Original quantitative research – Surveillance from the high ground: sentinel surveillance of injuries and poisonings associated with cannabis
Health Promotion and Chronic Disease Prevention in Canada
André S. Champagne, MPH; Steven R. McFaull, MSc; Wendy Thompson, MSc; Felix Bang, MPH
https://doi.org/10.24095/hpcdp.40.5/6.07
This article has been peer reviewed.
Author reference
Public Health Agency of Canada, Ottawa, Ontario, Canada
Correspondence: André Champagne, Centre for Surveillance and Applied Research, Public Health Agency of Canada, 785 Carling Avenue, Ottawa, ON K1A 0K9; Tel: 613-296-3654; Email: andre.champagne@canada.ca
Abstract
Introduction: In October 2018, Canada legalized the nonmedical use of cannabis for adults. The aim of our study was to present a more recent temporal pattern of cannabis-related injuries and poisonings found in the electronic Canadian Hospitals Injury Reporting and Prevention Program (eCHIRPP) database and provide a descriptive summary of the injury characteristics of cannabis-related cases captured in a nine-year period.
Methods: We conducted a search for cannabis-related cases in the eCHIRPP database reported between April 2011 and August 2019. The study population consisted of patients between the ages of 0 and 79 years presenting to the 19 selected emergency departments across Canada participating in the eCHIRPP program. We calculated descriptive estimates examining the intentionality, external cause, type and severity of cannabis-related cases to better understand the contextual factors of such cases. We also conducted time trend analyses using Joinpoint software establishing the directionality of cannabis-related cases over the years among both children and adults.
Results: Between 1 April, 2011, and 9 August, 2019, there were 2823 cannabis-related cases reported in eCHIRPP, representing 252.3 cases/100 000 eCHIRPP cases. Of the 2823 cannabis-related cases, a majority involved cannabis use in combination with one or more substances (63.1%; 1780 cases). There were 885 (31.3%) cases that involved only cannabis, and 158 cases (5.6%) that related to cannabis edibles. The leading external cause of injury among children and adults was poisoning. A large proportion of cannabis-related cases were unintentional in nature, and time trend analyses revealed that cannabis-related cases have recently been increasing among both children and adults. Overall, 15.1% of cases involved serious injuries requiring admission to hospital.
Conclusion: Cannabis-related cases in the eCHIRPP database are relatively rare, a finding that may point to the fact that mental and behavioural disorders resulting from cannabis exposure are not generally captured in this surveillance system and the limited number of sites found across Canada. With Canada’s recent amendments to cannabis regulations, ongoing surveillance of the health impacts of cannabis will be imperative to help advance evidence to protect the health of Canadians.
Keywords: cannabis, eCHIRPP, legalization, edibles, injuries, poisonings, Canada
Highlights
- Between 1 April, 2011, and 9 August, 2019, there were 2823 cannabis-related cases reported in the electronic Canadian Hospitals Injury Reporting and Prevention Program (eCHIRPP), representing 252.3 cases/100 000 eCHIRPP cases.
- Males have consistently represented a higher proportion of cases across all age groups, with the exception of the group aged 10 to 14 years, in which females represented a slightly larger proportion.
- Of the 2823 cases, 158 cases (5.6%) involved cannabis edibles.
- Significant increases in annual percent change (APC) in cannabis-related cases were identified across every group in recent years: among adults, a 27.9% APC was noted between 2013 and 2018; among children, a 35.6% APC was noted between 2016 and 2018; and overall, a 30.1% APC was noted between 2015 and 2018.
- The leading external cause of injury across all groups was poisoning.
