measles during their stay were included in this analysis.
A case was considered to have received a dose of measles-containing vaccine if the date of the vaccination is documented; otherwise, the case was considered unvaccinated. Cases with an unknown vaccination history were considered unvaccinated. A case was considered to be hospitalized if admitted to hospital due to measles or due to measles-related complications, but not if they were only seen in the emergency department.
The reporting province or territory identified the source of exposure in the course of the public health investigation. The sources of exposure were classified as outside Canada (imported); within Canada and linked to an imported case (import-related); within Canada and linked to a case of unknown origin; or unknown source/sporadic.
Verification of measles elimination through national and international goals and targets
PAHO set out four criteria for the ongoing verification of measles eliminationFootnote 9, (Table 1). The indicators, established by PAHO, of a well-performing surveillance system are based on investigation of measles-like illness (i.e. suspected cases), whereas only confirmed cases are nationally notifiable in Canada. As such, these data can only indirectly address the PAHO criteria.
| Criterion | Indicator |
|---|---|
| Verify the interruption of endemic measles cases for a period of at least 3 years from the last known endemic case, in the presence of high-quality surveillance | Zero cases of endemic transmission |
| Maintain high-quality surveillance sensitive enough to detect imported and import-related cases | >2 suspect cases per 100,000 population adequately investigated |
| Verify the absence of endemic measles virus strains through viral surveillance | Measles genotype assessed in 80% of outbreaks |
| Verify adequate immunization in the population | 95% of population cohorts aged 1–40 years have received a measles-containing vaccine |
Genotyping
NML routinely performs virus genotyping of all reverse transcription polymerase chain reaction (RT-PCR) confirmed cases for which viral specimens (respiratory swabs and/or urine) are available. The terminal 450 nucleotides of the measles nucleoprotein (N) gene (the N-450) were sequenced in accordance with World Health Organization (WHO) guidelinesFootnote 10Footnote 11 . Sequences were aligned with WHO genotype reference sequences and maximum parsimony phylogenetic trees generated in MEGA X softwareFootnote 12. Measles viral sequences were deposited in the WHO Measles Nucleotide Surveillance (MeaNS) database and distinct sequence identifiers (IDs) acquired. Sequences were also compared to designated named strains and to sequences deposited by other members of the global measles laboratory networkFootnote 11Footnote 13. All confirmed cases of measles with rash onset between January 1, 2019, and December 31, 2019, that had been genotyped were included in this report (n=73). The sequences were deposited in GenBank, the National Institutes of Health (NIH) genetic sequence database, with accession numbers MT386938 to MT387010.
Analysis
Descriptive epidemiologic analyses were performed based on the available variables in the CMRSS database, including age, sex, location, onset date, vaccination, hospitalization, source of exposure and genotypeFootnote 8. Statistical comparisons between frequencies were completed using Mid-P exact test, as appropriate. Measles outbreaks, defined as two or more confirmed cases linked epidemiologically, virologically or both, were described based on available informationFootnote 14. Incidence rates were calculated using Statistics Canada population estimates for July 1, 2019.
Results
A total of 113 confirmed measles cases (incidence rate of 3.0 cases per 1,000,000 population) were reported from seven provinces and one territory, in 2019 (Figure 1). Approximately one-third of these cases were related to one outbreak in the province of Québec. Of the 113 total confirmed cases, 73 (65%) were genotyped. The genotypes detected were B3 (n=20) and D8 (n=53), both of which circulated globally in 2019, based on data submitted to the WHO MeaNS databaseFootnote 15. Altogether, 102 cases were laboratory-confirmed and 11 cases were epidemiologically linked to a laboratory-confirmed case.
Figure 1: Number of reported measles cases (N=113), by epidemiologic week of rash onset and reporting province or territory, Canada, 2019
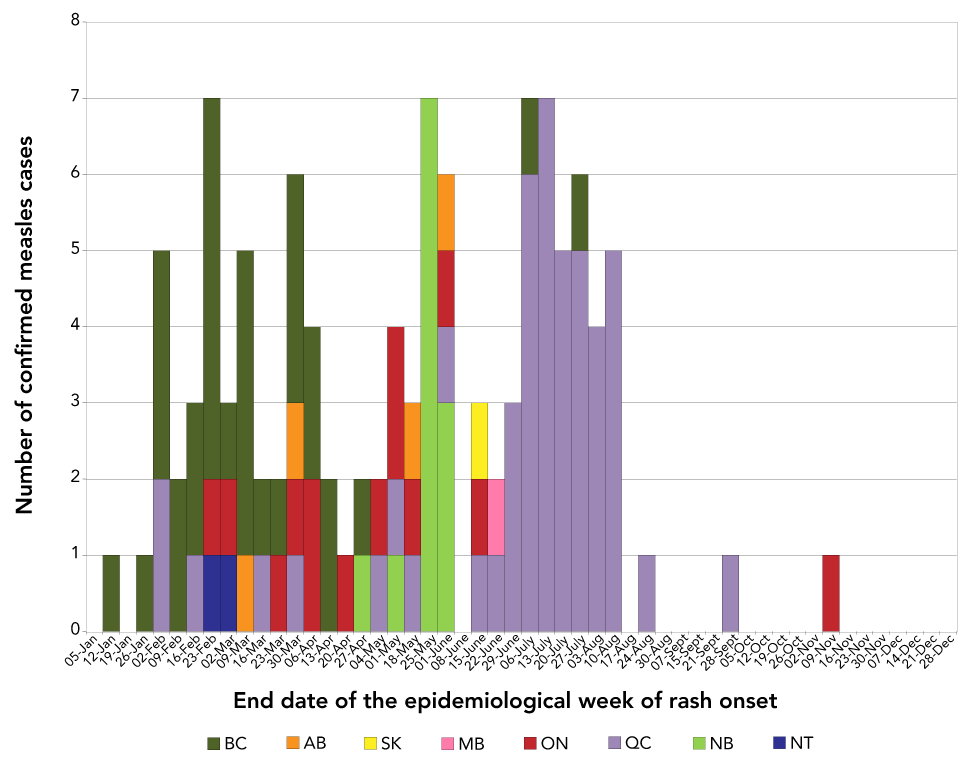
Text description: Figure 1
End date of the epidemiological week of rash onset |
Number of cases | |||||||
|---|---|---|---|---|---|---|---|---|
| Alberta | Manitoba | New Brunswick | British Columbia | Northern Territories | Ontario | Québec | Saskatchewan | |
