Exposure and transmission in a rural Canadian community of COVID-19

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 48-10, October 2022: Equity, Diversity and Inclusion in Public Health
Date published: October 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-10, October 2022: Equity, Diversity and Inclusion in Public Health
Outbreak
Demographic patterns of exposure and transmission for a rural Canadian community outbreak of COVID-19, 2020
Kaitlin Patterson1, Mathieu Chalifoux2, Rita Gad2, Shannon Leblanc2, Paige Paulsen2, Louise Boudreau3, Theresa Mazerolle4, Mariane Pâquet2
Affiliations
1 Canadian Field Epidemiology Program, Public Health Agency of Canada, Ottawa, ON
2 New Brunswick Department of Health, Fredericton, NB
3 Vitalité Health Network, Bathurst, NB
4 Vitalité Health Network, Richibucto, NB
Correspondence
Suggested citation
Patterson KA, Chalifoux M, Gad RR, Leblanc S, Paulsen P, Pâquet M. Demographic patterns of exposure and transmission for a rural Canadian community outbreak of COVID-19, 2020. Can Commun Dis Rep 2022;48(10):465–72. https://doi.org/10.14745/ccdr.v48i10a06
Keywords: COVID-19, Canada, outbreak, emerging infectious diseases, household transmission, workplace transmission, gender, rural communities
Abstract
Background: A coronavirus disease 2019 (COVID-19) community outbreak was declared October 5–December 3, 2020, in the Restigouche region of New Brunswick, Canada. This article describes the epidemiological characteristics of the outbreak and assesses factors associated with its transmission in rural communities, informing public health measures and programming.
Methods: A provincial line list was developed from case and contact interviews. Descriptive epidemiological methods were used to characterize the outbreak. Incidence rates among contacts, and by gender for the regional population were estimated.
Results: There were 83 laboratory-confirmed cases of COVID-19 identified during the observation period. The case ages ranged from 10–89 years of age (median age group was 40–59 years of age) and 51.2% of the cases were male. Symptom onset dates ranged from September 27–October 27, 2020, with 83% of cases being symptomatic. A cluster of early cases at a social event led to multiple workplace outbreaks, though the majority of cases were linked to household transmission. Complex and overlapping social networks resulted in multiple exposure events and that obscured transmission pathways. The incidence rate among men was higher than women, men were significantly more likely to have transmission exposure at their workplace than women, and men were the most common index cases within a household. No transmission in school settings among children was documented despite multiple exposures.
Conclusion: This investigation highlighted the gendered nature and complexity of a COVID-19 outbreak in a rural Canadian community. Targeted action at workplaces and strategic messaging towards men are likely required to increase awareness and adherence to public health measures to reduce transmission in these settings.
Introduction
The Restigouche region is located in north-central part of New Brunswick and has a population of 30,955 residents over a land mass of 8,580 km2 Footnote 1. With a population density of 3.6 people per km2, and no urban centres with a population over 30,000 people, Restigouche is considered to be a rural region Footnote 1. Between January 1 and October 4, 2020, the Restigouche region reported only 98 cases and relatively low community transmission rates of coronavirus disease 2019 (COVID-19). Here we describe a community outbreak within the Restigouche region where multiple chains of transmission resulted in 83 cases of COVID-19 identified between October 5 and November 4, 2020. The outbreak was declared on October 9, 2020, following the identification of an initial cluster of seven cases following a social gathering.
There is a paucity of reporting on rural COVID-19 outbreaks with complex overlapping social networks in the published literature. Because many rural and remote areas have limited capacity to manage and treat COVID-19, essential services may be rapidly paralyzed as individuals are implicated in outbreaks as either cases or contacts. Therefore, evidence is needed to inform targeted public health measures and programming for outbreak prevention and management in these rural communities. The objectives of this outbreak analysis are to describe the outbreak, to assess factors that led to spread and transmission and to inform recommendations for public health measures and programming in rural communities.
Methods
Public health nurses from both of New Brunswick's health networks (Réseau de santé Vitalité and Horizon Health Network) led data collection through case investigations and contact tracing interviews. The New Brunswick Department of Health also requested the assistance of the Canadian Field Epidemiology Program to provide epidemiological support to the investigation team, and the investigation was completed collaboratively between these agencies.
Sources of data included detailed case and contact interviews, a provincial case and contact line, and documentation of public health measures implemented during the outbreak (e.g. web pages, press releases, internal government documents).
Outbreak cases were defined as those with a laboratory-confirmed case using polymerase chain reaction (PCR) tests with nucleic acid detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), were a resident and/or visitor to the Restigouche region, whose episode date occurred from September 27, 2020, to November 5, 2020 (inclusive), and their source of acquisition was not travel-associated. Each case was assigned an episode date for analysis using either the date of symptom onset, or for asymptomatic cases the date of their positive laboratory specimen collection. The outbreak was declared over on December 3, 2020 (28 days or two COVID-19 incubation periods) from the last confirmed case on November 4, 2020 Footnote 2.
