The Canadian drugs and substances strategy: The Government of Canada’s approach to substance use related harms and the overdose crisis
Download the alternative format
(PDF format, 1.62 MB, 26 pages)
Organization: Health Canada
Date published: 2023-19-30
Cat.: H134-35/2023E-PDF
ISBN: 978-0-660-68488-8
Pub.: 230529
On this page
- Ministerial message
- Introduction
- About the strategy
- Our priorities for action under the Canadian drugs and substances strategy
- Implementation: monitoring and reporting on our progress
- Appendix: List of members of the Expert Task Force on Substance Use
Ministerial message
Canada is in the midst of one of the most serious and deadly public health crises in our country’s history - the toxic and illegal drug and overdose crisis. No community has been left untouched. Since 2016, more than 38,500 people have died of apparent opioid toxicity in Canada.
This crisis is tragic, and I want to recognize and remember the lives of people in Canada we have lost. Every person who overdoses is somebody who has a family and people that care about them and that we must do everything we can to support and protect them.
People who use substances, their families, and the communities around them, need us to use every tool at our disposal to provide compassionate care and maintain community safety. There is so much to be done and no one government, community or family can end this crisis alone.
That is why we are launching a renewed Canadian Drugs and Substances Strategy (CDSS) that has been designed to support a comprehensive and compassionate approach centered on promoting both public health and public safety. This whole-of-government initiative includes timely access to a full range of strategies to help people access the prevention, harm reduction, treatment, or recovery services and supports they need, when and where they need them.
The renewed CDSS is using an integrated approach that brings together prevention and education, substance use services and supports, evidence, and substance controls. New investments include supporting a wide range of activities such as community-based supports; streamlining authorizations for supervised consumption sites and drug checking services; vital data collection on substance-related harms and lab-based analysis of the illegal drug supply; an overdose monitoring platform for law enforcement and other first responders; and further action to work with our partners to disrupt illegal drug production and trafficking and stem the global flow of these devastating substances.
By using a wide-range of tools, we have the best opportunity to end this crisis, protect communities and save lives.
We must continue to work with our partners across all levels of government, communities, people with lived and living experience, and stakeholders to address the complex factors that contribute to substance use and related harms, including links with other issues, such as housing, mental health, economic insecurity, and chronic pain.
That’s the work we are doing, together. Because when people get the right support, there is hope. We are building a safer, healthier and more caring future for all Canadians. One where we embrace one another in the journey towards healing.
The Honourable Ya'ara Saks, P.C., M.P.
Introduction
Canada is experiencing an unprecedented and unrelenting rate of overdose deaths and harms, largely due to the toxic illegal drug supply that has continued to worsen since the start of the COVID-19 pandemic. National data shows that 38,514 apparent opioid toxicity deaths occurred between January 2016 and March 2023 (see Figure 1). The overdose crisis is complex and caused by many factors (see Box 1). In particular, drug traffickers and criminal organizations are seeking to maximize their profits by contaminating the illegal drug supply with inexpensive fentanyl and other opioids at a cost to Canadian lives. While in 2017 Canada saw a spike in fentanyl detected in the illegal drug supply, the overdose crisis continues to evolve and increasing amounts of other toxic substances are now present. This impacts the ability of first responders to reverse overdoses through the use of naloxone and makes the treatment of substance use disorders more complicated. Just under half (48%) of accidental apparent opioid toxicity deaths in 2023 also involved a stimulant, reflecting the role that the mixing of substances (polysubstance use) plays in this crisis.

Figure 1 - Text description
| Year | Crude rate of total apparent opioid toxicity deaths per 100,000 |
|---|---|
| 2016 | 7.8 |
| 2017 | 10.7 |
| 2018 | 11.4 |
| 2019 | 9.9 |
| 2020 | 16.9 |
| 2021 | 21.0 |
| 2022 | 19.2 |
| 2023 (January to March) | 20.3 |
The increasing toxicity and unpredictability of the illegal drug supply means that anyone is at risk for an overdose, whether they are trying drugs for the first time, or have been using drugs frequently. While anyone is at risk of a drug overdose, some populations in Canada have been disproportionately impacted by the crisis. Males accounted for the majority of apparent opioid toxicity deaths in Canada (70% to 75% since 2016). People living with co-occurring health conditions are also at increased risk of an overdose, including those with mental health conditions and chronic pain. Approximately 20% of Canadians with a substance use disorder (SUD) also have a co-occurring mental health disorder. Meanwhile, up to 55% of people who use drugs are also living with chronic pain.