| 05-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 12-Jan | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 19-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 26-Jan | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| 02-Feb | 0 | 0 | 0 | 3 | 0 | 0 | 2 | 0 |
| 09-Feb | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| 16-Feb | 0 | 0 | 0 | 2 | 0 | 0 | 1 | 0 |
| 23-Feb | 0 | 0 | 0 | 5 | 1 | 1 | 0 | 0 |
| 02-Mar | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 |
| 09-Mar | 1 | 0 | 0 | 4 | 0 | 0 | 0 | 0 |
| 16-Mar | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 |
| 23-Mar | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 |
| 30-Mar | 1 | 0 | 0 | 3 | 0 | 1 | 1 | 0 |
| 06-Apr | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 |
| 13-Apr | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 |
| 20-Apr | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| 27-Apr | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 04-May | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| 11-May | 0 | 0 | 1 | 0 | 0 | 2 | 1 | 0 |
| 18-May | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 |
| 25-May | 0 | 0 | 7 | 0 | 0 | 0 | 0 | 0 |
| 01-Jun | 1 | 0 | 3 | 0 | 0 | 1 | 1 | 0 |
| 08-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15-Jun | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| 22-Jun | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| 29-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 |
| 06-Jul | 0 | 0 | 0 | 1 | 0 | 0 | 6 | 0 |
| 13-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 7 | 0 |
| 20-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 |
| 27-Jul | 0 | 0 | 0 | 1 | 0 | 0 | 5 | 0 |
| 03-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 |
| 10-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 0 |
| 17-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 24-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 31-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 07-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 21-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 28-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 05-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 12-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 19-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 26-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 02-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 09-Nov | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| 16-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 23-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 30-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 07-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 21-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 28-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Information on age, sex and province or territory of residence was complete for all measles cases reported in 2019. The cases were aged from younger than one year to 73 years, with a median age of 15 years. Cases were most often in the 5–14 year age group (29%, n=33) or the 25–44 year age group (25%, n=28). The incidence rate of measles declined across age groups, with the highest incidence rate reported in infants younger than one year (13.1 cases per 1,000,000 population) and the lowest in adults 65 years and older (0.15 cases per 1,000,000 population; Figure 2). The majority of cases (65%, n=73) were male.
Figure 2: Confirmed measles cases (N=113) and incidence rates (per 1,000,000 population) by age group and vaccination status, Canada, 2019
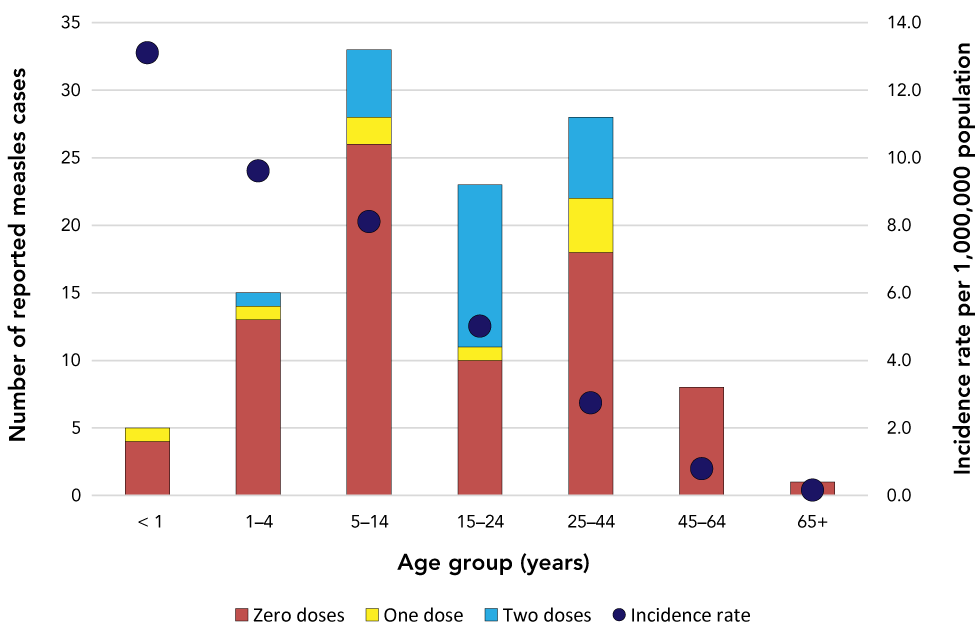
Text description: Figure 2
| Age group (years) | Number of reported measles cases by vaccination status | Incidence rate | ||
|---|---|---|---|---|
| Zero doses | One dose | Two doses | ||
| Younger than 1 | 4 | 1 | 0 | 13.1 |
| 1–4 | 13 | 1 | 1 | 9.6 |
| 5–14 | 26 | 2 | 5 | 8.1 |
| 15–24 | 10 | 1 | 12 | 5.0 |
| 25–44 | 18 | 4 | 6 | 2.7 |
| 45–64 | 8 | 0 | 0 | 0.8 |
| 65 and older | 1 | 0 | 0 | 0.2 |
Vaccination
Of the 113 measles cases reported in Canada in 2019, 71% (n=80) had no documented doses of measles-containing vaccine; of these, 16 cases had an unknown vaccination history. Over 40% of the unvaccinated measles cases (n=34) were related to an outbreak in a non-vaccinating community (see Outbreaks section, below). Of note, 57% (n=13) of cases in the 15–24 year age group had at least one documented dose of measles-containing vaccine; this is significantly higher than the proportion of cases with at least one dose of documented measles-containing vaccine in any other age group (p<0.01; Figure 2).