Investigation methods included descriptive epidemiology (e.g. frequency tables, epidemiological curves) using the available data collection tools, and additional case interviews to inform the extent of the outbreak and development of the social network diagrams. To examine potential transmission settings, we defined cluster events/locations where three or more cases were epidemiologically linked.
When multiple exposure settings were identified, a setting of most likely transmission was assigned for each case (family/household, social interaction and/or workplace), from likeliest to least likely. To ascertain most likely exposure settings, we examined the infectious period of cases present at each setting based on symptom onset date (if symptomatic) or specimen collection date (if asymptomatic) and risk of exposure. Cases who were secondary cases within their household (as defined by symptom onset date or testing date) were categorized as household exposure.
All cases were interviewed to identify how the case may have been exposed (backwards contact tracing) and any contacts the case may have exposed (forward contact tracing). At the outset of the outbreak, there were no public health recommendations for people in the community to wear a mask and no vaccine was available. Individuals that had close contact (i.e. less than two meters away for 15 or more minutes) with cases during their infectious period were classified as contacts, as per recommendations outlined by the Canadian government at the time of this outbreak. We calculated the secondary attack rate among contacts by dividing the number of known contacts that subsequently became cases by the total number of identified contacts.
We calculated the regional incidence rates overall and by age and gender. Gender, as part of the case investigation form, was defined as the socially constructed roles, behaviours, expressions and identities of girls, women, boys, men and gender diverse people (options for this variable were male, female, another gender or unknown). For the overall incidence rate, we divided the total number of laboratory-confirmed cases by the number of Restigouche residents according to the 2016 census Footnote 1. Then we divided the number of laboratory-confirmed cases by age/gender by their respective resident populations according to the census.
Cross tabulations (chi-squared or Fisher's exact for categorical or binary variables) and t-tests (for continuous variables) were used to examine differences in severity outcomes, number of contacts, exposures and testing delays by age and gender. Descriptive statistics were conducted using STATA, the charts were produced using excel and the social network diagram was produced in R.
Results
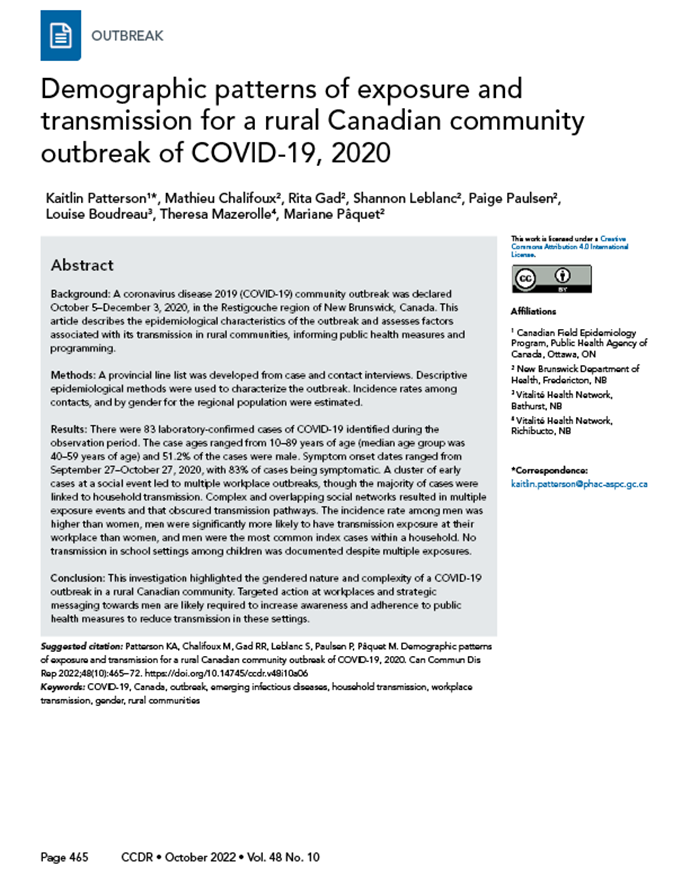
Case and testing demographics
A total of 83 laboratory-confirmed cases were associated with the community outbreak in Restigouche region between September 27, 2020, and November 5, 2020 (Figure 1) and 5,312 tests were conducted. None of the cases was genetically sequenced. Additionally, during the outbreak, three mass testing days were offered for asymptomatic individuals in Restigouche region (1,985 tests were conducted October 24, 25 and 30 during this mass testing). Slightly more females (58%) were tested than males (42%), and the majority (65%) of the tests were conducted among 40–79 year-olds.