Box 1. The overdose crisis has been driven by a dynamic and complex set of factors-but can generally be divided into four phases
The late 1990s to 2010 marked phase one of the overdose crisis which consisted of an overreliance on opioid prescriptions. During this phase, opioids were considered legitimate medications prescribed to treat acute or chronic pain, but the healthcare system’s overreliance on opioids resulted in a large numbers of Canadians being exposed to medications with high potential for higher risk use. The years 2010 to 2015 marked the second phase of the overdose crisis, which was characterized by an increase in diverted or illegally produced opioids. During this time period, there was an increase in diverted or illegally produced opioids bought and sold on the illegal market, which enabled opioid exposure among people who use drugs. The years 2015 to 2020 marked the third phase of the crisis where there was an unprecedented rise in synthetic opioids and analogues. During this phase, highly toxic synthetic opioids like fentanyl and its analogues were increasingly contaminating the illegal drug supply and driving the increasing mortality rates. From 2020 to the present is the fourth phase of the crisis where there is fentanyl dominance and widespread toxicity and unpredictability in the illegal drug supply. Currently, fentanyl continues to dominate the illegal drug market. The illegal supply remains highly unpredictable, with the introduction of stimulants, depressants and other emerging contaminants. There is increasing uncertainty as to what drugs are circulating in the illegal supply. In 2023, the illegal drug supply is more toxic than ever with fentanyl being widespread, both as a drug of choice as well as one of many contaminants found in other substances.
Indigenous populations in Canada also face an increased risk of overdose deaths and other substance use related harms. According to the First Nations Health Authority, First Nations people died of opioid toxicity deaths at 5.9 times the rate of other residents in British Columbia in 2022, a disproportionate impact on Indigenous populations that has also been seen across other provinces and territories. Historical and intergenerational trauma, including the impact of colonization, loss of traditional culture and language, and experiences with Indian Residential Schools, have contributed significantly to the elevated risk of overdose death and broader substance use related harms amongst Indigenous Peoples. Systemic racism arising from Canada's colonial history has also created inequities for African, Caribbean and Black populations, which has resulted in higher rates of poverty, unemployment, and precarious housing among these populations, placing them at greater risk of substance use harms.
In addition to the overdose crisis, Canada continues to see harms from other substances, such as tobacco and alcohol. In addition to the overdose crisis, Canada continues to see harms from other substances, such as tobacco and alcohol. According to the Canadian Costs of Substance Use and Harms 2007-2020 report, substance use and its related harms from all substances cost Canadians more than $49 billion and led to the loss of nearly 74,000 lives or 200 lives per day in 2020 (see Figure 2). In 2020, tobacco use was the leading cause of substance attributable deaths with 46,366 deaths in 2020, followed by alcohol use with 17,098 deaths and opioid use with 6,491 deaths. The harms related to substance use are not limited to the loss of lives alone, but also include increased costs to our health care system, from hospitalizations, emergency visits and specialized treatment for substance use disorders, which amounted to $13.4 billion in 2020. Substance use also has economic impacts due to lost productivity from premature deaths and time off work due to disability, which cost $22.4 billion in 2020. The enforcement of substance use laws cost Canada’s criminal justice system $10.0 billion in 2020.

Figure 2 - Text description
| Substance | Cost in billions of dollars |
|---|---|
| Alcohol | $19.7 |
| Tobacco | $11.2 |
| Cannabis | $2.4 |
| Opioids | $7.1 |
| Other CNS depressants | $1.4 |
| Cocaine | $4.2 |
| Other CNS stimulants | $3.0 |
| Other substances | $0.2 |
People use substances for many different reasons, such as medical purposes, personal enjoyment, religious or ceremonial purposes, or to cope with stress, trauma or pain. Substance use looks different for everyone and has varying stages of benefits and harms. Substance use related harms occur when substances are used in a manner, situation, amount, or frequency that harms the person using the substance or those around them. Examples of substance use related harms can include infection, hospitalization, risk of mental health disorders, including the risk of a substance use disorder; and the loss of income or housing. Harms may also occur in the illegal production, processing, and distribution of those substances such as community violence that disproportionately affects marginalized populations. Social and economic factors also impact a person's substance use, such as unemployment, housing insecurity or homelessness, poverty, trauma, colonialism, systemic racism, and stigma and can contribute to their marginalization from society.