Hospitalization
All 113 measles cases reported had hospitalization information complete. In total, 19% of cases (n=21) were hospitalized, resulting in a hospitalization rate of 0.6 per 1,000,000 population. The mean age of hospitalized cases was 31 years (median: 34 years, range: 1–73 years). On average, hospitalized cases were significantly older than non-hospitalized cases (p<0.001). Of the 21 hospitalized cases, only three (14%) had any documented doses of measles vaccination.
Molecular epidemiology by source of exposure
Of the 113 confirmed cases of measles in 2019, 42 (37%) were imported into Canada after exposure to measles during travel (Table 2). Twelve of these imported cases transmitted measles within Canada, which resulted in an additional 60 import-related cases (Table 3). In total, imported and import-related cases accounted for 90% (n=102) of the total cases, while 10% (n=11) had an unknown or sporadic source of measles exposure (Table 2, Table 3).
| WHO region (number of cases) | Country | Number of cases | Genotype (number of cases) | WHO-named strain, if applicable, MeaNS Distinct Sequence ID (Number of cases) |
|---|---|---|---|---|
| Western Pacific (n=25) | Philippines | 11 | B3 (n=11) | MVi/Marikina City.PHL/10.18/, 5306 (n=4); N/A, 6018 (n=2); MVi/Gombak.MYS/40.15/, 4274 (n=1); N/A, 5654 (n=1); N/A, 5793 (n=1); N/A, 5904 (n=1); N/A, 6083 (n=1) |
| Viet Nam | 11 | D8 (n=6) | MVs/Gir Somnath.IND/42.16/, 4683 (n=3); N/A, 5840 (n=2); N/A, 5823 (n=1) | |
| Cambodia | 1 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| Multiple countries | 2 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| Europe (n=6) | France | 1 | B3 (n=1) | N/A, 5852 (n=1) |
| Poland | 1 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| Ukraine | 1 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| United Kingdom | 1 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| Multiple countries | 2 | D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |
| Americas (n=3) | United States of America | 3 | D8 (n=3) | MVs/Gir Somnath.IND/42.16/, 4683 (n=2); MVs/Dagon Seikkan.MMR/5.18, ID (n=1) |
| South-East Asian (n=3) | Bangladesh | 2 | B3 (n=2) | N/A, 5622 (n=1); N/A, 6218 (n=1) |
| India | 1 | D8 (n=1) | N/A, 5970 (n=1) | |
| Other (n=5) | Pakistan | 2 | B3 (n=1) | N/A, 5309 (n=1) |
| D8 (n=1) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1) | |||
| Multiple countries and regions | 3 | B3 (n=1) | MVi/Marikina City.PHL/10.18/, 5306 (n=1) | |
| D8 (n=2) | MVs/Gir Somnath.IND/42.16/, 4683 (n=1); N/A, 5601 (n=1) | |||
| Case number | Exposure category | End date of the epidemiologic week of rash onset | Genotype (WHO-named strain if applicable, MeaNS Distinct Sequence ID)Table 3 footnote a | Description |
|---|---|---|---|---|
| 1 | Unknown (exposed either in Canada or abroad) | February 16 | B3 (N/A, 5800) |
|
| 2 | Exposed in Canada, not linked to any case | February 23 | B3 (N/A, 5654) |
|
| 3 | Unknown (exposed either in Canada or abroad) | March 30 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 4 | Exposed in Canada, not linked to any case | March 30 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 5 | Exposed in Canada, not linked to any case | March 30 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 6 | Exposed in Canada, not linked to any case | April 6 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 7 | Exposed in Canada, not linked to any case | April 6 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 8 | Exposed in Canada, not linked to any case | June 1 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 9 | Exposed in Canada, linked to a sporadic case of unknown origin | June 15 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 10 | Exposed in Canada, not linked to any case | July 20 | Not determined |
|
| 11 | Exposed in Canada, not linked to any case | September 28 | B3 (N/A, 5230) |
|
Unknown source
Eleven cases (10%) were neither imported nor import-related: eight had no recent history of travel or known links to other confirmed measles cases (sporadic cases); one was linked to a sporadic case of unknown origin; and the exact source of exposure for the other two cases could not be determined (unknown source) because exposure may have occurred either in another country with known measles activity or in Canada (Table 3). These cases originated from British Columbia (n=5), Québec (n=4) and Ontario (n=2). Six of these cases were female and five were male. Ten of these 11 cases were genotyped; in seven cases, the genotype D8 MVs/Gir Somnath.IND/42.16/ named strain was detected, which was circulating globally in 2019. Three distinct genotype B3 strains (sequence IDs 5230, 5654 and 5800) were identified in the remaining three cases, two of which were not detected in any other measles case genotyped in 2019 (5230 and 5800) (Figure 3, Table 3).