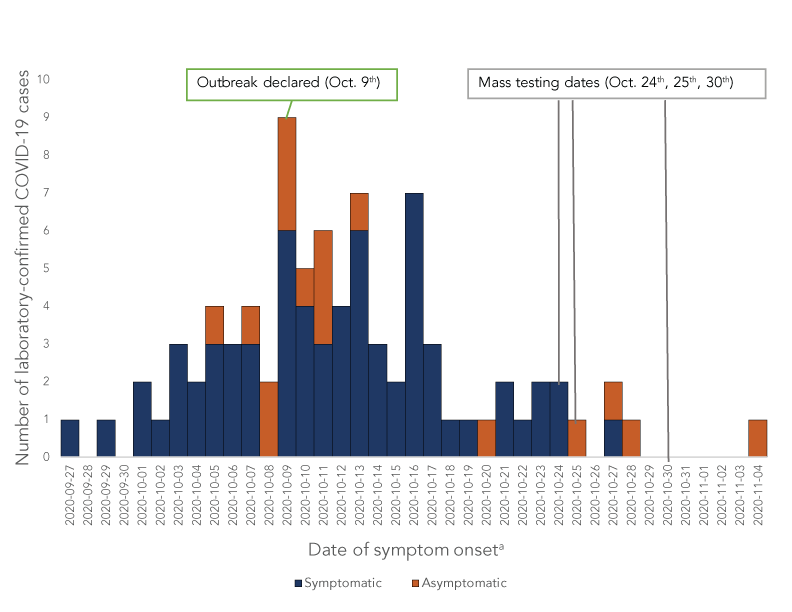
Figure 1 - Text description
| Dates | Symptomatic | Asymptomatic |
|---|---|---|
| 2020-09-27 | 1 | 0 |
| 2020-09-28 | 0 | 0 |
| 2020-09-29 | 1 | 0 |
| 2020-09-30 | 0 | 0 |
| 2020-10-01 | 2 | 0 |
| 2020-10-02 | 1 | 0 |
| 2020-10-03 | 3 | 0 |
| 2020-10-04 | 2 | 0 |
| 2020-10-05 | 3 | 1 |
| 2020-10-06 | 3 | 0 |
| 2020-10-07 | 3 | 1 |
| 2020-10-08 | 0 | 2 |
| 2020-10-09 | 6 | 3 |
| 2020-10-10 | 4 | 1 |
| 2020-10-11 | 3 | 3 |
| 2020-10-12 | 4 | 0 |
| 2020-10-13 | 6 | 1 |
| 2020-10-14 | 3 | 0 |
| 2020-10-15 | 2 | 0 |
| 2020-10-16 | 7 | 0 |
| 2020-10-17 | 3 | 0 |
| 2020-10-18 | 1 | 0 |
| 2020-10-19 | 1 | 0 |
| 2020-10-20 | 0 | 1 |
| 2020-10-21 | 2 | 0 |
| 2020-10-22 | 1 | 0 |
| 2020-10-23 | 2 | 0 |
| 2020-10-24 | 2 | 0 |
| 2020-10-25 | 0 | 1 |
| 2020-10-26 | 0 | 0 |
| 2020-10-27 | 1 | 1 |
| 2020-10-28 | 0 | 1 |
| 2020-10-29 | 0 | 0 |
| 2020-10-30 | 0 | 0 |
| 2020-10-31 | 0 | 0 |
| 2020-11-01 | 0 | 0 |
| 2020-11-02 | 0 | 0 |
| 2020-11-03 | 0 | 0 |
| 2020-11-04 | 0 | 1 |
- Figure 1 - abbreviation
-
Abbreviation: COVID-19, coronavirus disease 2019
- Footnote a
-
For asymptomatic cases the date of specimen collection was used
The overall test positivity rate was 1.70% (2.76% excluding the mass testing) during the outbreak period. Among the laboratory confirmed cases, the highest proportion of cases was among 40–49 year-olds (38%), and 52% of cases were male (Table 1). Overall, males had a higher incidence rate than females (Figure 2). None of the cases reported identifying as "another gender" or "unknown".