Addressing this crisis therefore requires a holistic approach, centered on promoting public health and protecting public safety. People who use substances, their families and communities around them are counting on us to use every tool at our disposal to provide compassionate care and maintain community safety. We also cannot end this crisis alone. It requires all levels of government, Indigenous communities and people with lived and living experience and partners from law and border enforcement and health and social systems to come together to save lives. Our collective work to address this crisis will guided by our world leading renewed Canadian Drugs and Substances Strategy (CDSS).
About the strategy
The CDSS is the federal government's comprehensive response to substance use related harms and the overdose crisis in Canada. The CDSS is an all-substances, public health and public safety strategy that covers a broad range of legal and illegal substances, such as tobacco, cannabis, alcohol opioids and stimulants. The goal of the CDSS is to improve the health and safety of all Canadians by minimizing substance-related harms for individuals, families, and communities. In particular, it prioritizes children and youth who are more susceptible to the negative impacts of substance use as they are still growing and developing and focuses on providing them the supports, tools and help they need to prevent, delay and lower the rates of substance use related harms. It also focuses on connecting people to evidence based substance use services and supports, while also keeping communities safe by taking action against criminal organizations who are trafficking and producing illegal drugs.
The CDSS is a horizontal initiative that is led by the Minister of Mental Health and Addictions and Associate Minister of Health, who is supported by Health Canada and over 15 federal government departments and agencies. As addressing substance use related harms is a shared responsibility between federal, provincial and territorial governments, the CDSS focuses on areas of federal jurisdiction, such as:
- legislation and regulation
- funding to support the adoption of innovative approaches
- national surveillance and research
- services and supports for populations served by the federal government
Budget 2023 provided $359.2 million in new funding to support the implementation of the renewed CDSS. The renewal of the CDSS has been informed by national public consultations in 2018 and on-going stakeholder roundtable discussions where we have heard from communities, provinces and territories, Indigenous leaders, professional and regulatory bodies and health care providers. It has also been informed by the findings and recommendations made the Expert Task Force on Substance Use (please see Appendix for list of members), which focused on how we could strengthen the CDSS moving forward as well as potential alternatives to criminal penalties for personal possession of controlled substances. The renewal of our strategy also reflects the findings and recommendations of the Canadian Pain Task Force, which examined how pain could be better understood and effectively prevented and treated in Canada. It has also been guided by our on-going analysis of data and evidence that we have collected since the strategy was first introduced in 2016.
The foundational elements
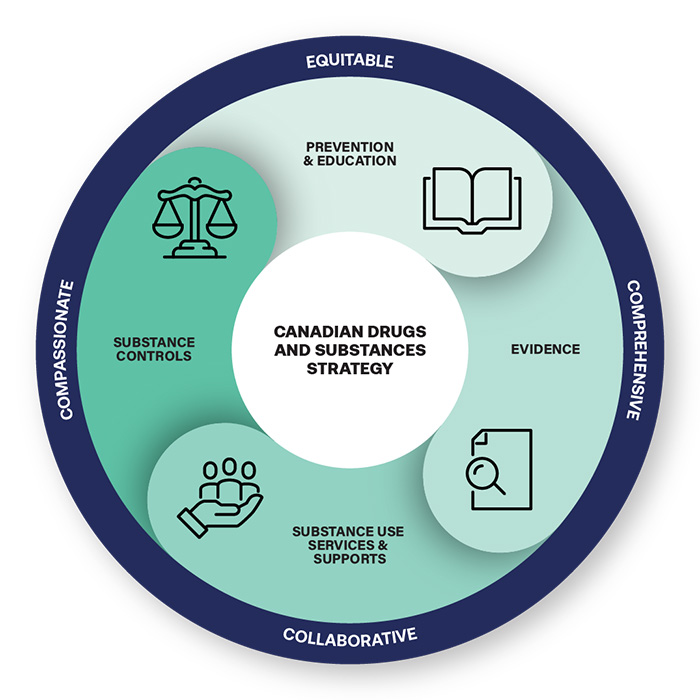
The CDSS has four integrated priority areas for action called foundational elements, including:
- Prevention and education initiatives to increase awareness and knowledge about the effects and risks of substances, and initiatives to prevent, reduce or delay substance use related harms.
- Substance use services and supports that support the full continuum of care, including treatment, harm reduction and recovery options as well as social services and supports to help people reduce their substance use related harms.