Figure 3: Maximum parsimony phylogenetic tree of measles N-450 sequences identified in Canada in 2019 (n=73) prepared using MEGA X softwareFigure 1 footnote a
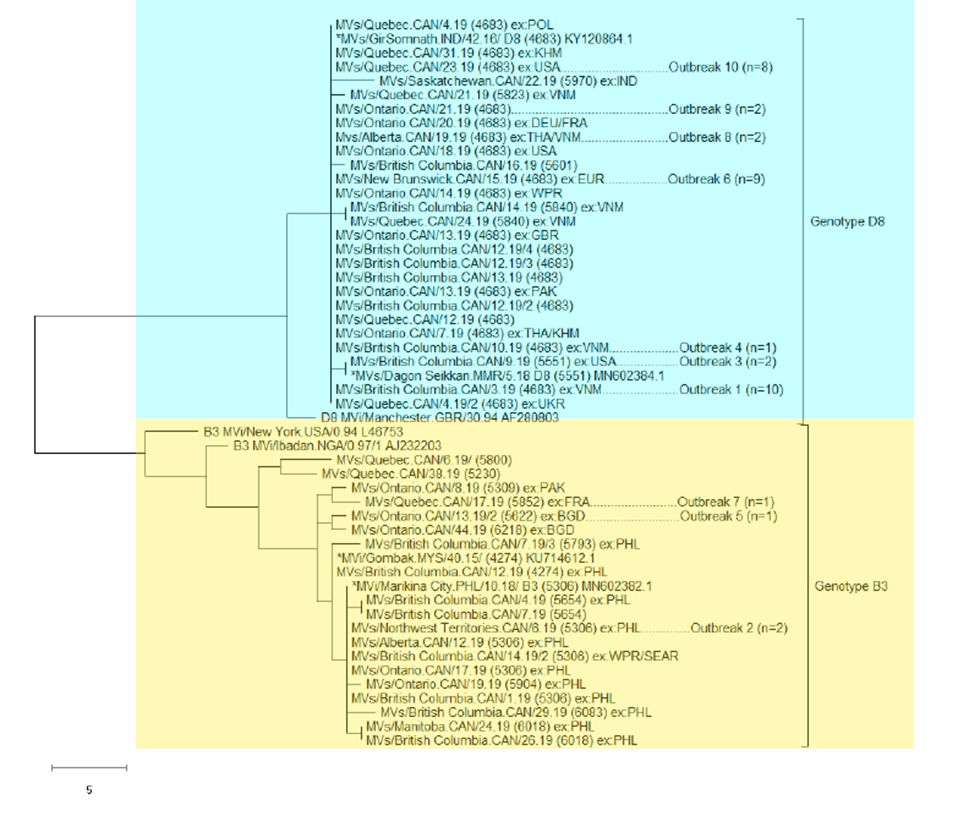
Text description: Figure 3
The phylogenetic tree of measles N-450 sequences detected in Canada in 2019 (n=73) is shown in figure 3 along with their outbreak status and source of importation, if applicable. Only genotypes B3 (n=20) and D8 (n=53) were detected in 2019 and those viral sequences are represented in the figure. The figure demonstrates that although most detected viruses were genotype D8, very little sequence diversity was seen, with most sequences identical to that of the MVs/Gir Somnath.IND/42.16 named strain (n=46) or highly similar with a maximum difference of four nucleotides. In total, including the MVs/Gir Somnath.IND/42.16 named strain, six distinct sequence identifiers (IDs) of genotype D8 were detected and included a second named strain: MVs/Dagon Seikkan.MMR/5.18. The cases with the MVs/Gir Somnath.IND/42.16 named strain identified (n=46) were associated with six of the seven genotype D8 outbreaks (n=32 sequenced cases) and 14 sporadic cases. These sporadic cases had travel history to Cambodia, Pakistan, Poland, Ukraine, United Kingdom, United State (US) or multiple countries (n=3 cases) while five cases had no history of travel. The sources for the six MVs/Gir Somnath.IND/42.16 named strain associated outbreaks were multiple countries (n=2), US, Viet Nam (n=2) or unknown. The remaining seven sequences that were not identical to the MVs/Gir Somnath.IND/42.16 named strain had travel history to India, the US and Viet Nam (n=3) or had no travel (two cases). Five of these cases were sporadic (one without travel) while the remaining two, identical to the MVs/Dagon Seikkan.MMR/5.18 named strain, were associated with a single outbreak.
The figure also shows that cases with genotype B3 sequences detected (n=20) had more sequence diversity with 13 distinct sequence IDs including two named strains: MVi/Gombak.MYS/40.15 and MVi/Marikina City.PHL/10.18. These two named strains are only one nucleotide different and, sequences identical or highly similar were the predominantly detected genotype B3 sequences detected (n=12 sporadic cases and two cases associated with one outbreak). Most of these cases had travel history either to the Philippines (n=11) or the Western Pacific / South-East Asian region (n=1). The figure shows that the remaining six cases with measles genotype B3 detected had distinct sequence IDs. Four cases had travel history: two to Bangladesh (one associated with an outbreak), one to France (associated with an outbreak) and one to Pakistan. The remaining two cases, also with distinct sequences, were sporadic cases without a history of travel.
Outbreaks
Ten measles outbreaks were identified for a total of 74 cases (Table 4). Seven of the 10 outbreaks were small (from 2 to 3 cases per outbreak), with limited transmission to household contacts or other close contacts of the index case. Three outbreaks were larger (from 12 to 34 cases per outbreak), with community-level transmission.
| Outbreak number | Province/territory | Number of cases (number of generations) | End date of the epidemiologic week of rash onset of index case | Genotype (WHO-named strain, if applicable, MeaNS Distinct Sequence ID)Table 4 footnote a | Description |
|---|---|---|---|---|---|
| 1 | British Columbia | 13 (n=5) | February 2 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 2 | Northwest Territories | 2 (n=2) | February 16 | B3 (MVi/Marikina City.PHL/10.18, 5306) |
|
| 3 | British Columbia | 2 (n=2) | March 9 | D8 (MVs/Dagon Seikkan.MMR/5.18, 5551) |
|
| 4 | British Columbia | 2 (n=2) | March 9 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 5 | Ontario | 2 (n=2) | March 23 | B3 (N/A, 5622) |
|
| 6 | New Brunswick | 12 (n=3) | April 27 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 7 | Québec | 3 (n=2) | May 4 | B3 (N/A, 5852) |
|
| 8 | Alberta | 2 (n=2) | May 18 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 9 | Ontario | 2 (n=2) | June 1 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
| 10 | Québec | 34 (unknown) | June 15 | D8 (MVs/Gir Somnath.IND/42.16, 4683) |
|
The WHO-named strain MVs/Gir Somnath.IND/42.16 was the most frequently detected in 2019. In total, 46 measles cases were identified with this strain (41% of all cases), and these cases were associated with six distinct outbreaks and 14 sporadic cases for a total of 20 chains of transmission. In the longest sustained outbreak associated with this strain, Outbreak 10, illness onset occurred during the week ending June 15 in the earliest case and during the week ending August 24 in the last case.