| Characteristics | Number of confirmed cases | |
|---|---|---|
| n | % | |
| Age (years) | 83 | 100 |
| 19 and younger | 10 | 12.1 |
| 20–39 | 13 | 15.7 |
| 40–59 | 32 | 38.6 |
| 60–79 | 27 | 32.5 |
| 80 and older | 1 | 1.2 |
| Gender | ||
| Male | 43 | 51.8 |
| Female | 40 | 48.2 |
| Symptoms at time of interview | ||
| Asymptomatic | 14 | 16.9 |
| Symptomatic | 69 | 83.1 |
| SeverityFootnote a | ||
| Hospitalizations | 5 | 6.0 |
| Intensive care unit admissions | 3 | 3.6 |
| Mechanical ventilation | 2 | 2.4 |
| Deceased | 2 | 2.4 |
| Testing delay among symptomatic cases | ||
| Range in time to testing after symptom onset (days) | 0–12 | N/A |
| Mean time to testing after symptom onset (days) | 2.78 | N/A |
| Median time to testing after symptom onset (days) | 3 | N/A |
| ContactsFootnote b | ||
| Range in number of contacts | 0–34 | N/A |
| Mean number of contacts | 6.43 | N/A |
| Median number of contacts | 4.5 | N/A |
- Table 1 - abbreviation
-
Abbreviations: COVID-19, coronavirus disease 2019; N/A, not applicable
- Footnote a
-
Severity categories are not mutually exclusive. A total of five cases were hospitalized, among those five, three were admitted to the intensive care unit, among those three, two required mechanical ventilation and both of those cases died
- Footnote b
-
These numbers exclude cases 19 years of age and under due to the large influence of the number of school contacts
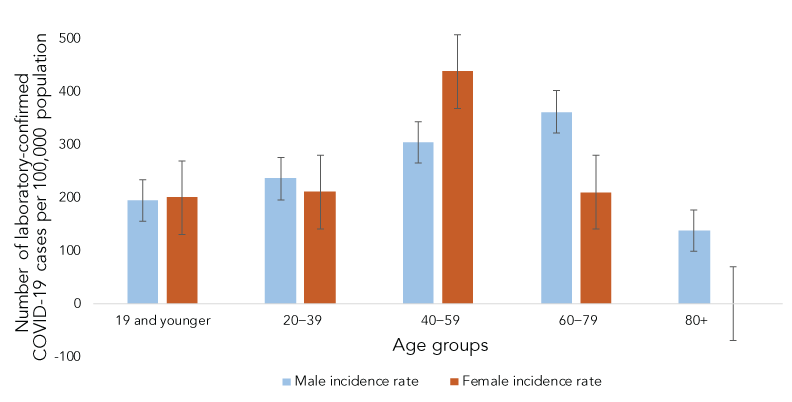
Figure 2 - Text description
| Age groups | Male incidence rate | Female incidence rate |
|---|---|---|
| 19 and younger | 195.5417 | 201.0454 |
| 20–39 | 236.6464 | 211.7149 |
| 40–59 | 304.8066 | 438.9004 |
| 60–79 | 362.628 | 210.5263 |
| 80+ | 138.3126 | 0 |
An initial cluster of seven cases was identified following a social gathering; no masking or physical distancing was reported among individuals attending the event. Symptom onset date and contact tracing were used to identify the probable source case (earliest symptom onset date with laboratory-confirmed COVID-19). None of the early cases had any travel exposure history or contact with known cases outside of the community. Because Restigouche region is on the border of New Brunswick and Québec, and as the Québec regions (Gaspésie–Îles-de-la-Madeleine and Bas Saint Laurent) bordering New Brunswick were experiencing community transmission and several outbreaks in the weeks leading up to this outbreak Footnote 3, the most likely introduction was as a result of interprovincial travel. As part of the "Atlantic Bubble", New Brunswick borders were controlled for interprovincial travel outside the Atlantic Provinces Footnote 4; however, residents on both sides of the Québec/New Brunswick border were exempt from travel restrictions if they were travelling for essential reasons (e.g. work, school and emergency services) Footnote 5. There was a series of indoor and outdoor events/gatherings held in the weeks prior to the identification of the outbreak that were mentioned during case investigations that did not fall within standard exposure periods (e.g. more than 14 days prior to episode onset). However, these events had both Québec and New Brunswick residents in attendance and may mean that some early cases were undetected.
The mean number of contacts per case was 6.43, with a total of 470 contacts of adult cases identified. Both men and women had similar mean numbers of reported contacts (6.25 and 6.61, respectively), but the median number of contacts for men was higher (6 versus 4). Of these contacts, 39 subsequently tested positive, resulting in a secondary attack rate of approximately 8.2% among identified case contacts. The remaining cases were not identified through contact tracing prior to testing positive for COVID-19. Forty-two were linked to cases through backwards contact tracing.
Among laboratory confirmed cases, men aged 20–39 years sought testing significantly longer after symptom onset (3.57 days after symptom onset) than women (1.2 days after symptom onset) (p>0.05). Additionally, cases aged 60 years or older (4.64 days after symptom onset) sought testing significantly (p>0.01) longer after symptom onset than cases younger than 60 years of age (2.63 days after symptom onset). Men and women had similar proportions of asymptomatic cases at time of testing, hospitalizations, admissions to intensive care units, mechanical ventilations, and deaths.