- Evidence through data and research to help inform substance use related policies and decision-making.
- Substance controls are activities that allow for the use of controlled substances and precursor chemicals for legitimate purposes, such as clinical trials or medical uses, while also giving health inspectors, law enforcement and border control authorities the tools that they need to enforce the laws and regulations that keep Canadians safe and address the harms of the illegal drug market.
Guiding principles
The CDSS is led by four guiding principles. It is:
- Compassionate by treating substance use as a health issue and people who use substances with compassion and respect, and recognizing stigma as a barrier to accessing health and other services.
- Equitable by recognizing the distinct impacts that substance use policies and interventions can have on Indigenous Peoples, African, Caribbean, Black and other racialized and marginalized populations.
- Collaborative by engaging all levels of government, Indigenous Peoples, communities, stakeholders, people with lived and living experience, law and border enforcement and international partners.
- Comprehensive by recognizing that substance use is different for everyone and requires a range of policies, services and supports to promote overall wellbeing and that many substance use related harms arise from the toxic illegal drug supply and illegal drug market more broadly.
Our priorities for action under the Canadian drugs and substances strategy
Prevention and education
Prevention and education initiatives support communities, and raise awareness to influence the health and wellbeing of people living in Canada. They aim to:
- educate people living in Canada by providing factual information that helps them make informed choices around substance use related harms and where to get help
- prevent, delay or reduce substance use related harms by reducing the factors that increase their risk, while increasing those that help protect against them
- reduce healthcare, social, economic and criminal justice system costs by preventing substance use harms
Addressing known risk and protective factors, especially early in life, is key in reversing the current trends of substance use related harms (see Figure 3). Risk factors are characteristics or experiences that increase the likelihood of a negative health outcome or harm due to substance use, whereas protective factors promote an person's overall health and well-being and decrease their likelihood of experiencing harms related to their substance use.
Figure 3. Risk and protective factors for substance use related harms
Risk factors
- Trauma
- Childhood adversity
- Mental illness
- Poverty
- Unstable housing
- Drug availability
- Chronic pain
Protective factors
- Caregiver involvement
- Coping skills
- Social inclusion
- Safe neighbourhoods
- Quality school environment
- Permanent housing
Factors like sex, gender, age, race, pre-existing health conditions, socioeconomic status, ability, sexual orientation, migration status, and geography, may also interact with each other to create multiple experiences of stigma, discrimination and marginalization for some individuals and population groups, such as 2SLGBTQIA+ populations, placing them at greater risk for negative mental health and substance use outcomes, while also limiting their access to health-related resources that could prevent substance use related harms. Experiences of discrimination, racism and intergenerational trauma arising from Canada's history of colonialism are also important determinants of health for certain groups in Canada such as Indigenous Peoples and Black Canadians.
What is the Government of Canada doing?
To prevent substance use related harms among youth, at risk and other marginalized populations and disproportionately impacted populations, we are:
Investing in community-led programs
- A new Youth Substance Use Prevention Program based upon the Icelandic Prevention Model will provide funding to communities to build their capacity to support data-driven community-led approaches to prevent and delay substance use related harms in youth
- Harm Reduction Fund provides funding to time-limited projects across Canada that help reduce HIV and hepatitis C among people who share injection and inhalation drug-use equipment
- Mental Wellness Program to support First Nations and Inuit access to mental wellness services
- National Crime Prevention Strategy provides funding to communities to address known risk and protective factors to prevent at risk, vulnerable youth from participating in crime
Raising awareness of substance use related harms, including stigma, through public education and outreach activities
We are raising awareness of substance use related harms and ways to reduce them, and the importance of reducing stigma, through public education, outreach activities and awareness campaigns. Stigma leads people to hide their substance use and prevents them from getting help for fear of reprisals, being labelled or judged. Examples of our campaigns include:
- Know More Opioids youth awareness program that educates teens and youth on the risks of opioids and substance use related harms and ways to reduce them
- Ease the Burden Campaign that promotes resources and supports for men working in physically demanding jobs who are at higher risk of substance use related harms
- Multi-year campaign to raise awareness of opioids, how to respond to an overdose, the Good Samaritan Drug Overdose Act and the impacts of stigma on people who use drugs
- Drug Stigma Awareness Training for the law enforcement community to help support frontline officers in their interactions with people who use substances