Verification of measles elimination through national and international goals and targets
The data in this report are provided as evidence in support of the ongoing verification of measles elimination in Canada, for which the PAHO has set out four essential criteriaFootnote 9. Based on the information available, Canada met or partially met three of the four criteria in 2019 (Table 5).
| Criterion | Description |
|---|---|
| Verify the interruption of endemic measles cases for a period of at least 3 years from the last known endemic case, in the presence of high-quality surveillance | Criterion met Canada achieved measles elimination status in 1998. Since then, molecular and epidemiologic data continue to demonstrate that no viral strain has circulated for a period of ≥1 year (Figure 4)Footnote 4Footnote 16Footnote 17Footnote 18Footnote 19 |
| Maintain high-quality surveillance sensitive enough to detect imported and import-related cases | Criterion partially met In Canada, national measles surveillance conducted through CMRSS consists of confirmed case surveillance and does not capture the number of clinical or suspect cases investigated, which are investigated at the provincial and territorial levels. However, based on data obtained by the Measles and Rubella Surveillance Pilot Project (which does not include all provinces and territories), the national rate of suspected case investigations has been previously estimated to be between 12 and 19 per 100,000 populationFootnote 17. Although the indicator cannot be met, the criterion has been met as the epidemiologic and laboratory evidence provided in this report indicates that Canada's measles surveillance capacity is sufficiently sensitive to detect imported and import-related cases and conduct case investigations |
| Verify the absence of endemic measles virus strains through viral surveillance | Criterion met Genotype information was available for 10/10 of outbreaks reported in 2019. Genotype information was also available for 90% of non-outbreak-related measles cases (35 genotyped of 39 cases) |
| Verify adequate immunization in the population | Criterion not met Canada currently measures (biennially) measles vaccination coverage rates at 2 and 7 years of age, and therefore is unable to assess measles vaccination coverage for all ages 1-40 years. The 2017 childhood National Immunization Coverage Survey estimated first dose measles-containing vaccine coverage in two year olds to be 90%, and two-dose measles-containing vaccine coverage in seven year olds to be 86%Footnote 5. |
Discussion
There were 113 confirmed cases of measles reported in Canada in 2019, the majority of which were imported or import-related (90%) and unvaccinated against measles (71%). This is higher than the median number of cases reported from 1998 to 2018 (median of 32 cases per year), and coincides with a trend of increasing rates of measles globally since 2017Footnote 2 Footnote 20Footnote 21Footnote 22. The United States (US) had the greatest number of measles cases since 1992 in 2019. Over 73% of cases in the US were linked to outbreaks in New York, and the majority of the cases in these outbreaks were not vaccinated against measlesFootnote 23. These US outbreaks had a direct impact on measles rates in Canada, with the largest Canadian outbreak of 2019 epidemiologically linked to a large outbreak in the US. Other large outbreaks in Canada were caused by unvaccinated travellers to Viet Nam and Europe, where outbreaks were also occurring in 2019. These outbreaks underscore the ongoing risk that any international travel places on the spread of measles in Canada, and validates PHAC’s 2019 broadening of its travel health notice for measles exposure risk to any international travel, and not only to certain areasFootnote 24.
Globally, only four of the 24 recognized measles genotypes continue to be detected, genotypes B3, D4, D8 and H1, as a result of elimination effortsFootnote 4, and only genotypes B3 and D8 were detected in confirmed measles cases in Canada in 2019. The genotype classification system captures viruses with similar yet distinct genetic (N-450) sequences, and for effective molecular epidemiology, additional granularity is required. The WHO global measles rubella laboratory network developed a system of “named strains” that are defined in the MeaNS database and represent a lineage, a precisely defined virus strain with a specific N-450 sequence, that has been frequently detected within a 2-year period in multiple countriesFootnote 11. In addition, the MeaNS database assigns a 4-digit identifier to all distinct or unique N-450 sequences within the database. All sequences obtained from cases of measles with the same N-450 sequence will share the same distinct sequence ID. In this way, all possible genetic sequences of reported measles cases can be tracked with their distinct sequence ID and some will also be designated as belonging to a named strain lineage, representing those with broader circulation. In 2019, 19 distinct sequence IDs, including four named strains, were identified in the 73 confirmed cases of measles that were genotyped.
The WHO-named strain MVs/Gir Somnath.IND/42.16 was the only strain detected in 2019 that was also detected in a handful of cases in 2018Footnote 16. This strain has been circulating globally since 2018, based on submissions to the MeaNS database, as reflected in the number of cases with travel history associated with this strain both in 2018 and 2019 (Figure 4). In 2018 to 2019, 51 measles cases were identified with this strain and these cases were associated with seven distinct outbreaks and 17 sporadic cases for a total of 24 chains of transmission. The time between illness onset in the first and last cases in the longest sustained outbreak associated with this strain was 70 days, which is far short of the 12 months of ongoing transmission that would signal endemic circulation. The detection of this strain in a large number of chains of transmission over an extended time demonstrates the value of integrating laboratory and epidemiologic data and necessitates the adoption of extended genotyping methods.