Among cases younger than 19 years of age, 210 contacts were identified and isolated (mean number of contacts per case was 23.33, significantly higher than cases older than 19 years of age). There were no secondary cases identified and no transmission observed in schools, school buses or child/youth-related activities. All adolescent cases were linked to household contacts (none were the primary case of the household) and resulted in no secondary transmission to non-household contacts, despite exposing contacts during their infectious periods.
Among all cases, there were significant differences in exposure by gender (Figure 3). Women were most likely to be exposed by family and/or household members (67% vs. 40% p>0.05) whereas men were more likely to be exposed at their workplace or through social interactions (60% vs 37% p>0.05).
Figure 3 - Text description
| Suspected transmission setting | Female | Male |
|---|---|---|
| Unknown | 2.50% | 2.33% |
| Social | 17.50% | 20.93% |
| Workplace | 15.00% | 37.21% |
| Family contact | 65.00% | 39.53% |
| Grand total | 100.00% | 100.00% |
Clusters
Through case interviews, contact tracing and analysis of the local line list, we were able to link all cases to two main transmission chains (Figure 4). Additionally, we identified a total of seven clusters of three or more confirmed cases associated with settings, events or locations where transmission may have occurred. A social event likely preceded the majority of transmission chains identified during the community outbreak. We also identified clusters among social outings with overnight stays and at several workplaces. Finally, we identified one family cluster we were unable to connect with other chains of transmission (Figure 4).
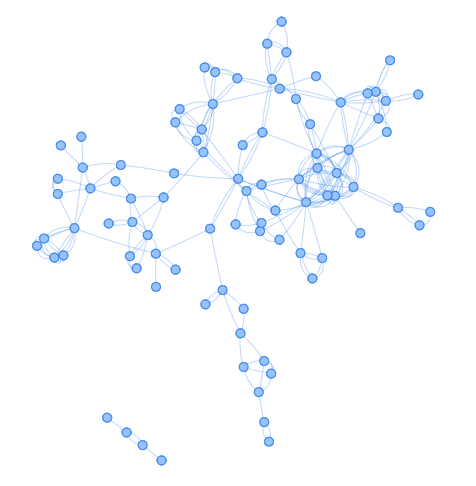
Figure 4 - Text description
Figure 4 shows the social network analysis of cases included in the COVID-19 outbreak investigation. There are a total of 83 nodes. There are two distinct clusters one with 79 nodes linked, and the second cluster has a total of 4 nodes linked. The network diagram shows multiple links between cases illustrating a tightly connected and overlapping network among cases.
- Figure 4 - abbreviation
-
Abbreviation: COVID-19, coronavirus disease 2019
- Footnote a
-
Each node represents a case
- Footnote b
-
Due to privacy considerations, the sequence of cases and clusters are not identified in this figure
Discussion
Introduction of COVID-19 into Restigouche region most likely occurred through travel for essential reasons across the New Brunswick-Québec borders, given the strict provincial border quarantine measures and absence of evidence of ongoing community transmission prior to the outbreak. The leading hypotheses are linked to a series of indoor and outdoor events/gatherings held in the weeks prior to the identification of the outbreak. These events had both Québec and New Brunswick residents in attendance. Interprovincial spread of COVID-19 cases due to land travel has been difficult to track throughout Canada, as each case is reported to the public health unit of their residence. Alternatively, it is possible COVID-19 was circulating undetected within the community from another source of introduction, and it was only identified upon reaching a critical threshold, resulting in rapid spread Footnote 6. However, undetected widespread community transmission in this case is unlikely, given the relatively short duration and small number of cases linked to this outbreak.
Globally, men have a higher proportion of COVID-19 case counts than women, and experience more severe illness and higher mortality Footnote 7. In this outbreak, we also found that the incidence rate among men was significantly higher than among women and that men were more likely to be the index case in workplaces and households, despite fewer men getting tested. Research of other health outcomes has found that male gender expectations within communities and work environments can drive various high-risk behaviours (e.g. poor health seeking behaviours and drinking and driving) Footnote 8. Emerging evidence on COVID-19 has found that women are more likely than men to follow government recommendations, take health precautions (e.g. mask-wearing, physical distancing, handwashing and staying at home) and encourage others to take health precautions Footnote 9 Footnote 10. Decreasing adherence to public health measures for COVID-19, such as staying at home, physical distancing and reducing contacts, has been observed over time regardless of gender Footnote 11. We also observed that older adults had longer delays in testing and had more contacts than younger adults. Often, older adults delayed seeking care because they underestimated the seriousness of their condition and attributed severity of symptoms as inevitable due to their age Footnote 12. Alternatively, older adults may have delayed seeking care because they had issues accessing transportation or don't know where to seek help Footnote 12.
