National Influenza Annual Report, Canada, 2021–2022

 Download this article as a PDF
Download this article as a PDFPublished by: The Public Health Agency of Canada
Issue: Volume 48-10, October 2022: Equity, Diversity and Inclusion in Public Health
Date published: October 2022
ISSN: 1481-8531
Submit a manuscript
About CCDR
Browse
Volume 48-10, October 2022: Equity, Diversity and Inclusion in Public Health
Surveillance
National Influenza Annual Report, Canada, 2021–2022: A brief, late influenza epidemic
Steven Buckrell1, Myriam Ben Moussa1, Tammy Bui1, Abbas Rahal1, Kara Schmidt1, Liza Lee1, Nathalie Bastien2, Christina Bancej1
Affiliations
1 Centre for Immunization and Respiratory Infectious Diseases, Public Health Agency of Canada, Ottawa, ON
2 National Microbiology Laboratory, Public Health Agency of Canada, Winnipeg, MB
Correspondence
Suggested citation
Buckrell S, Ben Moussa M, Bui T, Rahal A, Schmidt K, Lee L, Bastien N, Bancej C. National Influenza Annual Report, Canada, 2021–2022: A brief, late influenza epidemic. Can Commun Dis Rep 2022;48(10):473–83. https://doi.org/10.14745/ccdr.v48i10a07
Keywords: influenza, influenza-like illness, surveillance, pandemic preparedness, COVID-19
Abstract
Canadian seasonal influenza circulation had been suppressed since the beginning of the coronavirus disease 2019 (COVID-19) pandemic. This suppression was reported globally and generated concern that the return of community influenza circulation could be intense and that co-circulation of influenza and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was possible and potentially severe. Community circulation of influenza returned to Canada during the 2021–2022 influenza season. The influenza epidemic began in week 16 (mid-April 2022) and lasted only nine weeks. This epidemic was driven by influenza A(H3N2) and was exceptionally late in the season, low in intensity and short in length. Community co-circulation of influenza and SARS-CoV-2 was observed in Canada for the first time during the 2021–2022 seasonal influenza epidemic. The unusual characteristics of the 2021–2022 influenza epidemic suggest that a breadth of factors moderate transmission dynamics of the two viruses. Concerns of an intense seasonal influenza epidemic did not come to fruition during the 2021–2022 season; therefore, high influenza susceptibility remains, as does predisposition to larger influenza epidemics. Ongoing circulation of SARS-CoV-2 creates uncertainty about dynamics of future influenza epidemics, but influenza vaccination remains a key public health intervention available to protect Canadians. Public health authorities need to remain vigilant, maintain surveillance and continue to plan for both heightened seasonal influenza circulation and for the potential for endemic co-circulation of influenza and SARS-CoV-2.
Introduction
In March 2020, widespread non-pharmaceutical interventions (NPIs) such as masking, border and travel measures and physical distancing were implemented in Canada and globally to curtail the spread of coronavirus disease 2019 (COVID-19). Since their implementation, typical seasonal influenza activity has been suppressed globally, and Canadian influenza activity remained at interseasonal levels through the entire 2020–2021 influenza season Footnote 1 Footnote 2 Footnote 3 Footnote 4 Footnote 5 Footnote 6 Footnote 7.
Suppression of influenza circulation raised concern that a resurgence of influenza would be observed with relaxation of NPIs Footnote 8. Natural infection or annual vaccination is required to gain immunity to seasonal influenza strains. Waning immunity, antigenic drift and a larger cohort of young children without exposure to natural infection may have increased the population susceptible to seasonal influenza. This increased susceptibility creates a population-level predisposition to high-intensity seasonal influenza epidemics Footnote 9.
Of additional concern, influenza resurgence could coincide with continued waves of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Co-circulation of these high burden viruses would pose a threat to public health and place pressure on health systems. Public health surveillance is essential to plan for and mitigate this threat.
Seasonal influenza activity re-emerged in Canada during the 2021–2022 influenza season. This surveillance report summarizes the 2021–2022 Canadian influenza season through analysis of FluWatch core indicators.
Methods
Design
FluWatch is a long-standing national surveillance system that monitors the spread of influenza and influenza-like illness (ILI) in Canada. FluWatch is a composite surveillance system consisting of virological surveillance, influenza and ILI activity level surveillance, syndromic surveillance, outbreak surveillance, severe outcome surveillance and vaccine monitoring. Annually, influenza surveillance is conducted across Canada from epidemiological week 35 to week 34 of the following year. For the 2021–2022 Canadian influenza season, this surveillance period began on August 28, 2021, and ended on August 27, 2022.
Indicator definitions and data sources
FluWatch indicator definitions and data sources are summarized in Table 1, as is a single external SARS-CoV-2 indicator and data source that was included in analyses.
| Component | Indicator | Operational definition | Description of data source |
|---|---|---|---|
| FluWatch | |||
| Virological | Weekly percentage of RT-PCR influenza tests positive. | Numerator: weekly number of influenza detections. Denominator: total weekly number of influenza tests reported. |
Respiratory Virus Detections Surveillance System: Laboratory test counts are reported by public health laboratories from all P/Ts, and five hospital laboratories/networks. Primary surveillance target populations are acute respiratory infection cases at emergency departments, hospitalized severe acute respiratory virus infection cases, and influenza outbreak cases. Outpatient ILI cases may be targeted, but testing is typically limited to higher-risk individuals and algorithms vary by P/T. Case-level data is available for a subset of detections. |
| Counts of influenza detections by age group, type, and/or subtype. | N/A | ||
| Influenza/ILI activity levels | Weekly influenza/ILI activity level, based on activity within each influenza surveillance region over the preceding week. | Four levels of activity used for weekly classification: No activity: no laboratory-confirmed influenza detections during reporting week. Sporadic: sporadic ILI cases and influenza detections, but no outbreaks. Localized: increased ILI cases, influenza detections, and outbreaks occurring in less than 50% of the surveillance region. Widespread: increased ILI cases, influenza detections, and outbreaks occurring in 50% or more of the surveillance region. |
Epidemiologists from all P/Ts report weekly influenza/ILI activity level for influenza surveillance regions. |
| Syndromic | Weekly percentage of patients seen by primary healthcare providers with ILI. | ILI: acute onset of respiratory illness with fever and cough and one or more of sore throat, arthralgia, myalgia or prostration. Numerator: weekly number of patients seen with ILI. Denominator: total weekly number of patients seen. |
Sentinel Primary Care Provider ILI: Primary healthcare providers across Canada report on patients presenting with ILI. |
| Weekly percentage of FluWatchers participants reporting ILI. | ILI: acute cough and fever. Numerator: weekly number of participants reporting ILI. Denominator: total weekly participants reporting. |
FluWatchers: Volunteer participants across Canada report episodes of cough and fever experienced in the preceding week via an online questionnaire. |
|
| Outbreaks | Number of weekly laboratory-confirmed influenza outbreaks by setting. | Outbreak: two or more cases of ILI reported in the setting during a seven-day period with at least one case laboratory-confirmed as influenza. | Epidemiologists from all P/Ts report weekly. All P/Ts report outbreaks in hospitals and long-term care facilities. Some report in additional settings such as remote/isolated communities, schools/daycare, and "other" settings (includes locations such as retirement homes, assisted living, shelters and correctional facilities). |
| Severe outcomes | Weekly/cumulative influenza-associated hospitalization rates per 100,000 population. | Hospitalization rate: Numerator: number of influenza-associated hospitalizations. Denominator: combined population of reporting P/Ts. |
Provincial/Territorial Severe Outcome Surveillance: Nine P/T Ministries of Health (AB, MB, SK, NS, NB, NL, PE, YT and NT) report laboratory-confirmed influenza-associated hospitalizations, ICU admissions and deaths. |
| Counts of weekly influenza-associated hospitalizations, ICU admissions and deaths. | N/A | ||
| Counts of weekly influenza-associated hospitalizations, ICU admissions, and deaths among paediatric population by age group, type and/or subtype. | N/A | IMPACT: Sentinel network that reports paediatric laboratory-confirmed influenza-associated hospitalizations (16 years and younger). Detailed case-level data is reported by the network's 12 paediatric hospitals across eight P/Ts (BC, AB, SK, MB, ON, QC, NS and NL). |
|
| Counts of weekly influenza-associated hospitalizations, ICU admissions and deaths among adult population by age group, type and/or subtype. | N/A | CIRN–SOS: Sentinel hospital network that reports adult laboratory-confirmed influenza-associated hospitalizations (16 years and older). Detailed case-level data is reported by the network's nine hospitals across four P/Ts (AB, ON, QC and NS). |
|
| Viral characterization | Counts and proportions of influenza isolates antigenically similar to the vaccine strains. | N/A | National Microbiology Laboratory: P/T public health laboratories forward a subset of influenza isolates to the National Microbiology Laboratory from cases detected throughout the season. Specimens undergo genetic characterization, antigenic characterization, and/or antiviral susceptibility testing. Genetic characterization is established by sequencing the HA gene of the influenza viruses to compare their genetic properties. Antigenic characterization is established by HA inhibition assay. Drug susceptibility is determined by chemiluminescence assay. |
| Counts and proportions of influenza isolates susceptible to antivirals. | N/A | ||
Vaccine monitoring |
Percentage of Canadian adults who received the seasonal influenza vaccine during the current influenza season. | N/A | Public Health Agency of Canada's Seasonal Influenza Immunization Coverage Survey: Annual telephone survey conducted in January and February to assess seasonal influenza vaccine coverage among adults aged 18 years and older. |
| Effectiveness of seasonal influenza vaccination against laboratory-confirmed influenza-associated medically attended illness and hospitalization. | VE estimates are estimated by test negative design and calculated as: VE=100%×(1-O_pos/O_neg) where Opos is the odds of vaccination among those testing positive for influenza and Oneg is the odds of vaccination among those testing negative. |
SPSN and CIRN-SOS: These networks calculate and report vaccine effectiveness against laboratory-confirmed influenza-associated medically attended illness and hospitalization, respectively. |
|
| External | |||
| SARS-CoV-2 virological | Seven-day moving average percentage of SARS-CoV-2 tests positive. | Numerator: number of SARS-CoV-2 detections over the previous seven days. Denominator: total SARS-CoV-2 tests over the previous seven days. |
Publicly available data from the Public Health Agency of Canada Footnote 10. SARS-CoV-2 case and testing data published by provincial and territorial partners are collated and published. |
|
|||
Statistical analysis
Data cleaning, manipulation, and analysis of counts, rates and proportions were all performed in SAS v9.4. Visualizations of analyses were prepared in Microsoft Excel. Comparisons to pre-pandemic indicator data were presented where possible. Seasons used for comparison varied by data source, depending on stability, data quality and data comparability over time (Table 2).