- Resources and information for people who need help with substance use related harms
Box 2. Reducing stigma around substance use disorders
The Substance Use and Addictions Program (SUAP) supports projects that aim to reduce stigma associated with substance use disorders through public education, capacity building and research. With support from SUAP, the Sinai Health System redeveloped Effective Prescribing of Opioids for Chronic Pain (EPOCH), a training programfor primary health care providers to help build their competencies in treating substance use disorder. Beyond Stigma is a public and professional education program focused on stigma that complements the EPOCH training program and includes two videos:
- The Treating Pain in Opioid Use Disorder video which explores the impact of stigma on all aspects of treatment for people living with a opioid use disorder
- The Nurturing Circle of Care video which explores the impact of colonialism and institutional racism on stigma for Indigenous Peoples with opioid use disorders
Working with our partners to address the root causes of substance use related harms
We will work with our partners to leverage existing federal initiatives to address underlying inequities that are the root causes of substance use related harms and support the provision of social services, such as:
- reducing homelessness with the implementation of Reaching Home: Canada's Homelessness Strategy
- reducing poverty by implementing initiatives under the Opportunity for All – Canada's First Poverty Reduction Strategy
- promoting programs that focus on mental health and preventing family and gender-based violence
To address the role that unmanaged chronic pain plays in substance use related harms, we will also continue to work across all levels of government and with professional organizations and other key stakeholders to advance the priorities identified by the Canadian Pain Task Force, including ensuring that people living in Canada, including those who use substances, have better access to pain management services. Since 2018, there have been over 25 pain related projects funded through the Substance Use and Addictions Program to support the mental health and wellbeing of people who live with chronic pain in Canada.
Substance use services and supports
Substance use is different for each person and there is no single service that will meet the needs of everyone. The Government of Canada is therefore focusing on supporting equitable access to a continuum of effective, culturally appropriate and trauma informed evidence-based health services and supports to meet the diverse needs of individuals who use substances, including:
- Treatment: a range of approaches to help reduce, or cease, substance use related harms by managing withdrawal and cravings, such as psychological and behavioural interventions like talk based therapy and counselling that provide practical advice and support on abstinence or reduced use and other behavioural therapies that treat addictions; peer support from people with lived and living experience who offer emotional support; and pharmacological interventions that reduce cravings and withdrawal symptoms.
- Harm Reduction: an evidence-based, public health approach that aims to reduce the negative health, social, and economic impacts of substance use related harms, without requiring or promoting abstinence. Examples of harm reduction services could include providing drug checking services so that an individual can make informed decisions about the drugs that they are consuming or providing someone with a naloxone kit in case there is an overdose.
- Recovery: a process or lifestyle change where people who struggle with substance use related harms work to improve their health and well being, which could include accessing services and supports that have complete abstinence as a goal or a variety of harm reduction and treatment services, as well as broader social services and supports to meet employment, vocational training, housing, income and cultural needs.
Box 3. Spotlight on the Eastside Movement for Business and Economic Renewal Society
People who use substances need a range of integrated health and social services to support their health and wellbeing. Funded through the Substance Use and Addictions Program, the Eastside Movement for Business and Economic Renewal Society's Support and Employment Program provides rapid access, long-term substance use care to people who have gained employment and are now ready to better manage their substance use in order to maintain their employment and stabilize their overall lives. Evaluations of this project found that achieving employment goals was positively correlated with reduced risk of substance use related harms and improvements in physical and mental health.
What is the Government of Canada doing?
Supporting equitable access to a continuum of substance use services and supports
Though the delivery of substance use services and supports is primarily the responsibility of the provinces and territories, we are playing a critical role by improving equitable access to these services through investments, such as:
- $196.1 billion over 10 years, including $46.2 billion in new funding through the Canada Health Transfer and other mechanisms, for provinces and territories to improve health care services for Canadians. This funding includes:
- $25 billion over 10 years to provinces and territories for bilateral agreements to address unique needs in four shared health priorities, including access to quality mental health and substance use services
In addition, we are investing $2 billion over 10 years to address unique challenges Indigenous Peoples face when it comes to fair and equitable access to quality and culturally safe health care services.