Perception of risk of COVID-19 exposure may be underestimated in areas with low community transmission and case numbers. Several case contacts identified through backwards contact tracing were not initially reported as contacts as they did not meet the "two metres/15-minute interaction" criteria to be classified as a contact during the outbreak time period. This lack of reporting may have been as a result of a reluctance to disclose those interactions, or because individuals underestimated the time or overestimated the distance of their interactions Footnote 13. Another possibility is that transmission occurred despite those adhering to the two metres/15-minute interaction rule; however, most cases in this outbreak were linked to close contact with a known case. In backward contact tracing studies, an over dispersion effect has been observed, where the likelihood of transmission varies by case, and that certain events and individuals lead to a large number of secondary cases Footnote 14. It is possible that not all exposures to cases and/or events were captured.
Complex social networks that led to multiple exposures and transmissions throughout the region were identified. Other rural outbreaks of COVID-19 have been similarly characterized, and alternative approaches have been used to classify exposures and households where these networks occur Footnote 15. Modelling has demonstrated that full lockdowns for 14 days in these tightly connected communities can reduce significantly both the extent of the outbreak and the length, potentially reducing cases by 95% Footnote 16.
No transmission in schools or between children was detected in this outbreak, despite children being in contact during their infectious period. At the time of the outbreak, children were required to wear masks, all extracurricular activities were cancelled and most schools were using classroom cohorts to mitigate potential spread. Two hundred and ten individuals were required to isolate for 14 days after their last identified exposure in school settings; no cases were subsequently identified among these contacts. This finding is similar to evidence from the global literature that secondary cases in school environments between children are rare for COVID-19, especially when public health measures, such as masking, are being followed Footnote 17 Footnote 18.
Recommendations/implications for public health
Public health moved quickly to contain the outbreak presented here using enhanced non-pharmaceutical public health measures (including mandatory masking in public placement, workplace assessments, gathering limits) and the closure of nonessential services. As the Canadian population is increasingly vaccinated, and public health measures are reduced, it is likely that under-vaccinated populations and areas may experience increased numbers of cases and outbreaks. Early evidence is emerging that in rural areas, COVID-19 vaccine hesitancy is higher and vaccine coverage is lower than in urban areas Footnote 19.
In preparing for future outbreaks and emergence of cases the following should be considered, particularly if more transmissible variants are introduced:
- Public health education about the efficacy of public health measures (e.g. mask wearing and physical distancing) has been effective in increasing voluntary compliance with jurisdictional rules and recommendations Footnote 6; however, targeted messaging by gender and age is likely required to increase adherence to public health measures specifically among older men Footnote 7. In particular, the identification of trusted messengers (e.g. group leaders, peers, friends, family) has been effective in advocating for public health measures, including vaccination, in targeted groups and rural and remote communities Footnote 20.
- Less stringent approaches to managing contacts related to school exposures may be warranted; however, risk will be dependent on community rates of transmission, the nature of the exposure, age demographic of students, rates of vaccination and the variant in circulation.
- Communication of risks related to travel and exposure to individuals who have travelled may be necessary in low-prevalence areas, where risks may be perceived as non-existent.
- If staffing and resources permit, utilizing both forward and backward contact tracing is preferable, using backward contact tracing has resulted in identifying 2–3 times more cases Footnote 21. In rural and/or remote regions often with little to no incidence of COVID-19, identifying the source(s) of infection is critical for controlling spread and prevention strategies in the future Footnote 22.
- The number of significant interactions not recognized as such was large in this rural setting. Investigations in these settings may benefit from a broader set of criteria for identifying contacts, including lower thresholds for defining exposure interactions Footnote 23. Individuals may perceive a fifteen-minute interaction as less time (e.g. "I only stopped in to say hi") Footnote 24. Improving the clarity of public health measures and addressing changes to the measures are critical for acceptance and adherence Footnote 25. While these changes may not be feasible for public health follow-up due to limited resources, this clarification will support individual's ability to assess risk and make decisions in the context of outbreaks and more transmissible variants.
Limitations
Several limitations warrant discussion. First, because 30% of cases presented as asymptomatic certain dynamics of transmission may have been misclassified. In these cases, we used a combination of exposure information and specimen collection date to assess plausibility. Second, we relied on self-reported exposure information, and we only implemented backward contact tracing in the middle of the outbreak. This may have resulted in missed exposures and or transmission events. Third, we did not have any genomic data to identify whether the outbreak was linked to one or more introductions. At the time of this outbreak investigation, whole genome sequencing was not available in New Brunswick. All whole genome sequencing was conducted through the National Microbiology Laboratory in Winnipeg, Manitoba and because 95% of the cases were linked epidemiologically, sequencing the outbreak cases was not a high priority.