| Influenza season | FluWatch component | |||||
|---|---|---|---|---|---|---|
| Virological | Sentinel primary care provider ILI | FluWatchers | Outbreaks | P/T-SOSFootnote a | IMPACT | |
| 2014–2015 | Yes | Yes | No | No | No | Yes |
| 2015–2016 | Yes | Yes | No | No | No | Yes |
| 2016–2017 | Yes | Yes | Yes | No | Yes | Yes |
| 2017–2018 | Yes | Yes | Yes | No | Yes | Yes |
| 2018–2019 | Yes | Yes | Yes | Yes | Yes | Yes |
| 2019–2020Footnote b | Yes | Yes | Yes | Yes | Yes | Yes |
- Table 2 - abbreviation
-
Abbreviations: ILI, influenza-like illness; IMPACT, Canadian Immunization Monitoring Program ACTive; P/T-SOS, Province/Territory Severe Outcomes Surveillance
- Footnote a
-
Only cumulative end-of-season data is available prior to the 2019–2020 season
- Footnote b
-
In weekly comparisons to the 2019–2020 season, data from week 11 onwards is excluded due to the COVID-19 pandemic
Results
Virological
Early in the season, an increase in sporadic detections was recorded from week 48 to 51 (late-November to late-December 2021; 231 detections) but remained well below the seasonal epidemic threshold (5% or more tests positive and 15 or more detections). Detections then decreased, with fewer than 10 weekly detections reported from week 3 to 8 (late-January to late-February 2022). In week 16, influenza activity surpassed the epidemic threshold, and a national influenza epidemic was declared in Canada for the first time in two years.
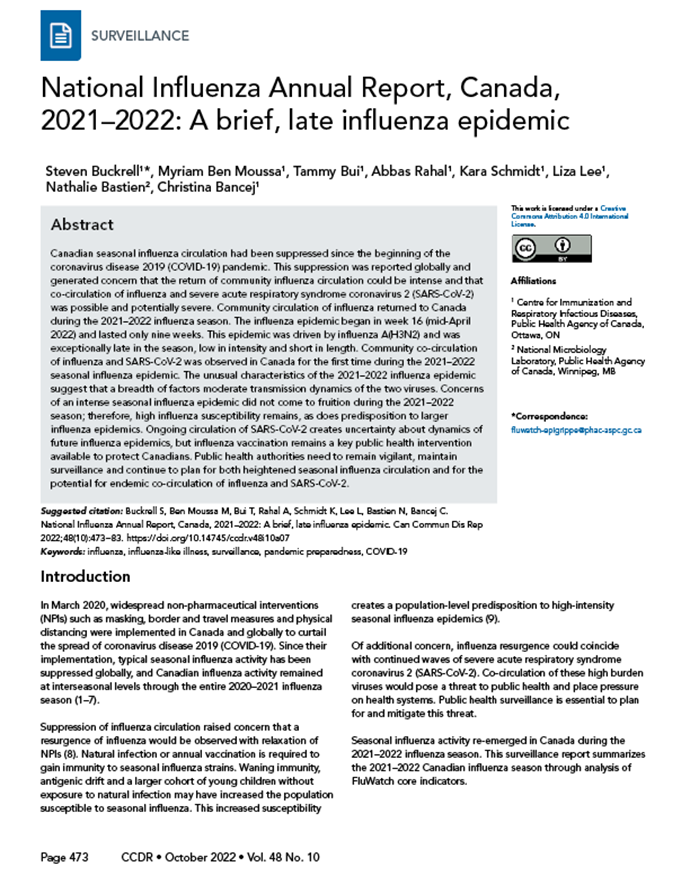
The 2021–2022 seasonal influenza epidemic began exceptionally late in the season and lasted nine weeks, from week 16 to 25 (late-April to mid-June 2022; Figure 1). Nationally, in pre-pandemic seasons, epidemics have typically begun around week 47 (mid to late-November) and lasted 27 weeks on average.
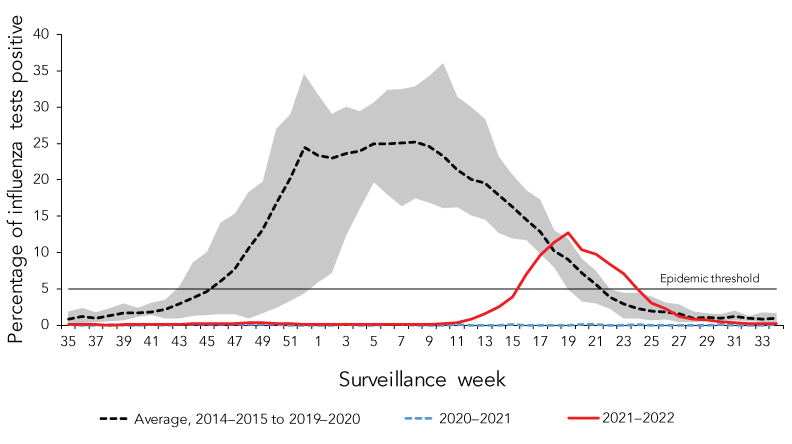
Figure 1 - Text description
| Surveillance week | 2021–2022 | 2020–2021 | Average 2014–2015 to 2019–2020 |
Minimum 2014–2015 to 2019–2020 |
Maximum 2014–2015 to 2019–2020 |
|---|---|---|---|---|---|
| 35 | 0.04 | 0.02 | 0.82 | 0.11 | 1.87 |
| 36 | 0.01 | 0.00 | 1.13 | 0.30 | 2.28 |
| 37 | 0.03 | 0.00 | 0.99 | 0.40 | 1.78 |
| 38 | 0.00 | 0.02 | 1.30 | 0.55 | 2.35 |
| 39 | 0.01 | 0.00 | 1.71 | 0.67 | 2.95 |
| 40 | 0.02 | 0.00 | 1.70 | 1.08 | 2.33 |
| 41 | 0.06 | 0.01 | 1.72 | 1.32 | 3.02 |
| 42 | 0.05 | 0.00 | 2.18 | 0.87 | 3.40 |
| 43 | 0.05 | 0.01 | 2.83 | 0.84 | 5.32 |
| 44 | 0.20 | 0.07 | 3.70 | 1.20 | 8.55 |
| 45 | 0.13 | 0.04 | 4.63 | 1.39 | 10.10 |
| 46 | 0.16 | 0.03 | 6.05 | 1.51 | 14.11 |
| 47 | 0.20 | 0.07 | 7.71 | 1.44 | 15.36 |
| 48 | 0.34 | 0.05 | 10.61 | 0.84 | 18.20 |
| 49 | 0.28 | 0.04 | 13.01 | 1.64 | 19.71 |
| 50 | 0.25 | 0.01 | 16.82 | 2.36 | 27.02 |
| 51 | 0.20 | 0.01 | 20.11 | 3.30 | 29.09 |
| 52 | 0.10 | 0.00 | 24.48 | 4.28 | 34.54 |
| 1 | 0.08 | 0.00 | 23.41 | 5.85 | 31.66 |
| 2 | 0.12 | 0.00 | 23.01 | 7.06 | 29.10 |
| 3 | 0.05 | 0.01 | 23.63 | 12.24 | 30.07 |
| 4 | 0.05 | 0.00 | 23.96 | 15.89 | 29.45 |
| 5 | 0.04 | 0.00 | 24.90 | 19.60 | 30.62 |
| 6 | 0.05 | 0.02 | 25.00 | 17.89 | 32.39 |
| 7 | 0.02 | 0.01 | 25.05 | 16.28 | 32.51 |
| 8 | 0.08 | 0.00 | 25.14 | 17.45 | 32.87 |
| 9 | 0.12 | 0.00 | 24.59 | 16.80 | 34.28 |
| 10 | 0.16 | 0.00 | 23.22 | 16.05 | 35.99 |
| 11 | 0.27 | 0.01 | 21.41 | 16.19 | 31.41 |
| 12 | 0.86 | 0.00 | 20.10 | 15.03 | 30.03 |
| 13 | 1.52 | 0.00 | 19.56 | 14.50 | 28.25 |
| 14 | 2.49 | 0.00 | 17.86 | 12.66 | 23.16 |
| 15 | 3.86 | 0.01 | 16.27 | 11.95 | 20.73 |
| 16 | 6.99 | 0.00 | 14.48 | 11.64 | 18.52 |
| 17 | 9.68 | 0.00 | 12.83 | 9.76 | 17.30 |
| 18 | 11.29 | 0.00 | 10.26 | 7.88 | 13.02 |
| 19 | 12.63 | 0.00 | 8.98 | 4.96 | 11.95 |
| 20 | 10.35 | 0.01 | 7.22 | 3.19 | 9.13 |
| 21 | 9.77 | 0.01 | 5.60 | 2.97 | 7.45 |
| 22 | 8.44 | 0.00 | 3.86 | 2.19 | 4.96 |
| 23 | 7.01 | 0.00 | 2.86 | 0.87 | 4.39 |
| 24 | 5.01 | 0.02 | 2.25 | 0.81 | 4.36 |
| 25 | 3.03 | 0.00 | 1.88 | 0.63 | 3.95 |
| 26 | 2.25 | 0.00 | 1.81 | 0.69 | 3.08 |
| 27 | 1.23 | 0.00 | 1.48 | 0.42 | 2.83 |
| 28 | 0.79 | 0.00 | 0.91 | 0.41 | 1.84 |
| 29 | 0.68 | 0.00 | 1.09 | 0.47 | 1.55 |
| 30 | 0.38 | 0.04 | 0.90 | 0.46 | 1.46 |
| 31 | 0.30 | 0.00 | 1.11 | 0.58 | 1.93 |
| 32 | 0.18 | 0.00 | 0.92 | 0.52 | 1.19 |
| 33 | 0.18 | 0.00 | 0.85 | 0.40 | 1.69 |
| 34 | 0.22 | 0.02 | 0.92 | 0.42 | 1.57 |
- Footnote a
-
Comparison of 2021–2022 influenza season to previous seasons, 2014–2015 to 2019–2020 and 2020–2021
- Footnote b
-
The shaded area represents the maximum and minimum percentage of tests positive reported by week from 2014–2015 to 2019–2020. The epidemic threshold is 5% tests positive for influenza. When it is exceeded, and a minimum of 15 weekly influenza detections is reported, a seasonal influenza epidemic is declared
During the 2021–2022 influenza season, a total of 16,126 laboratory-confirmed influenza detections were reported out of 751,900 total laboratory tests (Table 3). Considerable geographic variation was observed, as the majority of detections were recorded in Québec (47%), Alberta (17%) and British Columbia (10%). Nearly all of the detections were influenza A (99%) and the influenza A(H3N2) subtype predominated, accounting for 98% of the 5,240 subtyped influenza A specimens (Figure 2).