The Substance Use and Addictions Program (SUAP) also provides grant and contribution funding to other levels of government, community-led and not-for-profit organizations, for innovative evidence-based harm reduction, treatment and recovery projects that focus on at risk and disproportionately impacted populations, such as young and middle-aged men, Indigenous People, people experiencing chronic pain, 2SLGBTQIA+ populations and Black Canadians. This program has also supported building the evidence base for innovative approaches to harm reduction such as safer supply. SUAP is currently funding 29 safer supply pilot projects across the country. Safer supply is a promising harm reduction practice that involves health care practitioners providing prescription drugs as an alternative to highly toxic street drugs, with the goal of helping to reduce overdoses for those most at risk.
Box 4. Spotlight on Somerset West Community Health Centre's Drug Overdose Prevention and Education Program
Somerset West Community Health Centre's Drug Overdose Prevention and Education (DOPE) Project provides peer outreach to isolated people who use drugs in Ottawa, who otherwise may not have access to services and supports. This peer based program uses the knowledge, expertise and social networks of people who use drugs or have used drugs to provide support, resources and training on overdose prevention and response, including the use of Naloxone, a medication that can be used to reverse an opioid overdose. Since 2019, this Substance Use and Addictions Program funded project has:
- Conducted 441 injectable and 401 nasal naloxone training sessions
- Provided 1296 injectable and 1789 nasal naloxone kits
- Administered naloxone to community members 75 times
We will also streamline authorizations for supervised consumption sites, urgent public health need sites and drug checking services to create a new authorization process with clear public health and public safety requirements for organizations seeking to provide these evidence-based life saving services to Canadians.
Providing substance use services and supports for populations served by the federal government
We support the provision of substance use services and supports to some populations both directly and indirectly served by the federal government, such as:
- culturally appropriate and trauma-informed substance use services and supports within Indigenous communities
- people in federal correctional institutions
- Opioid Agonist Treatment, psychosocial and peer supports and harm reduction services to people in federal correctional institutions
- court-monitored treatment and community services for non-violent offenders with substance use disorder through the Drug Treatment Court Funding Program
- youth interacting with the criminal justice system who are struggling with complex needs, including trauma and mental health and substance use disorders through the Youth Justice Fund
- veterans, including those experiencing or at risk of homelessness through the Veteran Homelessness Program
Box 5. Supporting access to culturally grounded mental wellness and substance use services and supports in partnership with Indigenous communities
Indigenous Services Canada (ISC) recognizes that accessibility of quality federally funded health services is key to achieving physical and mental wellness for Indigenous Peoples. ISC continues to prioritize the implementation of distinctions-based mental wellness initiatives. The department works collaboratively with partners to improve access to high quality culturally grounded community based mental health and substance use services and supports for First Nations, Inuit and Métis, including: life promotion and suicide prevention programs, including on-the-land activities, mental wellness teams, the Hope for Wellness Help Line, as well as funding for a network of 45 treatment centres and drug and alcohol use prevention services. ISC also supports the provision of essential cultural, emotional and mental health supports to Survivors of Indian Residential Schools and Federal Indian Day Schools and families of former students, as well as those affected by the issue of Missing and Murdered Indigenous Women, Girls, and 2SLGBTQIA+ people. These initiatives are guided by the First Nations Mental Wellness Continuum Framework, and the National Inuit Suicide Prevention Strategy, which are holistic frameworks developed by and with Indigenous partners.
Evidence
Accurate, timely, reliable data and research are essential to policy development and decision making. They allow us to:
- assess the current situation
- identify trends
- set policy priorities
- respond to emerging drug issues
- measure our impact
What is the Government of Canada doing?
We are building our capacity to collect, analyze and disseminate disaggregated data in a timely manner and conduct research to support equity informed, evidence-based decision making to address the overdose crisis and substance use related harms. The new CDSS Data and Evidence Framework will guide these efforts by prioritizing the following activities:
- Conducting and updating our general population surveys to include sex and gender-based analysis plus data to better understand substance use trends among different population groups in Canada. Examples include:
- Developing new targeted surveys and research to identify trends among and needs of. at-risk, marginalized, Indigenous and racially diverse populations to support the development of programs and initiatives that better meet their needs.
- Strengthening current innovative approaches to surveillance to support public health and law enforcement's timely response to the overdose crisis and emerging trends in the illegal drug market by:
- Working with provinces and territories to collect and report data on opioid- and stimulant- related deaths and harms
- Providing bi-annual simulation models of opioid-related deaths during the overdose crisis
- Laboratory analysis of drugs seized by law enforcement by Health Canada's Drug Analysis Service to support investigations and prosecutions involving illegal drugs, as well as to better understand trends in the illegal drug supply, including the emergence of new harmful substances
- gathering data from supervised consumption sites to understand demand for harm reduction services, types of drugs consumed and the impact these services have on reducing overdose deaths and supporting access to other substance use services and supports.