Conclusion
This investigation highlighted the gendered nature and complexity of a COVID-19 outbreak in a rural Canadian community. Targeted action at workplaces and strategic messaging towards men are likely required to increase awareness and adherence to public health measures to reduce transmission in these settings.
Authors' statement
KAP — Conceptualized, obtained datasets, methodology, analyzed and interpreted data, drafted and revised the manuscript
MC — Conceptualized, obtained datasets, methodology, interpreted data, revised the manuscript
RRG — Conceptualized, obtained datasets, interpreted data, revised the manuscript
SL — Conceptualized, obtained datasets, interpreted data, revised the manuscript
PP — Analyzed and interpreted data, and revised the manuscript
LB — Conceptualized, collected data, obtained datasets, interpreted data, revised the manuscript
TM — Conceptualized, collected data, obtained datasets, interpreted data, revised the manuscript
MP — Conceptualized, obtained datasets, methodology, interpreted data, revised the manuscript
Competing interests
None.
Acknowledgements
We thank all of the public health nurses from Réseau de santé Vitalité and Horizon Health Network who supported the outbreak investigation and delivered impeccable and compassionate services to clients throughout the COVID-19 pandemic; in particular, M Bujold-Drapeau. We also thank all Public Health New Brunswick staff involved in supporting the outbreak investigation; in particular, the Medical Officers of Health and the members of the COVID-19 response unit, and the Epidemiology and Surveillance Branch. We thank the Canadian Field Epidemiology Program; in particular, F-W Tremblay, A Bilandzic and L Caron-Poulin, and K Wilkinson from the Public Health Agency of Canada, for their support and guidance during the outbreak investigation and the development of this manuscript.
Funding
This work was supported by the Public Health Agency of Canada and the New Brunswick Department of Health.
References
- Footnote 1
-
Statistics Canada. Population estimates, July 1, by census division, 2016 boundaries. Table 17-10-0139-01. Ottawa, ON: StatCan; 2022. https://doi.org/10.25318/1710013901
- Footnote 2
-
Government of New Brunswick. Six new cases / outbreak in Zone 5 over / COVID-19 vaccine planning / holiday guidance. Fredericton, NB: Government of New Brunswick; 2020. https://www2.gnb.ca/content/gnb/en/departments/premier/news/news_release.2020.12.0654.html
- Footnote 3
-
Pekar J, Worobey M, Moshiri N, Scheffler K, Wertheim JO. Timing the SARS-CoV-2 index case in Hubei province. Science 2021;372(6540):412–7. https://doi.org/10.1126/science.abf8003
- Footnote 4
-
CBC News. N.B. officials watching increase in COVID-19 cases across Québec border. September 16, 2020. https://www.cbc.ca/news/canada/new-brunswick/cases-spike-in-eastern-quebec-1.5726522
- Footnote 5
-
The Council of Atlantic Premiers. Atlantic Provinces Form Travel Bubble. June 24, 2020. https://immediac.blob.core.windows.net/cap-cmha/images/Newsroom/Draft%20news%20release%20(v7).pdf
- Footnote 6
-
CBC News. New Brunswick's travel bubble with Québec shrinks again. September 24, 2020. https://www.cbc.ca/news/canada/new-brunswick/second-quebec-region-booted-1.5737538
- Footnote 7
-
Tadiri CP, Gisinger T, Kautzy-Willer A, Kublickiene K, Herrero MT, Raparelli V, Pilote L, Norris CM; GOING-FWD Consortium. The influence of sex and gender domains on COVID-19 cases and mortality. CMAJ 2020;192(36):E1041–5. https://doi.org/10.1503/cmaj.200971
- Footnote 8
-
Betron M, Gottert A, Pulerwitz J, Shattuck D, Stevanovic-Fenn N. Men and COVID-19: Adding a gender lens. Glob Public Health 2020;15(7):1090–2. https://doi.org/10.1080/17441692.2020.1769702
- Footnote 9
-
Clark C, Davila A, Regis M, Kraus S. Predictors of COVID-19 voluntary compliance behaviors: An international investigation. Glob Transit 2020;2:76–82. https://doi.org/10.1016/j.glt.2020.06.003
- Footnote 10
-
Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: Panel evidence from eight countries. Proc Natl Acad Sci U S A 2020;117(44):27285–91. https://doi.org/10.1073/pnas.2012520117
- Footnote 11
-