| Province/territory | Influenza tests | Influenza detections | Peak weekly influenza percent positivity | Cumulative influenza percent positivity | |||||
|---|---|---|---|---|---|---|---|---|---|
| All influenza | Influenza A | Influenza B | |||||||
| % | 95% CIFootnote a | % | 95% CIFootnote a | ||||||
| Newfoundland and Labrador | 15,930 | 327 | 327 | 0 | 7.9 | 6.0–9.8 | 2.1 | 1.8–2.3 | |
| Prince Edward Island | 2,807 | 65 | 65 | 0 | 25.5 | 13.1–38.0 | 2.3 | 1.8–2.9 | |
| Nova Scotia | 27,351 | 431 | 422 | 9 | 8.3 | 6.1–10.4 | 1.6 | 1.4–1.7 | |
| New Brunswick | 21,601 | 495 | 495 | 0 | 25.9 | 21.6–30.3 | 2.3 | 2.1–2.5 | |
| Québec | 131,566 | 7,634 | 7,524 | 110 | 26.6 | 25.3–27.9 | 5.8 | 5.7–5.9 | |
| Ontario | 105,633 | 904 | 897 | 7 | 6.4 | 5.4–7.5 | 0.9 | 0.8–0.9 | |
| Manitoba | 60,920 | 577 | 577 | 0 | 9.4 | 7.4–11.3 | 0.9 | 0.9–1.0 | |
| Saskatchewan | 32,914 | 781 | 781 | 0 | 13.5 | 10.8–16.2 | 2.4 | 2.2–2.5 | |
| Alberta | 102,875 | 2,716 | 2,713 | 3 | 11.9 | 10.6–13.1 | 2.6 | 2.5–2.7 | |
| British Columbia | 225,352 | 1,558 | 1,462 | 96 | 3.9 | 3.2–4.5 | 0.7 | 0.7–0.7 | |
| Yukon Territory | 5,511 | 21 | 14 | 7 | 33.3 | 0.0–71.1 | 0.4 | 0.2–0.5 | |
| Northwest Territories | 2,263 | 207 | 207 | 0 | 31.5 | 23.4–39.6 | 9.1 | 8.0–10.3 | |
| Nunavut | 17,177 | 410 | 410 | 0 | 53.8 | 44.8–62.9 | 2.4 | 2.2–2.6 | |
| Canada | 751,900 | 16,126 | 15,894 | 232 | 12.6 | 12.1–13.1 | 2.1 | 2.1–2.2 | |
- Table 3 - abbreviation
-
Abbreviation: CI, confidence interval
- Footnote a
-
Binomial proportion Wald confidence interval
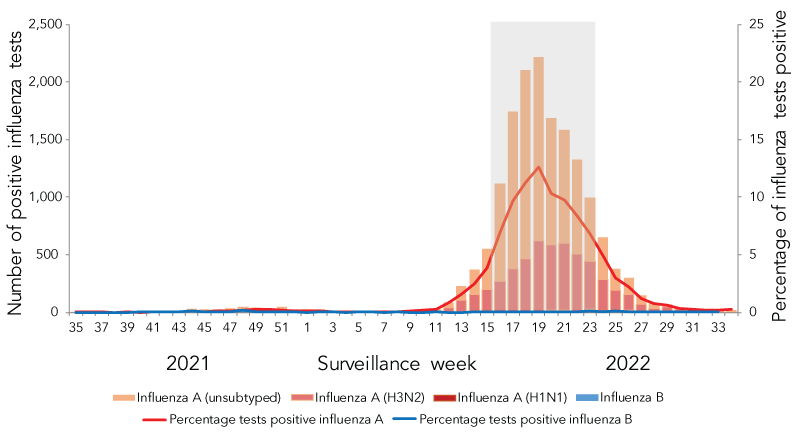
Figure 2 - Text description
The x-axis shows all epidemiological weeks of the 2021–2022 influenza season, weeks 35 to 34. The primary y-axis shows the count of positive influenza tests and the secondary y-axis shows the percentage of influenza tests positive. The striped red bars represent counts of unsubtyped influenza A; the light red bars represent counts of influenza A(H3N2); the dark red bars represent counts of influenza A(H1N1); the blue bars represent counts of influenza B; the red curve represents percentage of tests positive for influenza A; and the blue curve represents percentage of tests positive for influenza B.
Nearly all positive influenza tests during the 2021–2022 season were influenza A, and nearly all subtyped influenza A specimens were influenza A(H3N2). Very few positive influenza tests were reported until week 12, when detections of unsubtyped influenza A and influenza A(H3N2) began to increase, as did percentage of tests positive for influenza A. This increase continued until week 19 when percent of tests positive for influenza A peaked at 12.6%. Positive influenza tests and percentage of tests positive decreased consistently from thereon as the Canadian influenza epidemic, represented by the shaded area, began on week 16 and ended on week 25.
- Footnote a
-
The shaded area indicates weeks where the positivity rate was at least 5% and a minimum of 15 positive tests were observed, representing the 2021–2022 seasonal influenza epidemic
This influenza season was of low intensity, with weekly activity peaking in week 19 (mid-May 2022) at 12.6% tests positive, far below pre-pandemic seasonal peaks that averaged 31.5%. While influenza testing practices have changed during the COVID-19 pandemic, reflected by the total influenza test volume (n=751,900 vs an average of n=317,963 pre-pandemic), the elevated test volume does not account for the observed low peak epidemic percent positivity. Despite elevated testing, only 2,223 influenza detections were reported during the week 19 peak, much lower than the pre-pandemic average peak weekly detections (n=4,303). The 16,126 total detections were also quite low compared to the average 48,478 detections during pre-pandemic seasons.
Detailed information on age and influenza type/subtype was received for 14,159 laboratory-confirmed influenza detections of which 49% (n=7,169) were among individuals aged 0–19 years. Nearly half of influenza A(H3N2) detections (46%) were among individuals aged 0–19 years, an unusually young case distribution for an A(H3N2) dominant epidemic. In pre-pandemic seasons, an average of 17% of influenza A(H3N2) detections were among this age group (Table 4).
| Age group (years) |
Influenza season | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2014–2015 | 2015–2016 | 2016–2017 | 2017–2018 | 2018–2019 | 2019–2020 | 2021–2022 | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| 0–4 | 811 | 7% | 77 | 8% | 839 | 7% | 682 | 7% | 275 | 5% | 218 | 10% | 573 | 19% |
| 5–19 | 959 | 8% | 104 | 10% | 1,081 | 10% | 709 | 7% | 506 | 10% | 267 | 12% | 798 | 27% |
| 20–44 | 1,686 | 14% | 168 | 17% | 1,816 | 16% | 1,387 | 14% | 660 | 13% | 352 | 16% | 805 | 27% |
| 45–64 | 1,678 | 13% | 212 | 21% | 1,986 | 18% | 1,597 | 16% | 722 | 14% | 323 | 15% | 292 | 10% |
| 65 and older | 7,325 | 59% | 457 | 45% | 5,487 | 49% | 5,882 | 57% | 2,950 | 58% | 991 | 46% | 511 | 17% |
| Total | 12,459 | N/A | 1,018 | N/A | 11,209 | N/A | 10,257 | N/A | 5,113 | N/A | 2,151 | N/A | 2,979 | N/A |
- Table 4 - abbreviation
-
Abbreviation: N/A, not applicable
- Footnote a
-
Comparison of 2021–2022 influenza season to previous seasons, 2014–2015 to 2019–2020
Influenza/influenza-like illness activity levels
From week 40 (early-October) onwards, sporadic influenza activity was reported by at least one region in Canada in each week of the 2021–2022 influenza season. Nationally, the number of surveillance regions reporting sporadic or localized influenza activity reached a small peak in week 52 (late-December) and a larger peak in week 21 (late-May; Figure 3). Activity remained within peak levels from early-May to late-June. The first small peak mostly consisted of sporadic activity, whereas localized activity was more frequently reported during the second larger peak and was reported in multiple regions across Canada. Reported levels never exceeded localized activity.