Introduction
In October 2018, Canada became the second country in the world to legalize the nonmedical use of cannabis for adults, nearly two decades following its 2001 Marihuana Medical Access Regulations. At the national level, cannabis use has become increasingly prevalent in recent decades. For example, between 2004 and 2017, past-year use of cannabis among the Canadian household population aged 15 years or over increased from 9.4% to 14.8%.Footnote 1 Recent post-legalization national figures also show an increase in cannabis use for the same population: a comparison of first quarter estimates from 2018 and 2019 reveal a 29% increase in past-three-month use (from 14% to 18%).Footnote 1 In this short time period, a significant increase in cannabis use was noted among males between the ages of 18 and 64 years,Footnote 1 and the number of new users nearly doubled among both sexes (from 327 000–646 000).Footnote 2
Conversely, among youth, a decrease in cannabis use has been observed in the past decade. Between 2008/09 and 2014/15, past-year cannabis use decreased from 27.3% to 16.5% among youth in Grades 7 through 12.Footnote 3 More recent findings from 2016/17 and 2018/19, however, show that past-year cannabis consumption among this group has remained unchanged from 2014/15, at 18.1%.Footnote 4Footnote 5 Significant changes in the risk perception of this substance were also noted within this time period, suggesting a decreasing trend in the viewing of cannabis as a harmful substance: whereas in 2014/15, 7% of respondents reported that regular cannabis use posed “no risk,” in 2016/17, this percentage was up to 9%.Footnote 4Footnote 6 Further, when asked if people were at “great risk” of harming themselves when using cannabis on a regular basis, a statistically significant decrease was noted (58%–54%).Footnote 4 Such perception changes among this population are of concern, considering the findings of a recent pan-Canadian study by the Canadian Institute for Health Information (CIHI) showing that, of the 23 580 hospitalizations for harm caused by substance use among youth aged 10 to 24 years in 2017 to 2018, those related to cannabis were more common (38.5%) than those caused by any other substance, including alcohol, opioids and cocaine.Footnote 7 Moreover, this report noted that 81% of the cannabis-related hospitalizations involved a concurrent mental health condition.
The degree to which cannabis can affect the health of populations has also been examined in epidemiological studies. An area of research that has gained much attention is the ways in which cannabis consumption affects the operation of motor vehicles. Simulated driving experiments, for instance, following acute cannabis consumption have found that cognitive functions required to safely operate vehicles may become affected, resulting in greater risk of vehicle collisions.Footnote 8Footnote 9 These effects have also been found among regular cannabis users participating in such driving-simulation studies.Footnote 9 Observational studies have also found significant associations between acute cannabis intoxication and motor vehicle collisions,Footnote 10 including those resulting in fatalities.Footnote 11Footnote 12 As might be expected, preventing “drugged driving” has become a priority for governments and law enforcement in Canada.Footnote 13 At the federal level, for instance, the government of Canada launched the Don’t Drive High campaign in 2017, a widespread public safety initiative reaching Canadians through media platforms including television, cinema and popular social media applications.Footnote 14
Medical studies highlighting clinical presentations of acute ingestions of cannabis among children and adults have also been undertaken in an effort to better inform medical practitioners. These studies have documented pediatric patients presenting with decreased levels of consciousness, confusion, anxiety, ataxia and respiratory distress as a result of cannabis exposure.Footnote 15Footnote 16Footnote 17 Among adults, a Colorado-based study examining emergency department (ED) visits found that gastrointestinal ailments, intoxication and psychiatric symptoms were the most common medical conditions associated with inhaled cannabis–related visits.Footnote 18
With Canada’s recent amendments to cannabis regulations and the noted changes in trends in prevalence and the perceptions of this substance, the need for the ongoing surveillance of the health impacts of cannabis is evident. Expanding on Rao’s 2018 study,Footnote 19 the aim of our study was to present a more recent temporal pattern of cannabis-related injuries and poisonings found in the electronic Canadian Hospitals Injury Reporting and Prevention Program (eCHIRPP) database and provide a descriptive summary of the injury characteristics of cannabis-related cases captured since 1 April, 2011. Specifically, this study (1) analyzed three additional years of cannabis-related data using a similar methodology in eCHIRPP; (2) examined the factors involved in cases where edible cannabis products were consumed; and (3) established a baseline for future cannabis-related studies using the eCHIRPP database.
Methods
Data source
The eCHIRPP is a sentinel surveillance system that gathers injury and poisoning data from 19 selected EDs across Canada, 11 of which are primarily pediatric hospitals; the remaining hospitals serve both the child and adult populations. As a result, the eCHIRPP database contains a larger proportion of injuries and poisonings involving children. The program was designed to help researchers better understand the ways in which injuries and poisonings occur by obtaining a narrative description from patients, caregivers and/or onsite eCHIRPP personnel. In these narratives, questions addressing how, where and why the injuries occurred are generally answered. Additional information is also entered in reports by health care providers and eCHIRPP coders, who provide clinical and contextual data that include the presence of substance use, the region(s) of the body affected by the injuries, the location (e.g. home, public space) in which the injuries occurred, and the nature and external causes of the injuries. The capture of contextual factors by the eCHIRPP sentinel surveillance system makes it an important resource in the realm of injury prevention. Indeed, for nearly 30 years, data from the CHIRPP program have contributed to injury research by informing timely epidemiological reports and studies conducted in academic and organizational settings on a range of topics including fractures,Footnote 20Footnote 21 injuries as a result of products or equipmentFootnote 22Footnote 23 and sports-related injuries.Footnote 24Footnote 25
Data extraction
On 9 August, 2019, we conducted an extraction of all eCHIRPP records that had been entered into the system since 1 April, 2011 (total = 1 118 930), thus covering a nine-year time period.