Figure 4: Number of measles cases with genotype D8, WHO-named strain MVs/Gir Somnath.IND/42.16 detected in 2018 and 2019 (n=51), by epidemiologic week of rash onset, chain of transmission status and source of exposure, CanadaFigure 4 footnote a
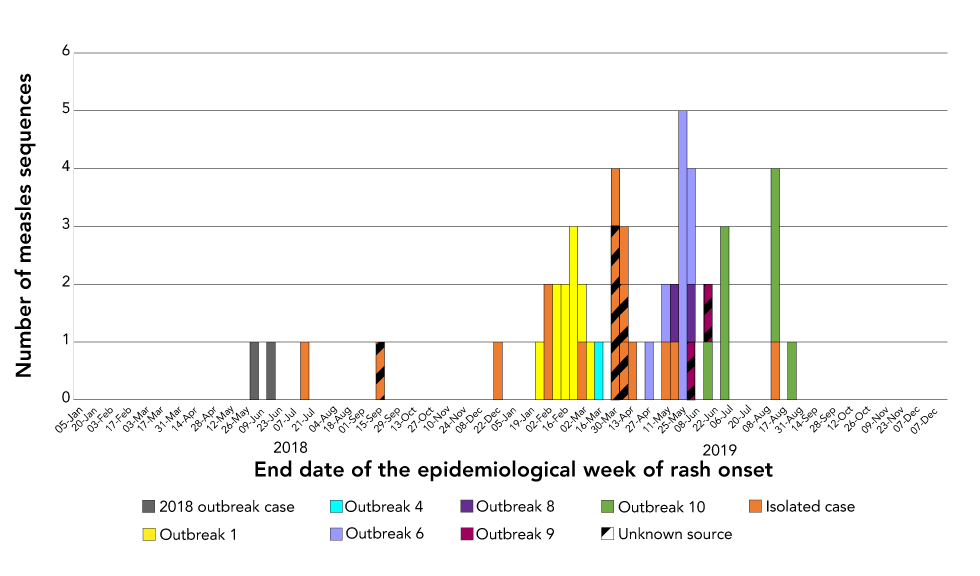
Text description: Figure 4
| End date of the epidemiological week of rash onset | Number of cases | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2018 outbreak case | Outbreak 1 | Outbreak 4 | Outbreak 6 | Outbreak 8 | Outbreak 9 (source unknown) | Outbreak 10 | Isolated case - imported | Isolated case - source unknown | ||
| 2018 | 06-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 13-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 20-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 27-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 03-Feb | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 10-Feb | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 17-Feb | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 24-Feb | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 03-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 10-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 17-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 24-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 31-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 07-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 14-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 21-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 28-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 05-May | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 12-May | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 19-May | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 26-May | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 02-Jun | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 09-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 16-Jun | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 23-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 30-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 07-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 14-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| 21-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 28-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 04-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 11-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 18-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 25-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 01-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 08-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 15-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| 22-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 29-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 06-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 13-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 20-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 27-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 03-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 10-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 17-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 24-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 01-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 08-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 15-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 22-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| 29-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 2019 | 05-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 12-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 19-Jan | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 26-Jan | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 02-Feb | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | |
| 09-Feb | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 16-Feb | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 23-Feb | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 02-Mar | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| 09-Mar | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 16-Mar | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 23-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 30-Mar | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | |
| 06-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | |
| 13-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| 20-Apr | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 27-Apr | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | |
| 04-May | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 11-May | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | |
| 18-May | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | |
| 25-May | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | |
| 01-Jun | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | |
| 08-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 15-Jun | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | |
| 22-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 29-Jun | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | |
| 06-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 13-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 20-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 27-Jul | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 03-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 10-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | |
| 17-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 24-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | |
| 31-Aug | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 07-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 15-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 21-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 28-Sep | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 05-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 12-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 19-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 26-Oct | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 02-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 09-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 16-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 23-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 30-Nov | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 07-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 14-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 21-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 28-Dec | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
Both in Canada and abroad, maintaining high vaccination coverage rate with measles-containing vaccine requires a sustained public health effort and is an essential component of a strategy for achieving and maintaining measles elimination. As in previous years, the large majority of measles cases were unvaccinated, highlighting the importance of adhering to vaccination guidelinesFootnote 16Footnote 17Footnote 25Footnote 26Footnote 27. Only one in five measles cases in 2019 had received two doses of measles vaccination, including five cases who were aged younger than one year and not yet eligible to receive the first routine dose of measles-containing vaccine under the routine vaccination scheduleFootnote 25.
The age distribution of measles cases reported in 2019 was similar to that seen in previous years, with younger age groups affected to a higher degree than older age groups Footnote 16 Footnote 17Footnote 18. Of note, over half of the measles cases in the 15–24 year age group had received two doses of measles-containing vaccine. The majority (n=7) of the fully vaccinated cases from this age group were related to a large outbreak in a secondary school in which many students were exposed. Given the large number of individuals exposed in this outbreak, some breakthrough cases, or cases that developed measles despite being fully vaccinated, would be expected even with high vaccine coverage. In addition, seroepidemiology conducted in the province of Ontario has found that this age group may have waning immunity to measlesFootnote 28. Breakthrough cases may have either failed to develop an appropriate immune response; their immunity may have waned to non-protective levels by time of exposure; or the vaccine they were given may have been stored, handled or administered improperlyFootnote 29Footnote 30.
Based on the information available, Canada met or partially met three of the four PAHO essential criteria for the verification of measles elimination in 2019. Canada falls short of the criterion regarding measles-containing vaccine coverage. Canada currently measures (biennially) measles vaccination coverage rates at 2 and 7 years of age, and therefore is unable to assess measles vaccination coverage for all ages between 1 and 40 years, as set out in the PAHO elimination framework. The 2017 estimate for two year olds receiving measles-containing vaccine is 90% and for seven year olds receiving the second dose of measles-containing vaccine is 86%, below the PAHO indicator of 95%Footnote 5. This estimate is derived from a survey that collected data from parent-held vaccination records, in which some information may be incomplete, erroneous or missing altogether. As vaccine doses with missing or invalid date are not counted in the calculation of coverage, the survey most likely underestimates coverage.