Figure 3 - Text description
| Surveillance week | Sporadic | Localized |
|---|---|---|
| 35 | 2 | 0 |
| 36 | 0 | 0 |
| 37 | 0 | 0 |
| 38 | 2 | 0 |
| 39 | 0 | 0 |
| 40 | 2 | 0 |
| 41 | 3 | 0 |
| 42 | 6 | 0 |
| 43 | 3 | 0 |
| 44 | 2 | 0 |
| 45 | 3 | 0 |
| 46 | 10 | 0 |
| 47 | 7 | 0 |
| 48 | 10 | 0 |
| 49 | 13 | 0 |
| 50 | 18 | 0 |
| 51 | 12 | 1 |
| 52 | 19 | 0 |
| 1 | 15 | 1 |
| 2 | 15 | 0 |
| 3 | 12 | 1 |
| 4 | 8 | 0 |
| 5 | 8 | 0 |
| 6 | 4 | 0 |
| 7 | 6 | 0 |
| 8 | 3 | 0 |
| 9 | 5 | 0 |
| 10 | 8 | 0 |
| 11 | 13 | 0 |
| 12 | 15 | 1 |
| 13 | 20 | 4 |
| 14 | 25 | 7 |
| 15 | 30 | 4 |
| 16 | 28 | 9 |
| 17 | 34 | 8 |
| 18 | 33 | 9 |
| 19 | 35 | 14 |
| 20 | 37 | 13 |
| 21 | 39 | 12 |
| 22 | 33 | 15 |
| 23 | 36 | 13 |
| 24 | 40 | 10 |
| 25 | 38 | 6 |
| 26 | 38 | 3 |
| 27 | 31 | 5 |
| 28 | 31 | 3 |
| 29 | 26 | 2 |
| 30 | 27 | 1 |
| 31 | 16 | 2 |
| 32 | 11 | 1 |
| 33 | 8 | 0 |
| 34 | 12 | 0 |
Syndromic—Sentinel primary healthcare provider influenza-like illness surveillance
During the 2021–2022 season, a weekly average of only 50 sentinel primary care providers reported to the ILI surveillance program with a weekly average of 3,769 total patients seen; both metrics were lower than historical levels. On average, in pre-pandemic seasons, 134 sentinel providers reported to the surveillance program and 7,688 total patients were seen each week.
The weekly percentage of visits to primary care providers due to ILI ranged from 0.5% to 2.1% (Figure 4). There was no single defined peak in ILI visits observed this season, while in pre-pandemic seasons a peak was typically observed in late-December/early-January, with an average of 3.4% visits due to ILI at this time of season. From the start of the season to mid-April (week 35 to 15), weekly percentage of visits due to ILI were almost exclusively below historical averages. From week 16 onwards (mid-April), the weekly percentage of visits due to ILI was above historical averages following an increase in weekly ILI visits at a time of typical decrease. This late increase in ILI coincided with the late seasonal influenza epidemic.
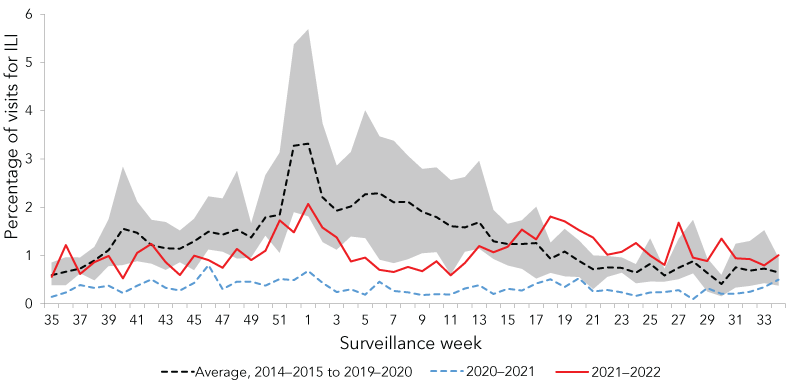
Figure 4 - Text description
| Surveillance Week | 2021–2022 | 2020–2021 | Average 2014–2015 to 2019–2020 |
Minimum 2014–2015 to 2019–2020 |
Maximum 2014–2015 to 2019–2020 |
|---|---|---|---|---|---|
| 35 | 0.56 | 0.14 | 0.59 | 0.38 | 0.85 |
| 36 | 1.21 | 0.23 | 0.66 | 0.38 | 0.96 |
| 37 | 0.62 | 0.39 | 0.73 | 0.62 | 0.96 |
| 38 | 0.86 | 0.33 | 0.90 | 0.48 | 1.18 |
| 39 | 0.99 | 0.37 | 1.11 | 0.78 | 1.74 |
| 40 | 0.53 | 0.22 | 1.55 | 0.80 | 2.84 |
| 41 | 1.05 | 0.37 | 1.47 | 0.88 | 2.11 |
| 42 | 1.24 | 0.50 | 1.22 | 0.83 | 1.74 |
| 43 | 0.86 | 0.33 | 1.15 | 0.70 | 1.69 |
| 44 | 0.59 | 0.27 | 1.14 | 0.86 | 1.51 |
| 45 | 1.00 | 0.43 | 1.30 | 0.69 | 1.76 |
| 46 | 0.90 | 0.80 | 1.49 | 1.12 | 2.22 |
| 47 | 0.75 | 0.30 | 1.43 | 1.07 | 2.18 |
| 48 | 1.13 | 0.46 | 1.54 | 0.93 | 2.75 |
| 49 | 0.90 | 0.46 | 1.37 | 0.95 | 1.66 |
| 50 | 1.10 | 0.37 | 1.79 | 1.40 | 2.66 |
| 51 | 1.73 | 0.51 | 1.84 | 1.05 | 3.13 |
| 52 | 1.48 | 0.49 | 3.27 | 1.89 | 5.37 |
| 1 | 2.07 | 0.68 | 3.32 | 1.81 | 5.69 |
| 2 | 1.58 | 0.44 | 2.21 | 1.27 | 3.73 |
| 3 | 1.37 | 0.24 | 1.93 | 1.11 | 2.86 |
| 4 | 0.87 | 0.30 | 2.02 | 1.39 | 3.14 |
| 5 | 0.96 | 0.19 | 2.27 | 1.35 | 4.00 |
| 6 | 0.70 | 0.46 | 2.29 | 0.91 | 3.47 |
| 7 | 0.66 | 0.26 | 2.10 | 0.84 | 3.37 |
| 8 | 0.76 | 0.24 | 2.11 | 0.92 | 3.06 |
| 9 | 0.67 | 0.18 | 1.91 | 1.04 | 2.79 |
| 10 | 0.88 | 0.20 | 1.80 | 1.07 | 2.82 |
| 11 | 0.59 | 0.19 | 1.61 | 0.60 | 2.56 |
| 12 | 0.84 | 0.31 | 1.58 | 1.07 | 2.62 |
| 13 | 1.19 | 0.38 | 1.69 | 1.14 | 2.96 |
| 14 | 1.07 | 0.20 | 1.29 | 0.92 | 1.94 |
| 15 | 1.18 | 0.31 | 1.24 | 0.79 | 1.65 |
| 16 | 1.54 | 0.27 | 1.24 | 0.72 | 1.73 |
| 17 | 1.33 | 0.42 | 1.26 | 0.52 | 2.01 |
| 18 | 1.81 | 0.50 | 0.93 | 0.63 | 1.26 |
| 19 | 1.71 | 0.35 | 1.08 | 0.56 | 1.55 |
| 20 | 1.53 | 0.53 | 0.89 | 0.55 | 1.31 |
| 21 | 1.37 | 0.25 | 0.71 | 0.30 | 1.00 |
| 22 | 1.02 | 0.29 | 0.75 | 0.55 | 0.99 |
| 23 | 1.08 | 0.24 | 0.74 | 0.64 | 0.96 |
| 24 | 1.26 | 0.16 | 0.64 | 0.42 | 0.82 |
| 25 | 1.00 | 0.23 | 0.83 | 0.46 | 1.35 |
| 26 | 0.80 | 0.24 | 0.59 | 0.45 | 0.72 |
| 27 | 1.68 | 0.28 | 0.74 | 0.50 | 1.34 |
| 28 | 0.96 | 0.09 | 0.88 | 0.62 | 1.73 |
| 29 | 0.89 | 0.32 | 0.64 | 0.25 | 0.94 |
| 30 | 1.35 | 0.21 | 0.41 | 0.15 | 0.59 |
| 31 | 0.94 | 0.21 | 0.75 | 0.33 | 1.24 |
| 32 | 0.92 | 0.25 | 0.69 | 0.36 | 1.30 |
| 33 | 0.79 | 0.34 | 0.73 | 0.42 | 1.52 |
| 34 | 1.00 | 0.50 | 0.65 | 0.37 | 0.95 |
- Figure 4 - abbreviation
-
Abbreviation: ILI, influenza-like illness
- Footnote a
-
Comparison of 2021–2022 influenza season to previous seasons, 2014–2015 to 2019–2020 and 2020–2021
- Footnote b
-
The shaded area represents the maximum and minimum percentage of visits for ILI reported by week from 2014–2015 to 2019–2020
Syndromic—FluWatchers
During the 2021–2022 season, an average of 12,045 FluWatchers participants reported each week. Overall, a total of 18,124 participants reported at least once this season, completing a total of 619,322 questionnaires.