Crane MA, Shermock KM, Omer SB, Romley JA. Change in Reported Adherence to Nonpharmaceutical Interventions during the COVID-19 Pandemic, April-November 2020. JAMA 2021;325(9):883–5. https://doi.org/10.1001/jama.2021.0286
- Footnote 12
-
Teo K, Churchill R, Riadi I, Kervin L, Wister AV, Cosco TD. Help-Seeking Behaviors Among Older Adults: A Scoping Review. J Appl Gerontol 2022;41(5):1500–10. https://doi.org/10.1177/07334648211067710
- Footnote 13
-
Lewis D. Why many countries failed at COVID contact-tracing — but some got it right. Nature 2020;588(7838):384–7. https://doi.org/10.1038/d41586-020-03518-4
- Footnote 14
-
Public Health Ontario. Focus on: Backward Contact Tracing. Toronto, ON: PHO; 2021. https://www.publichealthontario.ca/-/media/documents/ncov/phm/2021/05/covid-19-backward-contact-tracing.pdf?la=en#:~:text=Backward%20contact%20tracing%20(BCT)%20is,than%20forward%20contact%20tracing%20alone
- Footnote 15
-
Lavezzo E, Franchin E, Ciavarella C, Cuomo-Dannenburg G, Barzon L, Del Vecchio C, Rossi L, Manganelli R, Loregian A, Navarin N, Abate D, Sciro M, Merigliano S, De Canale E, Vanuzzo MC, Besutti V, Saluzzo F, Onelia F, Pacenti M, Parisi SG, Carretta G, Donato D, Flor L, Cocchio S, Masi G, Sperduti A, Cattarino L, Salvador R, Nicoletti M, Caldart F, Castelli G, Nieddu E, Labella B, Fava L, Drigo M, Gaythorpe KAM; Imperial College COVID-19 Response Team, Brazzale AR, Toppo S, Trevisan M, Baldo V, Donnelly CA, Ferguson NM, Dorigatti I, Crisanti A; Imperial College COVID-19 Response Team. Suppression of a SARS-CoV-2 outbreak in the Italian municipality of Vo’. Nature 2020;584(7821):425–9. https://doi.org/10.1038/s41586-020-2488-1
- Footnote 16
-
Hui BB, Brown D, Chisholm RH, Geard N, McVernon J, Regan DG. Modelling testing and response strategies for COVID-19 outbreaks in remote Australian Aboriginal communities. BMC Infect Dis 2021;21(1):929. https://doi.org/10.1186/s12879-021-06607-5
- Footnote 17
-
European Centre for Disease Prevention and Control. COVID-19 in children and the role of school settings in transmission - second update. Solna (Sweden): ECDC; July 8, 2021. https://www.ecdc.europa.eu/en/publications-data/children-and-school-settings-covid-19-transmission
- Footnote 18
-
Ismail SA, Saliba V, Lopez Bernal J, Ramsay ME, Ladhani SN. SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infect Dis 2021;21(3):344–53. https://doi.org/10.1016/S1473-3099(20)30882-3
- Footnote 19
-
Stojanovic J, Boucher VG, Gagne M, Gupta S, Joyal-Desmarais K, Paduano S, Aburub AS, Sheinfeld Gorin SN, Kassianos AP, Ribeiro PAB, Bacon SL, Lavoie KL. Global Trends and Correlates of COVID-19 Vaccination Hesitancy: Findings from the iCARE Study. Vaccines 2021;9(6):661. https://doi.org/10.3390/vaccines9060661
- Footnote 20
-
Lipsey AF, Waterman AD, Wood EH, Balliet W. Evaluation of first-person storytelling on changing health-related attitudes, knowledge, behaviors, and outcomes: A scoping review. Patient Educ Couns 2020;103(10):1922–34. https://doi.org/10.1016/j.pec.2020.04.014
- Footnote 21
-
Endo A, Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group; Leclerc QJ, Knight GM, Medley GF, Atkins KE, Funk S, Kucharski AJ. Implication of backward contact tracing in the presence of overdispersed transmission in COVID-19 outbreaks. Wellcome Open Res 2021;5:239. https://doi.org/10.12688/wellcomeopenres.16344.3
- Footnote 22
-
Kojaku S, Hébert-Dufresne L, Mones E, Lehmann S, Ahn YY. The effectiveness of backward contact tracing in networks. Nat Phys 2021;17:652–8. https://doi.org/10.1038/s41567-021-01187-2
- Footnote 23
-
BC Centre for Disease Control. Interim Guidance: Public Health Management of Cases and Contacts Associated with Novel Coronavirus (COVID-19) in the Community. Vancouver, BC: BCCDC; May 4, 2022. http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Epid/CD%20Manual/Chapter%201%20-%20CDC/COVID-19%20Public%20Health%20Guidance%20May%204_2022.pdf
- Footnote 24
-
Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, Spiegelhalter D, van der Linden S. Risk perceptions of COVID-19 around the world. J Risk Res 2020;23(7-8):994–1006. https://doi.org/10.1080/13669877.2020.1758193
- Footnote 25
-
Balog-Way D, McComas KA. COVID-19: Reflections on trust, tradeoffs, and preparedness. J Risk Res 2020;23(7-8):838–48. https://doi.org/10.1080/13669877.2020.1758192