Age groups
We conducted descriptive analyses by examining injuries and poisonings across three groups: children (aged 17 years or younger), adults (18 years and over) and all individuals combined. To present greater granularity of the data, we also conducted further analyses examining smaller age group ranges, though such groups were not the principal focus of this study.
Case identification
To identify all cannabis-related cases, we examined three variables in the eCHIRPP records: substance use, substance ID and the narrative description of the injury. The substance use code was the primary variable used to identify cannabis-related cases. We screened all records in which the substance use field indicated “yes” or was left blank by searching key words pertaining to cannabis in the narrative description and substance ID fields. Subsequently, accounting for human coding error, we conducted a similar process for records in which the substance use field indicated “no.”
Injury characteristics
In parallel with Rao’s 2018 study,Footnote 19 we grouped injury characteristics into four broad categories examining the intentionality, external cause, type and severity of all cannabis-related cases. Table 1 shows the eCHIRPP codes used in the analyses, along with their descriptions.
Table 1. Cannabis-related injury characteristics and codes, eCHIRPP, 2011 to 2019
| Injury characteristic | Description | eCHIRPP codes | Rationale for inclusion in analysis |
|---|---|---|---|
| Intent of the injury or poisoning | Unintentional injury | 10IN, 16IN | To examine the intentional nature of the injury or poisoning event. Key word search terms were also used for classification. |
| Physical assault and/or aggression | 15IN | ||
| Self-harm | 11IN | ||
| Involvement of emergency response personnel (ERP) | 19IN | ||
| Sexual assault | 12IN | ||
| Maltreatment | 13IN, 14IN | ||
| External cause | Poisoning | 210EC, 301EC | To examine the mechanism of the injury or poisoning. Key word search terms were also used for classification. |
| Fall | 201EC, 2011EC | ||
| Assault | 400EC, 4001EC | ||
| Transport | 100EC, 101EC, 102EC | ||
| External agent | 202EC, 203EC, 205EC, 209EC, 302EC, 305EC, 309EC | ||
| Nature of injury | Intoxication | 50NI | To examine the type of injuries sustained. Key word search terms were also used for classification. |
| External wound | 10NI, 11NI | ||
| Internal wound | 24NI, 25NI, 26NI, 27NI, 52NI, 53NI, 60NI, 77NI | ||
| Brain injury | 41NI, 42NI, 43NI | ||
| Fracture, sprain, or strain (or key terms) | 12NI, 13NI, 14NI, 15NI, 16NI, 17NI, 75NI | ||
| Severity | Severe | 700T, 800T, 900T | The severity of the injuries or poisonings was dichotomized based on treatment outcomes. Patients admitted in hospitals or pronounced dead in emergency departments were deemed as severe, whereas patients requiring treatment or observational care in the emergency departments were deemed as not severe. |
| Not severe | 100T, 200T, 300T, 400T, 500T, 600T | ||
Statistical analyses
Estimates of identified cannabis-related cases relative to all cases found in the database are presented as proportions relative to 100 000 eCHIRPP records. The proportions of the injury characteristics we examined are relative to all cannabis-related cases. We performed time trend analyses across three groups—children, adults and all ages—covering an eight-year period using Joinpoint (Version 4.6.0.0),Footnote 26 This software detects inflection points, calculates whether annual percent changes (APC) of segments are significantly different from zero (alpha = 0.05), and provides 95% confidence intervals. In our study, time trend analyses were based on the proportion of cannabis-related cases relative to all cases found in eCHIRPP according to the given groups.
Results
Between 1 April, 2011, and 9 August, 2019, there were 2823 cannabis-related cases reported in eCHIRPP, representing 252.3 cases/100 000 eCHIRPP cases. Of the 2823 cannabis-related cases, a majority involved cannabis use in combination with one or more substances (63.1%; 1780 cases). There were 885 (31.3%) cases that involved only cannabis, and 158 cases (5.6%) that related to cannabis edibles. Excluding cases involving cannabis edibles, males represented the largest proportion (compared to females) at 60.9% (n = 1623). Conversely, among those involving edibles, females represented the largest proportion at 53.2% (n = 84), as shown in Table 2.