The percentage of FluWatchers reporting ILI remained very low for the majority of the 2021–2022 season (Figure 5). From the beginning of the season to early-April (week 39 to 13), this percentage remained far below pre-pandemic levels. Despite this, a peak was observed in week 52 (early-January) at 1.5%. Five weeks later, a subsequent higher peak occurred in week 14 (early-April) at 2.3%, reaching expected levels for the first time of the season. A final peak in FluWatcher-reported ILI was observed in week 27 (early-July) at 2.0%.
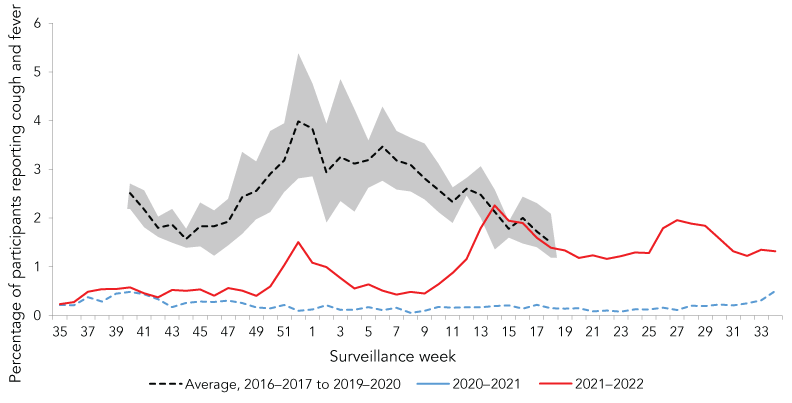
Figure 5 - Text description
| Surveillance week | 2021–2022 | 2020–2021 | Average 2016–2017 to 2019–2020 |
Minimum 2016–2017 to 2019–2020 |
Maximum 2016–2017 to 2019–2020 |
|---|---|---|---|---|---|
| 35 | 0.23 | 0.22 | - | - | - |
| 36 | 0.28 | 0.21 | - | - | - |
| 37 | 0.49 | 0.38 | - | - | - |
| 38 | 0.54 | 0.29 | - | - | - |
| 39 | 0.54 | 0.45 | - | - | - |
| 40 | 0.58 | 0.49 | 2.51 | 2.18 | 2.71 |
| 41 | 0.46 | 0.44 | 2.18 | 1.81 | 2.57 |
| 42 | 0.38 | 0.33 | 1.80 | 1.61 | 2.03 |
| 43 | 0.53 | 0.17 | 1.87 | 1.49 | 2.18 |
| 44 | 0.51 | 0.26 | 1.57 | 1.39 | 1.78 |
| 45 | 0.54 | 0.29 | 1.83 | 1.42 | 2.32 |
| 46 | 0.41 | 0.28 | 1.83 | 1.22 | 2.15 |
| 47 | 0.57 | 0.31 | 1.93 | 1.44 | 2.39 |
| 48 | 0.51 | 0.26 | 2.43 | 1.67 | 3.35 |
| 49 | 0.40 | 0.17 | 2.56 | 1.97 | 3.16 |
| 50 | 0.60 | 0.15 | 2.91 | 2.12 | 3.79 |
| 51 | 1.03 | 0.22 | 3.18 | 2.53 | 3.95 |
| 52 | 1.51 | 0.10 | 3.98 | 2.81 | 5.38 |
| 1 | 1.08 | 0.12 | 3.84 | 2.85 | 4.76 |
| 2 | 0.99 | 0.21 | 2.94 | 1.90 | 3.93 |
| 3 | 0.77 | 0.12 | 3.25 | 2.35 | 4.84 |
| 4 | 0.56 | 0.12 | 3.12 | 2.13 | 4.23 |
| 5 | 0.64 | 0.17 | 3.19 | 2.62 | 3.59 |
| 6 | 0.51 | 0.11 | 3.47 | 2.76 | 4.28 |
| 7 | 0.43 | 0.16 | 3.18 | 2.58 | 3.79 |
| 8 | 0.49 | 0.06 | 3.09 | 2.54 | 3.65 |
| 9 | 0.45 | 0.10 | 2.81 | 2.38 | 3.53 |
| 10 | 0.64 | 0.18 | 2.58 | 2.12 | 3.11 |
| 11 | 0.88 | 0.16 | 2.33 | 1.89 | 2.63 |
| 12 | 1.16 | 0.17 | 2.60 | 2.46 | 2.82 |
| 13 | 1.79 | 0.17 | 2.48 | 1.99 | 3.06 |
| 14 | 2.26 | 0.19 | 2.13 | 1.35 | 2.58 |
| 15 | 1.95 | 0.21 | 1.78 | 1.60 | 1.93 |
| 16 | 1.90 | 0.14 | 2.00 | 1.47 | 2.44 |
| 17 | 1.60 | 0.22 | 1.73 | 1.40 | 2.31 |
| 18 | 1.39 | 0.15 | 1.50 | 1.19 | 2.09 |
| 19 | 1.34 | 0.14 | - | - | - |
| 20 | 1.18 | 0.15 | - | - | - |
| 21 | 1.23 | 0.09 | - | - | - |
| 22 | 1.16 | 0.10 | - | - | - |
| 23 | 1.22 | 0.08 | - | - | - |
| 24 | 1.30 | 0.13 | - | - | - |
| 25 | 1.28 | 0.12 | - | - | - |
| 26 | 1.79 | 0.16 | - | - | - |
| 27 | 1.96 | 0.11 | - | - | - |
| 28 | 1.89 | 0.20 | - | - | - |
| 29 | 1.84 | 0.20 | - | - | - |
| 30 | 1.58 | 0.22 | - | - | - |
| 31 | 1.32 | 0.21 | - | - | - |
| 32 | 1.22 | 0.25 | - | - | - |
| 33 | 1.35 | 0.31 | - | - | - |
| 34 | 1.32 | 0.50 | - | - | - |
- Footnote a
-
Comparison of 2021–2022 influenza season to previous seasons, 2016–2017 to 2019–2020 and 2020–2021
- Footnote b
-
The shaded area represents the maximum and minimum percentage of percentage of participants reporting cough and fever by week, from 2016–2017 to 2019–2020
The percentage of FluWatchers reporting ILI aligned well with the percentage of SARS-CoV-2 laboratory tests that were positive in Canada (Figure 6). The first peak in FluWatchers ILI (week 52; 1.5%) occurred concurrently with SARS-CoV-2 activity reaching its maximum peak during the surveillance period. The highest peak in FluWatchers ILI (week 14; 2.3%) occurred during a smaller SARS-CoV-2 activity peak, and as influenza activity was approaching its highest peak of the season. During the third peak in FluWatchers ILI (week 27; 2.0%), ILI increased with SARS-CoV-2 activity while influenza positivity decreased.
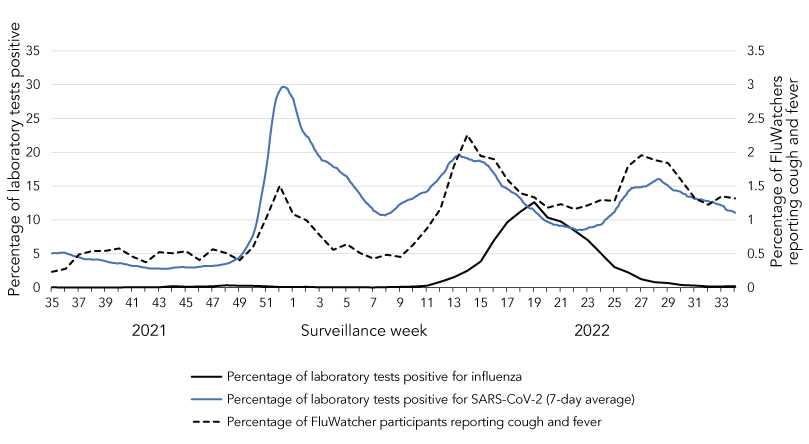
Figure 6 - Text description
The x-axis shows all epidemiological weeks of the 2021–2022 influenza season, weeks 35 to 34. The primary y-axis shows the percentage of laboratory tests positive for both influenza tests and SARS-CoV-2 tests. The secondary y-axis shows the percentage of FluWatcher participants reporting cough and fever. The black curve represents the percentage of influenza tests positive; the blue curve represents the percentage of SARS-CoV-2 tests positive; the dashed black curve represents the percentage of FluWatchers reporting cough and fever.
There is one distinct peak in percentage of tests positive for influenza, occurring in week 19 at 12.6%. Percentage of tests positive for SARS-CoV-2 and percentage of FluWatchers reporting cough and fever each have three peaks, occurring at similar times. The first of these shared peaks occurred in week 52, the largest peak in percentage of tests positive for SARS-CoV-2 (29.7%) but the smallest peak in FluWatchers reporting cough and fever (1.5%). The second shared peak occurred around week 14 and was the highest peak in FluWatchers reporting cough and fever (2.3%), while the third peak occurred around week 27.