- Monitoring the impact of our policies and programs through activities such as:
- supporting the Canadian Research Initiative in Substance Misuse (CRISM)'s five-year independent, scientific evaluation of the impacts of the subsection 56 (1) exemption for adults (18 years and older) in the province of British Columbia to remove criminal penalties for people who possess a small amount of certain illegal substances for personal use
- supporting a four year CRISM led evaluation of the implementation and impact of safer supply pilot projects
- Supporting the evaluation of data and research to develop evidence-based guidance to prevent and address substance use related harms and support treatment, such as British Columbia Centre on Substance Use's National Guideline for the Clinical Management of High-Risk Drinking and Alcohol Use Disorder
Substance controls
The Government of Canada has various laws in place that regulate access to controlled substances, precursor chemicals, cannabis, alcohol and tobacco and vaping products to mitigate their public health and safety risks while supporting access to them for legitimate purposes. These include:
- the Controlled Drugs and Substances Act (CDSA) is the federal law that prohibits the possession, production, distribution, and sale of controlled substances, unless authorized through the regulations or an exemption, to protect public health and public safety. Controlled substances are those that can alter mental process and may harm a person’s health or society when used inappropriately or diverted to an illegal market.
- the Cannabis Act creates a strict legal framework for controlling the production, distribution, sale and possession of cannabis across Canada
- the Tobacco and Vaping Products Act regulates the manufacture, sale, labelling and promotion of tobacco products and vaping products sold in Canada
- the Food and Drugs Act applies to food, drugs, medical devices and cosmetics
The Government of Canada also has obligations under international drug control conventions, including measures to ensure the availability of drugs and substances for medical and scientific purposes while also preventing their diversion into the illegal market and collaborating with international partners to combat drug trafficking:
- Single Convention on Narcotic Drugs, 1961
- Convention on Psychotropic Substances, 1971
- United Nations Convention against the Illicit Traffic in Narcotic Drugs and Psychotropic Substances, 1988
What is the Government of Canada doing?
To support the administration and enforcement of our substance control laws, we are focusing our efforts on authorizing activities with controlled substances and precursor chemicals for legitimate purposes, such as clinical trials or medical uses, while also giving health inspectors, law enforcement and border control authorities the tools that they need to enforce the laws that keep people living in Canada safe and address the harms of the illegal drug trade. To achieve this objective, we will:
Provide law enforcement and public health officials with new tools to respond to the overdose crisis
Law enforcement interact daily with people who use substances and have crucial role to play in supporting a public health approach to substance use related harms. We are supporting law enforcement in this role by:
- offering training to raise awareness of drug stigma
- piloting an overdose monitoring platform to provide near real-time suspected overdose surveillance data to support an immediate community-level response to a sudden increase or spike in overdose events and collect information on organized crime’s drug trafficking patterns to support decision-making.
Target organized drug crime
We are working with law and border enforcement partners across the country to address the role of organized crime in the production, diversion and trafficking of toxic illegal drugs. Our activities include:
- preventing cross-border movement of illegal drugs and precursor chemicals through on-going enforcement efforts
- supporting major drug enforcement operations both domestically and internationally and the dismantling of illegal drug labs
- collecting, assessing and sharing criminal intelligence on the illegal drug supply among law enforcement partners
- working closely with the United States and other countries to identify and disrupt shipments of illegal drugs destined for Canada
- providing forensic accounting services to support law enforcement agencies in conducting complex and sophisticated organized drug crime investigations
- identifying drugs seized by law enforcement agencies to support police investigation and enforcement of our drug laws
Support the diversion of people away from the criminal justice system and towards the health and social services
To address the harms that people who use substances experience as result of their interactions with the criminal justice system, such as stigma, loss of income and employment and loss of housing, and the over representation of Indigenous, racialized and diverse populations within the criminal justice system, we have introduced a number of measures:
- Bill C-5, which repealed mandatory minimum penalties for all drug offences in the Controlled Drugs and Substances Act; it also requires police and prosecutors to consider diverting people who commit simple drug possession offences toward health and social services
- guidance to prosecutors to encourage them to consider alternatives for simple drug possession offences, except when there are serious public safety concerns
- the Good Samaritan Drug Overdose Act, which provides some legal protection for people who seek emergency help during an overdose
We will continue to support policies and approaches that divert people who use substances away from the criminal justice system and towards health and social services by:
- continuing our engagement and monitoring of the Province of British Columbia's implementation of the three-year subsection 56(1) exemption for adults (18 years of age and older) in the province of British Columbia to remove criminal penalties for people who possess small amounts of certain illegal substances for personal use
Facilitate access to controlled substances for medical and scientific purposes and/or in the public interest
We will also continue to facilitate the use of controlled substances in scientific research and medical treatment, or when it is in the public interest, with appropriate controls in place by providing exemptions under subsection 56(1) of the CDSA.