Table 2. Number of cannabis-related cases by age group and sex, eCHIRPP, 2011 to 2019
| Category | Total (column%) | Males (%) | Females (%) |
|---|---|---|---|
| Edibles | 158 (5.6%) | 74 (46.9) | 84 (53.2) |
| Cannabis alone | 884 (31.3%) | 549 (62.1) | 335 (37.9) |
| Polysubstance use | 1780 (63.1%) | 1074 (60.3) | 706 (39.7) |
| All casesFootnote a of Table 2 | 2822 | 1697 (60.1) | 1125 (39.9) |
| Age groupsFootnote b of Table 2 | |||
| Children (17 years or younger) | 1914 (67.8%) | 1001 (52.3) | 913 (47.7) |
| Adults (18 years or older) | 907 (32.2%) | 696 (76.7) | 211 (23.3) |
| Under 10 yrs | 97 | 50 (51.6) | 47 (48.4) |
| 10 to 14 yrs | 477 | 237 (49.7) | 240 (50.3) |
| 15 to 19 yrs | 1457 | 800 (54.9) | 657 (45.1) |
| 20 to 29 yrs | 383 | 307 (80.2) | 76 (19.8) |
| 30 to 39 yrs | 205 | 156 (76.1) | 49 (23.9) |
| 40 to 49 yrs | 99 | 70 (70.7) | 29 (29.3) |
| 50 to 64 yrs | 91 | 68 (74.7) | 23 (25.3) |
| 65 yrs and older | 12 | 9 (75.0) | 3 (25.0) |
Table 2 also summarizes the results for both sexes across eight different age groups. Males consistently accounted for a higher proportion of all cannabis-related cases across the majority of age groups, with the exception of the group aged 10 to 14 years, in which females represented a slightly larger proportion compared to males (50.3% vs. 49.7%). When comparing children (aged 17 years and younger) and adults, the former accounted for the largest proportion of all cannabis-related cases at 67.8%, representing 1914 cases or 210.4 cases/100 000 eCHIRPP cases. Adults accounted for 907 cannabis-related cases, or 32.2%; however, in relation to all eCHIRPP records, the proportion was higher among this group compared to children, at 434.6 cases/100 000 eCHIRPP cases.
With respect to temporal patterns, we conducted time trend analyses examining the three groups—children, adults and overall cases. Of note, these analyses only included cases related to cannabis and cannabis edibles up to the end of the 2018 calendar year and not 2019, accommodating the varying entry time for eCHIRPP records. As shown in Figure 1, significant increases in annual percent change (APC) in all cannabis-related cases were detected in the Joinpoint software across every group in recent years: among adults, a 27.9% APC was noted between 2013 and 2018; among children, a 35.6% APC was noted between 2016 and 2018; and overall, there was a 30.1% APC between 2015 and 2018. We also noted a significant increase in APC (26.0%, CI: 6.0%–49.8%) between 2011 and 2018 when examining overall cases related to cannabis edibles, though caution should be taken when interpreting this result, given the low number of these cases (Figure 1).
Figure 1. Time trend of cannabis-related cases presenting to emergency departments, children, adults and overall cases, eCHIRPP, 2011 to 2018Figure 1 footnote a
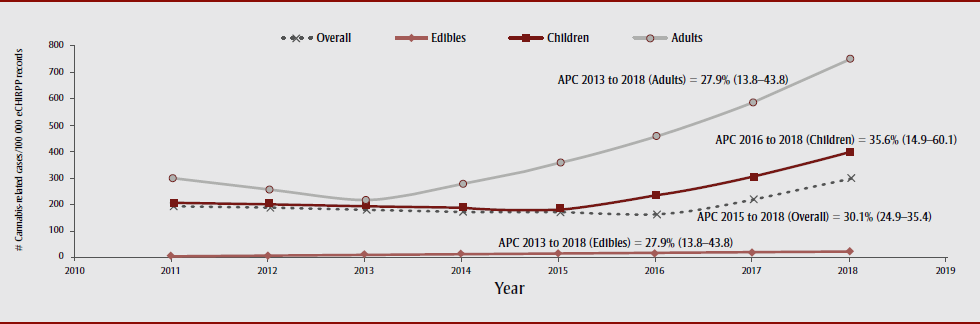
Text description: Figure 1
Figure 1. Time trend of cannabis-related cases presenting to emergency departments, children, adults and overall cases, eCHIRPP, 2011 to 2018Figure 1 footnote a
| Year | # of cannabis-related cases/100 000 eCHIRPP records | |||
|---|---|---|---|---|
| Overall | Edibles | Children | Adults | |
| 2011 | 194.92 | 4.83 | 208.37 | 300.18 |
| 2012 | 188.17 | 6.09 | 201.38 | 256.35 |
| 2013 | 181.66 | 7.67 | 194.64 | 218.91 |
| 2014 | 175.37 | 9.66 | 188.11 | 279.99 |
| 2015 | 169.30 | 12.18 | 181.81 | 358.11 |