Outbreaks
During the 2021–2022 season, 91 laboratory-confirmed influenza outbreaks were reported. The majority of laboratory-confirmed outbreaks (88%) were reported from week 11 to 24 (mid-March to mid-June), with the highest number of outbreaks in any given week (n=9) reported in week 16. Of reported laboratory-confirmed outbreaks, 49% were in long-term care facilities (n=45) and 38% were in facilities categorized as "other" (e.g. retirement homes, correctional facilities). All but one laboratory-confirmed outbreak were due to influenza A, and 96% (n=44) of outbreaks with subtype information were due to influenza A(H3N2).
This season, there were fewer laboratory-confirmed influenza outbreaks reported and a lower proportion of outbreaks occurred in long-term care facilities compared to recent pre-pandemic seasons. In the 2018–2019 and 2019–2020 seasons respectively, there were 978 and 1,038 total laboratory-confirmed outbreaks reported with 64% and 62% of outbreaks occurring in long-term care facilities.
Severe outcomes—Provincial/Territorial Severe Outcome Surveillance
During the 2021–2022 influenza season, 776 influenza-associated hospitalizations were reported by participating provinces and territories. Nearly all hospitalizations were associated with influenza A (99.6%), and among hospitalizations with subtype information, 99.5% (n=407) were associated with influenza A(H3N2).
The annual seasonal hospitalization incidence was nine hospitalizations per 100,000 population, much lower than rates recorded in pre-pandemic seasons where on average 42 hospitalizations per 100,000 population were recorded (Table 5). Similar to previous seasons, the annual seasonal hospitalization rates were highest among adults aged 65 years and older (21 per 100,000) and children aged 0–4 years (19 per 100,000). However, in past seasons of predominant influenza A(H3N2) circulation, hospitalization rates have been much higher among adults aged 65 years and older, relative to younger age groups (Table 5).
| Age group (years) |
Influenza season (predominant influenza of season) | ||||
|---|---|---|---|---|---|
| 2016–2017 (H3N2) |
2017–2018 (H3N2 & B) |
2018–2019 (H1N1) |
2019–2020 (H1N1 & B) |
2021–2022 (H3N2) |
|
| 0–4 | 46 | 70 | 98 | 77 | 19 |
| 5–19 | 9 | 17 | 21 | 16 | 7 |
| 20–44 | 5 | 12 | 15 | 14 | 5 |
| 45–64 | 15 | 41 | 40 | 23 | 6 |
| 65 and older | 128 | 280 | 127 | 76 | 21 |
| Overall | 30 | 64 | 45 | 30 | 9 |
- Footnote a
-
Comparison of 2021–2022 season to previous seasons, 2016–2017 to 2019–2020
The majority of this season's influenza-associated hospitalizations (94%) occurred from week 14 to 26, corresponding to the brief influenza epidemic experienced this season. While brevity contributes to this season's lower annual hospitalization incidence, weekly incidence peaked at 1.2 hospitalizations per 100,000; lower than the 2019–2020 season, which peaked at 2.9 hospitalizations per 100,000 and featured 13 consecutive weeks with a hospitalization rate greater than 1.2 per 100,000.
A total of 69 intensive care unit (ICU) admissions and 22 deaths were reported this season by participating provinces and territories. Of hospitalized cases, 9% were admitted to ICU; which is comparable to pre-pandemic seasons (average 11%; range 4%–17%). The ICU admissions were most common among adults 65 years of age and older (30%) and 45–64 years of age (26%). Deaths were most common among adults 65 years of age and older (59%).
Severe outcomes—Canadian Immunization Monitoring Program ACTive
The Canadian Immunization Monitoring Program ACTive (IMPACT) network preliminarily reported 303 influenza-associated paediatric hospitalizations during the 2021–2022 influenza season—far fewer than reported in pre-pandemic seasons. From 2014–2015 to 2019–2020, an average of 1,057 paediatric hospitalizations were reported, with 593 hospitalizations during the 2016–2017 season being the lowest reported in a single season.
Weekly preliminary paediatric hospitalizations remained below expected pre-pandemic levels for most of the 2021–2022 season but increased late in the season peaking in week 18 (early-May; n=48; Figure 7). This peak was of low intensity and late compared to prior seasons; on average, pre-pandemic paediatric hospitalizations peaked at 93 weekly hospitalizations, and peak weekly hospitalizations occurred no later than week 9.
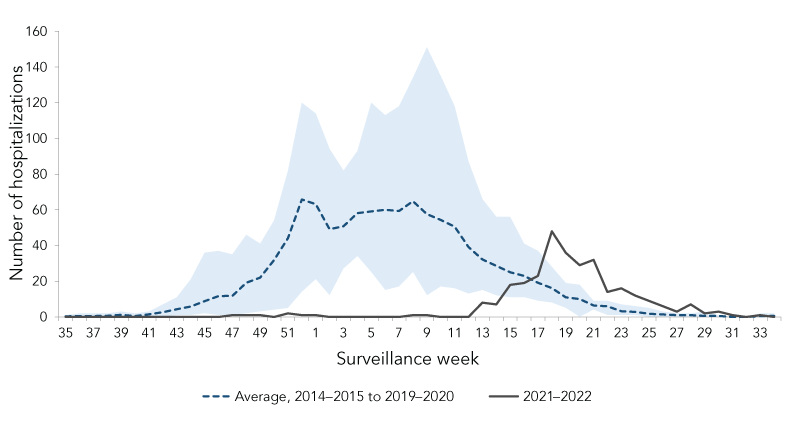
Figure 7 - Text description
| Surveillance week | 2021–2022 | Average 2014–2015 to 2019–2020 |
Minimum 2014–2015 to 2019–2020 |
Maximum 2014–2015 to 2019–2020 |
|---|---|---|---|---|
| 35 | 0 | 0 | 0 | 1 |
| 36 | 0 | 1 | 0 | 2 |
| 37 | 0 | 1 | 0 | 2 |
| 38 | 0 | 1 | 0 | 2 |
| 39 | 0 | 1 | 0 | 3 |
| 40 | 0 | 1 | 0 | 2 |
| 41 | 0 | 2 | 0 | 3 |
| 42 | 0 | 3 | 0 | 7 |
| 43 | 0 | 4 | 1 | 11 |
| 44 | 0 | 6 | 1 | 21 |
| 45 | 0 | 9 | 2 | 36 |
| 46 | 0 | 12 | 1 | 37 |
| 47 | 1 | 12 | 1 | 35 |
| 48 | 1 | 19 | 2 | 46 |
| 49 | 1 | 22 | 3 | 41 |
| 50 | 0 | 32 | 4 | 54 |
| 51 | 2 | 44 | 5 | 82 |
| 52 | 1 | 66 | 14 | 120 |
| 1 | 1 | 63 | 21 | 114 |
| 2 | 0 | 49 | 12 | 94 |
| 3 | 0 | 51 | 27 | 82 |
| 4 | 0 | 58 | 34 | 93 |
| 5 | 0 | 59 | 25 | 120 |
| 6 | 0 | 60 | 15 | 113 |
| 7 | 0 | 59 | 17 | 118 |
| 8 | 1 | 65 | 25 | 134 |
| 9 | 1 | 58 | 12 | 151 |
| 10 | 0 | 54 | 17 | 135 |
| 11 | 0 | 51 | 16 | 118 |
| 12 | 0 | 39 | 13 | 87 |
| 13 | 8 | 32 | 15 | 66 |
| 14 | 7 | 29 | 12 | 56 |
| 15 | 18 | 25 | 11 | 56 |
| 16 | 19 | 23 | 11 | 41 |
| 17 | 23 | 19 | 9 | 37 |
| 18 | 48 | 16 | 8 | 28 |
| 19 | 36 | 11 | 5 | 19 |
| 20 | 29 | 10 | 0 | 18 |
| 21 | 32 | 6 | 4 | 9 |
| 22 | 14 | 6 | 1 | 9 |
| 23 | 16 | 3 | 1 | 7 |
| 24 | 12 | 3 | 1 | 6 |
| 25 | 9 | 2 | 0 | 5 |
| 26 | 6 | 1 | 0 | 3 |
| 27 | 3 | 1 | 0 | 2 |
| 28 | 7 | 1 | 0 | 2 |
| 29 | 2 | 1 | 0 | 3 |
| 30 | 3 | 1 | 0 | 1 |
| 31 | 1 | 0 | 0 | 0 |
| 32 | 0 | 0 | 0 | 0 |
| 33 | 1 | 0 | 0 | 2 |
| 34 | 0 | 1 | 0 | 2 |
- Figure 7 - abbreviation
-
Abbreviation: IMPACT, Canadian Immunization Monitoring Program ACTive
- Footnote a
-
Comparison of 2021–2022 influenza season to previous seasons, 2014–2015 to 2019–2020
- Footnote b
-
The shaded area represents the maximum and minimum hospitalizations reported by week of admission, from 2014–2015 to 2019–2020
Almost all hospitalizations were associated with influenza A (99%), and among the 96 hospitalizations with subtype information, 98% were associated with influenza A(H3N2). Age distribution of paediatric hospitalizations was similar to pre-pandemic seasons, with hospitalized cases most commonly reported in patients younger than two years of age (32%).
There were 30 ICU admissions and fewer than five deaths reported this season. Of hospitalized cases, 10% were admitted to ICU; lower than pre-pandemic seasons (average 18%). The highest proportion of ICU admissions was reported among patients 10–16 years (30%) and 2–4 years of age (23%).
Severe outcomes—Canadian Immunization Research Network Severe Outcome Surveillance
A total of 30 influenza-associated hospitalizations were reported through the Canadian Immunization Research Network Severe Outcome Surveillance (CIRN-SOS) during the 2021–2022 influenza season. There were too few hospitalizations to analyze temporality or severity trends.