Strengths and limitations
This report has several limitations that bear consideration. Only measles cases that interact with the Canadian health system are captured in enhanced measles surveillance, and therefore cases with mild symptoms or visitors to Canada who do not seek health care may not be detected. Other federal or provincial surveillance systems may use case attribution methods that differ from CMRSS, which can cause discrepancies in annual case countsFootnote 31. Information on mortality and detailed information on morbidity (e.g. length of hospitalization, sequelae) are not currently captured by CMRSS, limiting the ability to completely describe the burden of illness due to measles. However, despite these limitations, this report serves to provide a detailed picture of measles in Canada in 2019 through an integrated analysis of both laboratory and epidemiologic case data for all reported cases.
Conclusion
The occurrence of measles cases and subsequent measles outbreaks in Canada in 2019, which were largely due to measles importations, underscore the importance of continued enhanced measles surveillance and efforts to increase vaccine uptake across the country. Although importation of measles and areas of low vaccination coverage continue to challenge Canada’s elimination status, the laboratory and epidemiologic evidence provided by this report indicates that endemic transmission of the measles virus has not been re-established in Canada.
Authors’ statement
- CC — Methodology, software, formal analysis, investigation, data curation, writing–original draft, writing–review and editing, visualization
- FRD — Conceptualization, methodology, formal analysis, writing–original draft, writing–review and editing, project administration
- JH — Methodology, validation, investigation, data curation, writing–original draft, writing–review and editing
- SS — Conceptualization, methodology, writing–review and editing, project administration
Competing interests
None.
Acknowledgements
The authors gratefully acknowledge the continued cooperation and efforts of provincial and territorial surveillance and laboratory partners in providing and validating data captured by Canadian Measles and Rubella Surveillance System (CMRSS) and referring specimens for molecular surveillance (genotyping) and for their review of the report content. The authors would like to thank Dr. C Dickson for her valuable contributions to the report.
Funding
This work was supported by the Public Health Agency of Canada.
References
- Footnote 1
-
World Health Organization (WHO). Measles. Geneva (CH): WHO; (accessed 2020-02). http://www.who.int/news-room/fact-sheets/detail/measles
- Footnote 2
-
Patel MK, Dumolard L, Nedelec Y, Sodha SV, Steulet C, Gacic-Dobo M, Kretsinger K, McFarland J, Rota PA, Goodson JL. Progress toward regional measles elimination— worldwide, 2000–2018. MMWR Morb Mortal Wkly Rep 2019;68(48):1105–11. https://doi.org/10.15585/mmwr.mm6848a1
- Footnote 3
-
King A, Varughese P, De Serres G, Tipples GA, Waters J; Working Group on Measles Elimination. Measles elimination in Canada. J Infect Dis 2004;189 Suppl 1:S236–42. https://doi.org/10.1086/378499
- Footnote 4
-
Public Health Agency of Canada. Elimination of measles rubella and congenital rubella syndrome in Canada: documentation and verification report: executive summary. Ottawa (ON): Government of Canada; 2013-04 (accessed 2020-02). https://www.canada.ca/en/public-health/services/immunization/vaccine-preventable-diseases/elimination-measles-rubella-congenital-rubella-syndrome-canada-documentation-verification-report.html
- Footnote 5
-
Public Health Agency of Canada. Vaccine coverage in Canadian children: results from the 2017 Childhood National Immunization Coverage Survey (cNICS). Ottawa (ON): Government of Canada; 2019 (accessed 2020-03). https://www.canada.ca/en/public-health/services/publications/healthy-living/2017-vaccine-uptake-canadian-children-survey.html
- Footnote 6
-
Public Health Agency of Canada. Vaccination Coverage Goals and Vaccine Preventable Disease Reduction Targets by 2025; Vaccine preventable disease reduction targets by 2025; Diseases under elimination: Maintain elimination status. Ottawa (ON): Government of Canada; 2020 (accessed 2020-01). https://www.canada.ca/en/public-health/services/immunization-vaccine-priorities/national-immunization-strategy/vaccination-coverage-goals-vaccine-preventable-diseases-reduction-targets-2025.html#2.1
- Footnote 7
-
Public Health Agency of Canada. Case definitions for diseases under national surveillance: results of provincial/territorial (P/T) consultation process. Can Commun Dis Rep 2009;35-Suppl 2:71–2. https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/ccdr-rmtc/09pdf/35s2-eng.pdf
- Footnote 8
-
Public Health Agency of Canada. Canadian measles/rubella surveillance system. Ottawa (ON): Government of Canada; (accessed 2020-02). https://www.canada.ca/en/public-health/services/surveillance.html#a5
- Footnote 9
-
Pan-American Health Organization. Plan of action. Documentation and verification of measles, rubella and congenital rubella syndrome elimination in the region of the Americas. Washington (DC): PAHO; 2010. https://www.paho.org/immunization/toolkit/resources/paho-publication/PoA-Documentation-Verification-MRCRS-Elimination-e.pdf
- Footnote 10
-
World Health Organization. Expanded Programme on Immunization (EPI). Standardization of the nomenclature for describing the genetic characteristics of wild-type measles viruses. Wkly Epidemiol Rec 1998;73(35):265–9. https://apps.who.int/iris/bitstream/handle/10665/230557/WER7335_265-269.PDF?sequence=1&isAllowed=y
- Footnote 11
-
World Health Organization. Genetic diversity of wild-type measles viruses and the global measles nucleotide surveillance database (MeaNS). Wkly Epidemiol Rec 2015;90(30):373–80. https://apps.who.int/iris/bitstream/handle/10665/242393/WER9030_373-380.PDF?sequence=1&isAllowed=y