| 2016 | 163.44 | 15.34 | 236.45 | 458.03 |
| 2017 | 221.64 | 19.33 | 307.51 | 585.83 |
| 2018 | 300.56 | 24.36 | 399.92 | 749.28 |
| APC | 2015 to 2018: 30.1% (24.9, 35.4) | 2013 to 2018: 27.9% (13.8,43.8) | 2016 to 2018: 35.6% (14.9, 60.1) | 2013 to 2018: 27.9% (13.8, 43.8) |
When examining the intentionality of the cannabis-related cases, we identified similar patterns among children and adults. As shown in Figure 2, the majority of all cannabis-related cases were unintentional in nature (e.g. poisonings, falls and motor vehicle collisions) among both groups (children 66.3%, adults 58.2%), followed by those caused by self-harm (e.g. suicidal ideations and attempts; children 15.7%, adults 19.8%) and physical assault/aggression (e.g. physical altercations or striking of inanimate objects; children 9.7%, adults 16.9%). Of the 481 self-harm cases, 62.4% involved children (n = 300), with a median age of 16 years, and the remaining 37.6% (n = 181) involved adults, with a median age of 30 years. As for the degree of severity among self-harm cannabis-related cases, 29.3% of children and 18.3% of adults were admitted to hospitals (data not shown). Representing the smallest proportions in this category were cases involving Emergency Response Personnel (ERP) and those related to sexual assault and other maltreatment. Cases involving ERP (children 7.4%; adults 4.0%) included situations in which patients were unresponsive or disorderly in public. Sexual assault–related cases (children 0.7%; adults 0.2%) included situations in which patients were touched or forced into intercourse. Of note, all sexual assault–related cases involved the presence of other substances in addition to cannabis, including alcohol, ecstasy and cocaine. Lastly, maltreatment cases (children 0.3%; adults 1.0%) included circumstances related to intimate partner violence as well as abuse by family members.
Figure 2. Distribution of intent categories among cannabis-related injury cases in eCHIRPP, 2011 to 2019Figure 2 footnote a
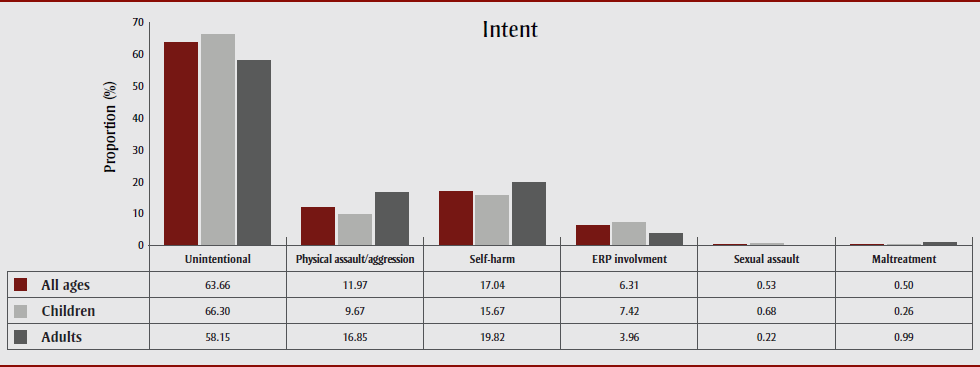
Text description: Figure 2
Figure 2. Distribution of intent categories among cannabis-related injury cases in eCHIRPP, 2011 to 2019Figure 2 footnote a
| Intent Categories | Proportion (%) | ||
|---|---|---|---|
| All ages | Children | Adults | |
| Unintentional | 63.66 | 66.30 | 58.15 |
| Physical assault/aggression | 11.97 | 9.67 | 16.85 |
| Self-harm | 17.04 | 15.67 | 19.82 |
| ERP involvement | 6.31 | 7.42 | 3.96 |
| Sexual assault | 0.53 | 0.68 | 0.22 |
| Maltreatment | 0.50 | 0.26 | 0.99 |
The leading external cause across all three groups was poisoning, as shown in Figure 3. Cases captured in this category included those with adverse reactions to cannabis use, but also included incidents in which cannabis was involved in conjunction with other substances including alcohol, cocaine and methamphetamine. Whereas falls and transport-related injuries represented the second and third most frequent external causes among adults, at 18.9% and 17.6%, respectively, assaults and external agent–related injuries were the second and third most frequent external causes among children, at 6.6% and 6.2%, respectively. The external agent category captured both intentional and unintentional cases in which external agents were factors contributing to the injuries—these agents included objects such as windows, knives and items of furniture.