Viral characterization
From September 1, 2021 to August 27, 2022, the National Microbiology Laboratory (NML) characterized 277 influenza viruses, far fewer than during a typical influenza surveillance season (1,171 to 3,857 viruses from 2014–2015 to 2019–2020). All 277 influenza viruses were influenza A (266 A(H3N2), 11 A(H1N1)).
Of the 266 influenza A(H3N2) viruses genetically characterized, sequence analysis of the hemagglutinin gene indicated that 100% of these viruses belonged to genetic clade 3C.2a1b.2a.2.
A total of 277 influenza viruses were antigenically characterized (n=266 influenza A(H3N2) and 11 influenza A(H1N1)). Among these viruses, 19% of A(H3N2) viruses (n=51) were antigenically similar to the egg-propagated A(H3N2) reference virus used in the production of the 2021–2022 Northern Hemisphere influenza vaccine, while 91% of A(H1N1) viruses (n=10) were similar to the cell-propagated A(H1N1) reference virus.
Two-hundred and fifty-nine influenza viruses (246 A(H3N2) and 11 A(H1N1)) were tested for antiviral resistance, with 100% of viruses sensitive to each oseltamivir and zanamavir.
Vaccine monitoring—Vaccine coverage
Vaccine coverage for the 2021–2022 influenza season was similar to the previous season. Thirty percent of adults 18–64 years of age received their influenza vaccine. Vaccine coverage was higher among seniors aged 65 years and older (71%) and adults aged 18–64 years with chronic medical conditions (38%). Overall vaccine coverage was higher amongst females compared to males.
Vaccine monitoring—Vaccine effectiveness
Using a test-negative design, the Canadian Sentinel Practitioner Surveillance Network (SPSN) reports adjusted vaccine effectiveness (VE) of 36% (95% confidence interval [CI]: −38–71) against medically-attended illness due to late-season influenza A(H3N2) clade 3C.2a1b.2a.2 viruses Footnote 11. This estimate is adjusted for age group, province, comorbidity and calendar month, and is based on 327 specimens collected from week 10 to 26 (early-March to early-July 2022).
Given the low-intensity community circulation of influenza this season, estimates of seasonal influenza vaccine effectiveness in preventing hospitalization for laboratory-confirmed influenza are not available for the 2021–2022 season.
Discussion
The 2021–2022 Canadian influenza season saw the return of community influenza circulation. A national seasonal influenza epidemic was declared for the first time since the 2019–2020 season. Starting in mid-April and lasting only nine weeks, the 2021–2022 Canadian influenza season was later and shorter than usual and dominated by influenza A(H3N2).
The COVID-19 pandemic and response disrupted seasonal transmission patterns of influenza and other respiratory viruses. The NPIs put in place to address the COVID-19 pandemic, such as masking, border and travel measures and physical distancing, contributed to these disruptions. Associations between NPIs and decreased transmission of influenza and SARS-CoV-2 have been demonstrated Footnote 12 Footnote 13 Footnote 14 Footnote 15 Footnote 16. The aforementioned factors, as well as other factors such as antagonistic viral interference, which has been observed between influenza and other seasonal respiratory viruses Footnote 17 Footnote 18, may have contributed to the early-season suppression of influenza. The breadth of these factors continues to create uncertainty about the dynamics of influenza and SARS-CoV-2 co-circulation.
Seasonal influenza activity increased late in the season to reach the epidemic threshold at a time that corresponded to elevated SARS-CoV-2 transmission, demonstrating that community-level co-circulation of these viruses is possible. When influenza activity reached 5% of tests positive in Canada, the SARS-CoV-2 7-day average of test positivity was 17.6% and never dropped below 8.5% during the influenza epidemic (Figure 6). However, the 2021–2022 Canadian seasonal influenza epidemic peaked when SARS-CoV-2 percentage positivity was decreasing. Globally, peaks in influenza percentage positivity have thus far occurred at times when SARS-CoV-2 percentage positivity is relatively low or declining; a trend observed at some World Health Organization regional levels as well Footnote 19. Factors that modulate transmission of both viruses, such as viral interference, NPIs, vaccination, social mixing patterns and climatic conditions, require further study in combination to explain these trends.
There was evidence of influenza and SARS-CoV-2 co-circulation activity in ILI reports from FluWatchers. Reported ILI activity broadly aligned with SARS-CoV-2 laboratory activity, but the magnitude of the two indicators did not align precisely. Fluwatchers ILI activity increased but remained below expected levels during the most intense SARS-CoV-2 activity peak. The highest peak in FluWatchers ILI activity was later reported during a period of influenza and SARS-CoV-2 co-circulation. These findings highlight potential usefulness of FluWatchers for signal detection, but also highlight the lack of specificity of the case definition.
In Canada, the seasonal epidemic was driven by the spread of influenza A(H3N2). Influenza A(H3N2) case distribution tends to skew towards older adults, but this was not observed during the 2021–2022 season. The proportion of A(H3N2) infections detected among children and teenagers was nearly three times higher than typical, and hospitalization rates were similar among children aged 0–4 years and adults aged 65 years and older—atypical for a season dominated by A(H3N2). This unusual age distribution has a complex set of possible explanations, including more restrictive NPIs among vulnerable older adults differentially impacting influenza transmission in this group. Immunologic factors including increased susceptibility among the large cohort of young children unexposed to influenza infection may also play a role.
There was no evidence of increased severity of influenza cases among FluWatch indicators. The proportion of hospitalized cases admitted to ICU was either within or below expected levels. While a scarcity of documented cases has limited assessment, there was some early evidence of synergistic effects on severity of cases co-infected with influenza and SARS-CoV-2 Footnote 20 Footnote 21 Footnote 22 Footnote 23. FluWatch surveillance indicators are not well equipped to assess these effects.
Increased population-level influenza susceptibility was a concern coming into the 2021–2022 season. Several modelling studies demonstrated that pandemic-related conditions could cause greater seasonal influenza epidemic intensity, but that the complexity of transmission dynamics cause uncertainty in both the magnitude and timing Footnote 8 Footnote 24 Footnote 25. The 2021–2022 influenza epidemic highlighted this uncertainty, being late and low intensity. Influenza susceptibility remains higher than typical pre-pandemic years, and predisposition to larger influenza epidemics also remains Footnote 9; however, the likelihood of an intense influenza season is influenced by the ongoing COVID-19 pandemic and response, and population susceptibility to influenza cannot be considered in isolation.
With influenza susceptibility remaining high, the importance of seasonal influenza vaccination to reduce susceptibility is highlighted. The SPSN reported 36% VE against illness due to the influenza A(H3N2) clade 3C.2a1b.2a.2 viruses that predominated this season (95% CI: −38–71). These viruses are considered antigenically-distinct from the 2021–2022 vaccine strain instead belonging to clade 3C.2a1b.2a.1, but the estimate is very similar to VE estimates against influenza A(H3N2) recently reported from the United States (35%; 95% CI: 19–47) for the period spanning October 2021 to April 2022 Footnote 26 and from Europe (35%; 95% CI: 6–54) spanning October 2021 to March 2022 Footnote 27. Findings from SPSN, as well as strain characterization results from NML, reinforce the World Health Organization's decision to switch to a more representative clade 3C.2a1b.2a.2 strain for the northern hemisphere 2022–2023 A(H3N2) vaccine component Footnote 28.
Conclusion
The 2021–2022 Canadian influenza season was highlighted by the return of epidemic-level influenza activity. The 2021–2022 influenza epidemic was late, low-intensity and brief, and was influenced by the ongoing COVID-19 pandemic. Over the past two years, relatively few Canadians have been infected with influenza, rendering the population more susceptible to the seasonal influenza strains that are likely to circulate in the upcoming years. Ongoing circulation of SARS-CoV-2 creates great uncertainty regarding when an intense influenza epidemic may reoccur in Canada. Public health authorities need to remain vigilant and continue to plan for seasonal influenza circulation and to maintain laboratory diagnostics and surveillance capacity to help prevent the spread and impact of influenza. Influenza vaccination remains a key public health intervention available to protect Canadians.
Authors' statement
The FluWatch team in the Centre for Immunization and Respiratory Infectious Diseases developed the first draft collaboratively; all authors contributed to the conceptualization, writing and revision of the manuscript.
Competing interests
None.
Acknowledgements
Many thanks to all those across Canada who contribute to influenza surveillance. The FluWatch program consists of a volunteer network of labs, hospitals, doctors' offices, provincial and territorial ministries of health and individual Canadians who contribute as FluWatchers. We also acknowledge the following surveillance and research networks who contribute enhanced surveillance and knowledge exchange on influenza vaccine effectiveness to FluWatch: Canada's Immunization Monitoring Program ACTive, Canadian Immunization Research Network Serious Outcomes Surveillance Network, and the Canadian Influenza Sentinel Practitioner Surveillance Network. Finally, we wish to acknowledge the National Microbiology Laboratory's Influenza and Respiratory Virus section for the strain characterization and antiviral resistance testing data and the Centre for Immunization and Respiratory Infectious Diseases' Vaccination Coverage Section for their analysis of the annual national Seasonal Influenza Vaccination Coverage Surveys.
Funding
FluWatch surveillance is funded by the Public Health Agency of Canada.