- Footnote 12
-
Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: molecular Evolutionary Genetics Analysis across computing platforms. Mol Biol Evol 2018;35(6):1547–9. https://doi.org/10.1093/molbev/msy096
- Footnote 13
-
Rota PA, Brown K, Mankertz A, Santibanez S, Shulga S, Muller CP, Hübschen JM, Siqueira M, Beirnes J, Ahmed H, Triki H, Al-Busaidy S, Dosseh A, Byabamazima C, Smit S, Akoua-Koffi C, Bwogi J, Bukenya H, Wairagkar N, Ramamurty N, Incomserb P, Pattamadilok S, Jee Y, Lim W, Xu W, Komase K, Takeda M, Tran T, Castillo-Solorzano C, Chenoweth P, Brown D, Mulders MN, Bellini WJ, Featherstone D. Global distribution of measles genotypes and measles molecular epidemiology. J Infect Dis 2011;204 Suppl 1:S514–23. https://doi.org/10.1093/infdis/jir118
- Footnote 14
-
Measles and Rubella Elimination Working Group (MREWG), Public Health Agency of Canada. Guidelines for the prevention and control of measles outbreaks in Canada. An Advisory Committee Statement (ACS) Measles and Rubella Elimination Working Group (MREWG). Can Commun Dis Rep 2013;39(ACS-3):1–52. http://doi.org/10.14745/ccdr.v39i00a03
- Footnote 15
-
World Health Organization (WHO). Measles and rubella surveillance Data. Geneva (CH): WHO; (accessed 2020-02). https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/
- Footnote 16
-
Coulby C, Domingo FR, Hiebert J, MacDonald D. Measles surveillance in Canada: 2018. Can Commun Dis Rep 2020;46(4):77–83. https://doi.org/10.14745/ccdr.v46i04a04
- Footnote 17
-
Sherrard L, Hiebert J, Squires S. Measles surveillance in Canada: trends for 2014. Can Commun Dis Rep 2015;41(7):157–68. https://doi.org/10.14745/ccdr.v41i07a01
- Footnote 18
-
Public Health Agency of Canada. Measles surveillance in Canada: 2017. Ottawa (ON): Government of Canada; 2018 (accessed 2020-03). https://www.canada.ca/en/public-health/services/publications/diseases-conditions/measles-surveillance-canada-2017.html
- Footnote 19
-
Public Health Agency of Canada. Sustainability of Measles, Rubella and Congenital Rubella Syndrome (CRS) Elimination. Country template for the update of country reports (PAHO/WHO). Ottawa (ON): Government of Canada; 2016-04
- Footnote 20
-
World Health Organization. Feasibility assessment of measles and rubella eradication. Geneva (CH): WHO; 2019 (accessed 2020-03). https://www.who.int/immunization/sage/meetings/2019/october/3_Feasibility_Assessment_of_Measles_and_Rubella_Eradication_updatedSAGE.pdf
- Footnote 21
-
Dabbagh A, Laws RL, Steulet C, Dumolard L, Mulders MN, Kretsinger K, Alexander JP, Rota PA, Goodson JL. Progress toward regional measles elimination— worldwide, 2000–2017. MMWR Morb Mortal Wkly Rep 2018;67(47):1323–9. https://doi.org/10.15585/mmwr.mm6747a6
- Footnote 22
-
Public Health Agency of Canada. Vaccine preventable disease: surveillance report to December 31, 2017. Ottawa (ON): Government of Canada; 2020 (accessed 2020-10). https://www.canada.ca/en/public-health/services/publications/vaccines-immunization/vaccine-preventable-disease-surveillance-report-december-31-2017.html
- Footnote 23
-
United States Centre for Disease Control and Prevention. Measles (Rubeola): measles cases and outbreaks. Atlanta (GA): U.S. Department of Health & Human Services; 2019 (accessed 2020-02). https://www.cdc.gov/measles/cases-outbreaks.html
- Footnote 24
-
Public Health Agency of Canada. Global measles notice. Ottawa (ON): Government of Canada; 2019 (accessed 2020-05). https://travel.gc.ca/travelling/health-safety/travel-health-notices/203
- Footnote 25
-
Provincial and territorial routine and catch-up vaccination schedule for infants and children in Canada. Ottawa (ON): Government of Canada; 2018 (accessed 2020-01). https://www.canada.ca/en/public-health/services/provincial-territorial-immunization-information/provincial-territorial-routine-vaccination-programs-infants-children.html
- Footnote 26
-
Measles vaccine: Canadian immunization guide: Table 1: Criteria for measles immunity. Ottawa (ON): Government of Canada; 2018 (accessed 2020-01). https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-4-active-vaccines/page-12-measles-vaccine.html#p4c11t1
- Footnote 27
-
Immunization of travellers: Canadian immunization guide. Ottawa (ON): Government of Canada; 2017 (accessed 2020-02). https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-3-vaccination-specific-populations/page-9-immunization-travellers.html
- Footnote 28
-
Bolotin S, Severini A, Hatchette T, McLachlan E, Savage R, Hughes SL, Wang J, Deeks SL, Wilson S, Brisson M, Halperin SA, Gubbay J, Mazzulli T, Serhir B, Ward BJ, Crowcroft N. Assessment of population immunity to measles in Ontario, Canada: a Canadian Immunization Research Network (CIRN) study. Hum Vaccin Immunother 2019;15(12):2856–64. https://doi.org/10.1080/21645515.2019.1619402
- Footnote 29
-
Breakwell L, Moturi E, Helgenberger L, Gopalani SV, Hales C, Lam E, Sharapov U, Larzelere M, Johnson E, Masao C, Setik E, Barrow L, Dolan S, Chen TH, Patel M, Rota P, Hickman C, Bellini W, Seward J, Wallace G, Papania M. Measles outbreak associated with vaccine failure in adults – Federated States of Micronesia, February-August 2014. MMWR Morb Mortal Wkly Rep 2015;64(38):1088–92. https://doi.org/10.15585/mmwr.mm6438a7
- Footnote 30
-
Hinman AR, Orenstein WA, Mortimer EA Jr. When, where, and how do immunizations fail? Ann Epidemiol 1992;2(6):805–12. https://doi.org/10.1016/1047-2797(92)90074-Z
- Footnote 31
-
Public Health Agency of Canada. Case definitions for communicable diseases under national surveillance: results of provincial/territorial (P/T) consultation process. Can Commun Dis Rep 2009;35 S2:1–123. https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2009-35/definitions-communicable-diseases-national-surveillance.html