Figure 3. Distribution of external cause among cannabis-related injury cases in the eCHIRPP, 2011 to 2019Figure 3 footnote a
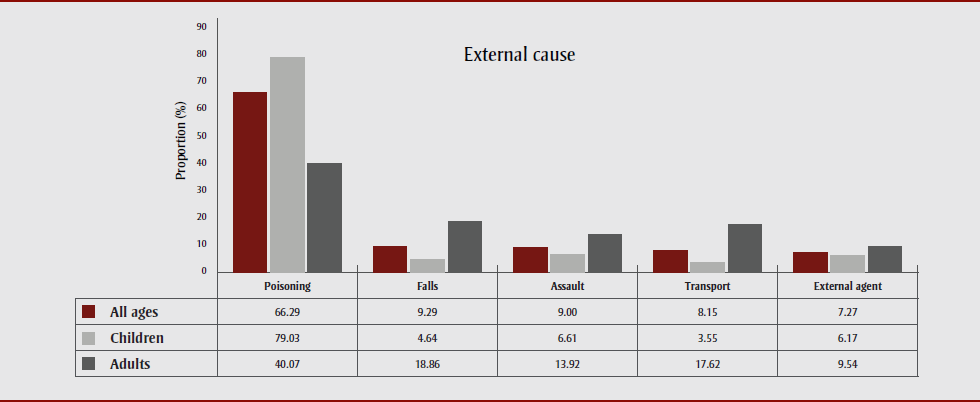
Text description: Figure 3
Figure 3. Distribution of external cause among cannabis-related injury cases in the eCHIRPP, 2011 to 2019Figure 3 footnote a
| External Cause | Proportion (%) | ||
|---|---|---|---|
| All ages | Children | Adults | |
| Poisoning | 66.29 | 79.03 | 40.07 |
| Falls | 9.29 | 4.64 | 18.86 |
| Assault | 9.00 | 6.61 | 13.92 |
| Transport | 8.15 | 3.55 | 17.62 |
| External agent | 7.27 | 6.17 | 9.54 |
With respect to the nature of the injuries or poisonings reported, Figure 4 shows that an overwhelmingly large proportion of cases (84.6%) involved intoxication among children. In this category, the median age was 16 years, and cases included children suffering adverse effects of cannabis alone or in conjunction with other substances. The second most common type of injury among children was external wounds, representing 7.7% of cases. Here, cases included falls, altercations and motor vehicle collisions. Among adults, we identified a similar pattern, in which intoxication (42.5%) was most common (median age of 29 years). As shown in Figure 4, the external wounds (20.7%) and fracture, sprain or strain (20.2%) categories were the second and third most frequent types of injuries sustained.