References
- Footnote 1
-
Nwosu A, Lee L, Schmidt K, Buckrell S, Sevenhuysen C, Bancej C. National Influenza Annual Report, Canada, 2020-2021, in the global context. Can Commun Dis Rep 2021;47(10):405–13. https://doi.org/10.14745/ccdr.v47i10a02
- Footnote 2
-
Groves HE, Piché-Renaud PP, Peci A, Farrar DS, Buckrell S, Bancej C, Sevenhuysen C, Campigotto A, Gubbay JB, Morris SK. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. Lancet Reg Health Am 2021;1:100015. https://doi.org/10.1016/j.lana.2021.100015
- Footnote 3
-
Groves HE, Papenburg J, Mehta K, Bettinger JA, Sadarangani M, Halperin SA, Morris SK; for members of the Canadian Immunization Monitoring Program Active (IMPACT). The effect of the COVID-19 pandemic on influenza-related hospitalization, intensive care admission and mortality in children in Canada: A population-based study. Lancet Reg Health Am 2022;7:100132. https://doi.org/10.1016/j.lana.2021.100132
- Footnote 4
-
Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, Cohen C, Fry AM. Decreased Influenza Activity During the COVID-19 Pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 2020;69(37):1305–9. http://dx.doi.org/10.15585/mmwr.mm6937a6
- Footnote 5
-
Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, Kok J, Macartney K, MacLachlan J, Minney-Smith C, Smith D, Stocks N, Taylor J, Barr IG. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill 2020;25(47):2001847. https://doi.org/10.2807/1560-7917.ES.2020.25.47.2001847
- Footnote 6
-
Tang JW, Bialasiewicz S, Dwyer DE, Dilcher M, Tellier R, Taylor J, Hua H, Jennings L, Kok J, Levy A, Smith D, Barr IG, Sullivan SG. Where have all the viruses gone? Disappearance of seasonal respiratory viruses during the COVID-19 pandemic. J Med Virol 2021;93(7):4099–101. https://doi.org/10.1002/jmv.26964
- Footnote 7
-
World Health Organization. Karlsson EA, Mook PAN, Vandemaele K, Fitzner J, Hammond A, Cozza V, Zhang W, Moen A. Review of global influenza circulation, late 2019 to 2020, and the impact of the COVID-19 pandemic on influenza circulation. Weekly epidemiological record No 25, 2021, 96, 241-4. Geneva (CH): WHO; 2021. https://apps.who.int/iris/bitstream/handle/10665/341994/WER9625-eng-fre.pdf
- Footnote 8
-
Baker RE, Park SW, Yang W, Vecchi GA, Metcalf CJE, Grenfell BT. The impact of COVID-19 nonpharmaceutical interventions on the future dynamics of endemic infections. Proc Natl Acad Sci USA 2020;117(48):30547–53. https://doi.org/10.1073/pnas.2013182117
- Footnote 9
-
Woolthuis RG, Wallinga J, van Boven M. Variation in loss of immunity shapes influenza epidemics and the impact of vaccination. BMC Infect Dis 2017;17(1):632. https://doi.org/10.1186/s12879-017-2716-y
- Footnote 10
-
Public Health Agency of Canada. COVID-19 epidemiology update. Ottawa, ON: PHAC; 2022. https://health-infobase.canada.ca/covid-19/
- Footnote 11
-
Kim S, Chuang ESY, Sabaiduc S, Olsha R, Kaweski SE, Zelyas N, Gubbay JB, Jassem AN, Charest H, De Serres G, Dickinson JA, Skowronski DM. Influenza vaccine effectiveness against A(H3N2) during the delayed 2021/22 epidemic in Canada. Euro Surveill 2022;27(38). https://doi.org/10.2807/1560-7917.ES.2022.27.38.2200720
- Footnote 12
-
Lagacé-Wiens P, Sevenhuysen C, Lee L, Nwosu A, Smith T. Impact of nonpharmaceutical interventions on laboratory detections of influenza A and B in Canada. Can Commun Dis Rep 2021;47(3):142–8. https://doi.org/10.14745/ccdr.v47i03a04
- Footnote 13
-
Qiu Z, Cao Z, Zou M, Tang K, Zhang C, Tang J, Zeng J, Wang Y, Sun Q, Wang D, Du X. The effectiveness of governmental nonpharmaceutical interventions against COVID-19 at controlling seasonal influenza transmission: an ecological study. BMC Infect Dis 2022;22(1):331. https://doi.org/10.1186/s12879-022-07317-2
- Footnote 14
-
Han S, Zhang T, Lyu Y, Lai S, Dai P, Zheng J, Yang W, Zhou X-H, Feng L. Influenza's plummeting during the COVID-19 pandemic: The roles of mask-wearing, mobility change, and SARS-CoV-2 interference. Engineering (Beijing) 2022 Feb 2. https://doi.org/10.1016/j.eng.2021.12.011
- Footnote 15
-
Brown KA, Soucy J-PR, Buchan SA, Sturrock SL, Berry I, Stall NM, Jüni P, Ghasemi A, Gibb N, MacFadden DR, Daneman N. The mobility gap: estimating mobility thresholds required to control SARS-CoV-2 in Canada. CMAJ 2021;193(17):E592–600. https://doi.org/10.1503/cmaj.210132
- Footnote 16
-
Nouvellet P, Bhatia S, Cori A, Ainslie KEC, Baguelin M, Bhatt S, Boonyasiri A, Brazeau NF, Cattarino L, Cooper LV, Coupland H, Cucunuba ZM, Cuomo-Dannenburg G, Dighe A, Djaafara BA, Dorigatti I, Eales OD, van Elsland SL, Nascimento FF, FitzJohn RG, Gaythorpe KAM, Geidelberg L, Green WD, Hamlet A, Hauck K, Hinsley W, Imai N, Jeffrey B, Knock E, Laydon DJ, Lees JA, Mangal T, Mellan TA, Nedjati-Gilani G, Parag KV, Pons-Salort M, Ragonnet-Cronin M, Riley S, Unwin HJT, Verity R, Vollmer MAC, Volz E, Walker PGT, Walters CE, Wang H, Watson OJ, Whittaker C, Whittles LK, Xi X, Ferguson NM, Donnelly CA. Reduction in mobility and COVID-19 transmission. Nat Commun 2021;12(1):1090. https://doi.org/10.1038/s41467-021-21358-2
- Footnote 17
-
Nickbakhsh S, Mair C, Matthews L, Reeve R, Johnson PCD, Thorburn F, von Wissmann B, Reynolds A, McMenamin J, Gunson RN, Murcia PR. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc Natl Acad Sci U S A 2019;116(52):27142–50. https://doi.org/10.1073/pnas.1911083116
- Footnote 18
-
Piret J, Boivin G. Viral Interference between Respiratory Viruses. Emerg Infect Dis 2022;28(2):273–81. https://doi.org/10.3201/eid2802.211727
- Footnote 19
-
World Health Organization. Global Influenza Programme. Influenza Update N° 425. Geneva, CH: WHO; 2022. https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring/influenza-updates/current-influenza-update
- Footnote 20
-
Stowe J, Tessier E, Zhao H, Guy R, Muller-Pebody B, Zambon M, Andrews N, Ramsay M, Lopez Bernal J. Interactions between SARS-CoV-2 and influenza, and the impact of coinfection on disease severity: a test-negative design. Int J Epidemiol 2021;50(4):1124–33. https://doi.org/10.1093/ije/dyab081
- Footnote 21
-
Zheng J, Chen F, Wu K, Wang J, Li F, Huang S, Lu J, Huang J, Liu H, Zhou R, Huang Z, Meng B, Yuan Z, Wu X. Clinical and virological impact of single and dual infections with influenza A (H1N1) and SARS-CoV-2 in adult inpatients. PLoS Negl Trop Dis 2021;15(11):e0009997. https://doi.org/10.1371/journal.pntd.0009997
- Footnote 22
-
Dao TL, Hoang VT, Colson P, Million M, Gautret P. Co-infection of SARS-CoV-2 and influenza viruses: A systematic review and meta-analysis. J Clin Virol Plus 2021;1(3):100036. https://doi.org/10.1016/j.jcvp.2021.100036
- Footnote 23
-
Santos CAD, Bezerra GVB, Marinho ARRAA, Sena LOC, Menezes VJ, Teixeira DCP, Souza MF, Góes MAO, Martins-Filho PR. SARS-CoV-2/influenza A (H3N2) virus coinfection: epidemiological surveillance in Northeast Brazil. Rev Soc Bras Med Trop 2022;55:e0132. https://doi.org/10.1590/0037-8682-0132-2022
- Footnote 24
-
Lee K, Jalal H, Raviotta JM, Krauland MG, Zimmerman RK, Burke DS, Roberts MS. Estimating the Impact of Low Influenza Activity in 2020 on Population Immunity and Future Influenza Seasons in the United States. Open Forum Infect Dis 2021;9(1):ofab607. https://doi.org/10.1093/ofid/ofab607
- Footnote 25
-
Krauland MG, Galloway DD, Raviotta JM, Zimmerman RK, Roberts MS. Impact of Low Rates of Influenza on Next-Season Influenza Infections. Am J Prev Med 2022;62(4):503–10. https://doi.org/10.1016/j.amepre.2021.11.007
- Footnote 26
-
Centers for Disease Control and Prevention (CDC). Interim US flu vaccine effectiveness (VE) data for 2021–2022. Atlanta, GA: CDC; (accessed 2022-09-06). https://www.cdc.gov/flu/vaccines-work/2021-2022.html
- Footnote 27
-
Santé publique France. Grippe. Bilan préliminaire de l'épidémie de grippe 2021-22. [Influenza. Preliminary assessment of the 2021/22 influenza epidemic.] Saint-Maurice: Santé publique France; 2022. French. https://www.santepubliquefrance.fr/content/download/440665/document_file/Bulletin_grippe_bilan_21-22.pdf
- Footnote 28
-
World Health Organization (WHO). Recommendations for influenza vaccine composition; 2022; (accessed 2022-09-20). https://www.who.int/teams/global-influenza-programme/vaccines/who-recommendations