Figure 4. Distribution of nature of injury among cannabis-related cases in the eCHIRPP, 2011 to 2019Figure 4 footnote a
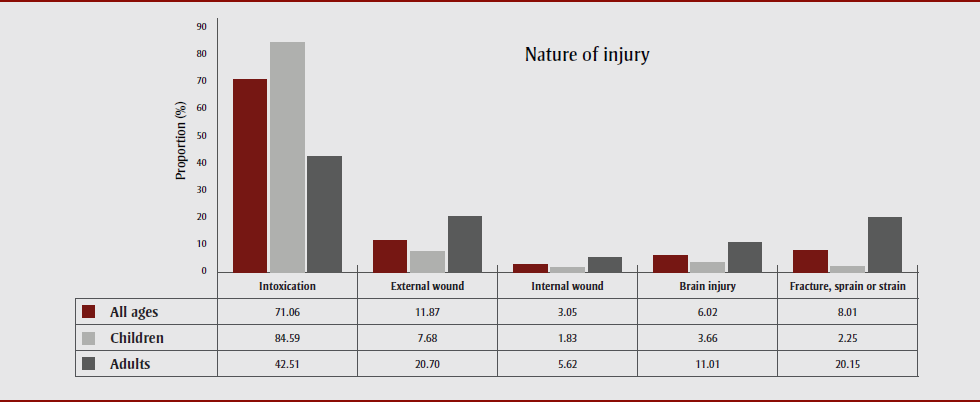
Text description: Figure 4
Figure 4. Distribution of nature of injury among cannabis-related cases in the eCHIRPP, 2011 to 2019Figure 4 footnote a
| Nature of Injury | Proportion (%) | ||
|---|---|---|---|
| All ages | Children | Adults | |
| Intoxication | 71.06 | 84.59 | 42.51 |
| External Wound | 11.87 | 7.68 | 20.70 |
| Internal Wound | 3.05 | 1.83 | 5.62 |
| Brain injury | 6.02 | 3.66 | 11.01 |
| Fracture, sprain or strain | 8.01 | 2.25 | 20.15 |
With respect to the severity of all cannabis-related cases, 15.1% of cases involved serious injuries requiring admission to hospital. Of these cases, 238 (56%) involved children, with an overall median age of 16 years, and a higher proportion of males (52.2%; data not shown). In this category of serious injuries involving children, suicide attempts, motor vehicle collisions and polysubstance use were contributing factors. Among adults, there were 187 cases requiring admission to hospital, of which 81.8% involved males (data not shown). Factors contributing to these cases among adults were similar to those involving children, and included assaults, suicide attempts and motor vehicle collisions. Notably, only one death was identified in this study; polysubstance use and a motor vehicle collision were the factors involved.
Lastly, because edible cannabis products were legalized in Canada in October 2019, this study examined cases in which such products were involved. Of the 158 cases identified, a significantly large proportion involved children (87.3%), among whom females represented a slightly higher proportion than males, at 56.5%. Here, symptoms included dizziness, drowsiness and emesis. Among children under the age of 10 years, there were 35 cases, all of which were unintentional in nature and two of which were admitted to hospital. Based on these narratives, these edible products were either mistakenly left within the reach of children or unintentionally given to them. Among the 20 cases in adults, 14 cases involved males (70%). Among this group, symptoms included anxiety, disorientation and emesis.
Discussion
This study demonstrated that cannabis-related injury and poisoning cases are relatively rare in the eCHIRPP database. A possible explanation for this finding may be supplied by the CIHI study mentioned earlier,Footnote 7 which found that the majority of cannabis-related hospitalizations can be attributed to concurrent mental health conditions—conditions that may not be captured in the eCHIRPP database.
Our study’s findings, however, are consistent with other studies examining US data from poison centres and EDs, which show that males generally represent the largest proportion of cannabis-related cases presenting there.Footnote 27Footnote 28 In Canada, the higher proportion of cannabis-related cases involving males may be in part a reflection of patterns of cannabis use; both past and recent national statistics have shown that the prevalence of cannabis use among Canadians aged 15 years or older is statistically higher among males.Footnote 1Footnote 29 Further, recent national figures for Canadians aged 15 years and older have shown that daily or almost daily use of cannabis was significantly higher among males compared to females, at 7.6% versus 4.5%, respectively.Footnote 2
Time trend analyses showed increases in APC regarding the proportion of cannabis-related cases in eCHIRPP among both children and adults in some years during the study period. While the recent increase in the prevalence of cannabis use among the adult population may help explain such a pattern, the noted decreasing prevalence of cannabis use among youth suggests otherwise. However, despite these trends, cannabis use among the younger population still remains higher in proportion compared to adults,Footnote 1 which points to their higher degree of exposure. It is possible that the large amount of media coverage and discussion surrounding cannabis in the years leading up to the 2018 legalization may have resulted in individuals being less reluctant to disclose cannabis use when presenting to EDs, thereby apparently increasing the overall number of cannabis-related cases.
A large majority of cases among children and adults presenting to the ED were unintentional in nature; patients were simply experiencing the adverse effects of cannabis. Of concern are the ways in which such unintentional cannabis-related exposures can affect younger children. Indeed, a systematic review examining the health effects of unintentional cannabis exposure concluded that when children present to EDs with lethargy and ataxia, clinicians should suspect cannabis toxicity.Footnote 30 The 35 cases in our study that involved the unintentional ingestion of cannabis products among those under 10 years of age also reinforce the need for safer practices in individual households, mainly the safer storage of such products. Child-resistant, plain packaging and THC limits are examples of other measures that have been considered to prevent such events.Footnote 31 And though much warranted attention is focussed on edibles, there are other hidden hazards that parents and caregivers need to be mindful of when children are present, including cannabis resin and joints.Footnote 30
From a public health perspective, transportation-related incidents captured in this study not only speak to the adverse outcomes that may arise at the individual level, but also to those that may affect the public. This aspect of cannabis use will likely continue to be a priority among law enforcement and nongovernmental organizations such as Mothers Against Drunk Driving Canada (MADD),Footnote 32 given the recent changes to cannabis regulations.
Lastly, with respect to the severity of cannabis-related cases, this study identified 425 cases of serious injuries requiring admission to hospital. Of these, 56% involved children. While this larger proportion of children is likely reflective of the fact that eCHIRPP is more likely to capture the pediatric population than adults, it nevertheless signals an ongoing need to keep cannabis products out of the reach of children. The implementation of a minimum legal age requirement enforced by the provinces and territories is in line with this need, though to determine the effectiveness of this regulation, as well as the others introduced as a result of the October 2018 legalization, ongoing surveillance efforts examining cannabis-related injuries and poisonings will be required.
Strengths and limitations
The principal strength of our study is the use of eCHIRPP data, since the program can capture contextual information about injuries or poisonings presenting in EDs. This information is then transformed into a standardized form of coding, which allows for analysis. However, there are some limitations. While eCHIRPP sites are found in various regions across Canada, injury estimates arising from this program are not representative of the national population. A slight exception is injuries among youth, which may in fact be reflective of those occurring at the national level. For example, when comparing injury findings of the World Health Organization’s Health Behaviour in School-Aged Children Survey (WHO-HBSC) to those in eCHIRPP, Pickett et al.Footnote 33 found that the program may be representative of the general injury patterns among youth in Canada. However, such a finding does not apply to injuries and poisonings among older teenagers, adults, First Nations and Inuit peoples and those who live in rural and remote areas.Footnote 34 Additionally, at both ends of the severity spectrum, eCHIRPP does not capture fatal injuries or poisonings that occur outside of EDs, nor injuries or poisonings that are mild in nature and for which treatments are carried out in other medical settings, including medical clinics.
Of particular relevance to our study, strong sensitivity and specificity of the variables used for identifying cannabis-related cases in eCHIRPP have been demonstrated in Rao’s 2018 study,Footnote 19 reflecting good capture. However, patients’ reluctance to disclose the use of cannabis may have resulted in the underreporting of cannabis-related cases in eCHIRPP, especially in the years prior to the legalization of the recreational use of cannabis. Underreporting may also occur among those who use cannabis on a more regular basis and perhaps fail to recognize this substance as being one of the factors contributing to the injuries. Furthermore, because of the limitations of eCHIRPP data, we were not able to distinguish whether cannabis was used for medical or recreational purposes, nor were we able to ascertain the amount of the substance taken at the time of injury or poisoning. In the future, obtaining such information may lead to better identification of at-risk populations and a better understanding of the dose-response relationship of such injuries.
Conclusion
The aim of our study was to present a more recent temporal pattern of all cannabis-related injuries and poisonings found in the eCHIRPP database and provide a descriptive summary of the injury characteristics of such cases captured in the nine-year time period from 1 April, 2011, to 9 August, 2019. In so doing, we identified APC increases in cannabis-related cases among both children and adults in recent years. Males consistently represented a higher proportion of cannabis-related cases, which signals potential educational opportunities. While there was an increase in edible cannabis–related cases throughout this study period, they represented only a small proportion of all the cannabis-related cases. Such a finding suggests the need for parents and caregivers to implement safer storage practices. Though not representative of the national population, our findings indicate that cannabis-related injuries have increased in recent years in the eCHIRPP database among both children and adults. Continuing to monitor such injuries and poisonings through surveillance measures will be imperative, considering the recent changes to cannabis regulations in Canada.
Acknowledgements
We extend our sincere thanks to Deepa Rao, as the extracting and categorizing of all cannabis-related cases was made possible by applying her previous methodology. We also thank James Cheesman for providing the eCHIRPP extraction file.
Conflicts of interest
The authors have no conflicts of interest to declare.
Authors’ contributions and statement
ASC, SRM, WT and FB were involved in the design and conceptualization of the project. ASC conducted the data analyses and drafted the manuscript. All authors contributed to the interpretation of the results and revisions of the paper.
The content and views expressed in this article are those of the authors and do not necessarily reflect those of the Government of Canada.