Advance a coordinated global approach to substance related harms and the illegal drug supply
We are also participating in international forums to advance a coordinated and global approach to substance use related harms that balances public health and public safety interests through information sharing and joint action. Key international forums include:
- Canada-US Opioids Action Plan
- Cross-Border Crime Forum
- North American Trilateral Fentanyl Committee
- North American Drug Dialogue
- Global Coalition to Address Synthetic Drug Threats
- United Nations Commission on Narcotic Drugs
Box 6. Spotlight on the Canada-United States Joint Action Plan on Opioids
Launched in January 2020, the Canada-United States Joint Action Plan on Opioids brings our two countries together to find solutions to the overdose crisis, which continues to take a tragic toll on families, loved ones and communities on both sides of the border. Through the Action Plan, Canada and the United States are taking steps in law enforcement, border security and health to address this tragic crisis. Together, we are:
- sharing information and best practices
- collaborating to stop trafficking in opioids, including fentanyl, and their precursor chemicals
- addressing the health consequences of harmful opioid use
Implementation: monitoring and reporting on our progress
Our shared goal is to reduce overall rates of substance use related harms and overdose deaths in Canada. Long-term success will be measured through our ability to decrease substance related deaths and hospitalizations. Over the next five years, we will evaluate the impact of the activities under the Strategy by monitoring progress towards:
- Greater awareness, knowledge, skills and resources related to substance use and related harms
- More equitable access to services and supports to reduce substance use related harms
- Access to population specific data and evidence on substance use related harms and the illegal drug supply to make informed decisions
- Law enforcement and health authorities have the tools they need to administer and enforce our laws and regulations related to controlled substances and precursor chemicals
Our success in achieving these results will depend on our ability to collaborate with many partners and stakeholders. We are committed to publicly reporting our progress, including impacts on at risk and marginalized populations, Indigenous Peoples and racialized communities.
Appendix: List of members of the Expert Task Force on Substance Use
The following people were members of the Expert Task Force on Substance Use:
- Carol Hopkins (Co-Chair), CEO of the Thunderbird Partnership Foundation (a division of the National Native Addictions Partnership Foundation)
- Dr. Kwame McKenzie (Co-Chair), CEO of Wellesley Institute, Director of Health Equity at the Centre for Addiction and Mental Health, Full Professor in Psychiatry at the University of Toronto and consultant with the World Health Organization
- Mike Serr (Co-Chair), Chief Constable, Abbotsford Police Department; Chairperson of the Drug Advisory Committee, Canadian Association of Chiefs of Police (CACP), and Chair of the CACP's Special Purposes Committee on the Decriminalization of Illicit Drugs
- Natasha Touesnard (Co-Chair, stepped down in April 2021) the Executive Director of the Canadian Association of People who Use Drugs
- Serge Brochu, PhD, Professor, École de criminologie at the Université de Montréal
- Deirdre Freiheit, President and CEO, Shepherds of Good Hope (SGH) and Shepherds of Good Hope Foundation
- Gord Garner, Executive Director, Community Addictions Peer Support Association
- Charles Gauthier, President and CEO, Downtown Vancouver Business Improvement Association
- Cheyenne Johnson, Executive Director, British Columbia Centre on Substance Use (BCCSU)
- Harold R. Johnson, Elder, Advisor and Ambassador, Northern Alcohol Strategy Saskatchewan, Former Crown Prosecutor
- Damon Johnston, Chair, Addictions Foundation of Manitoba, and President, Aboriginal Council of Winnipeg
- El Jones, Spoken Word Poet, Educator, Journalist, and a Community activist living in African Nova Scotia
- Mae Katt, Primary Health Care Nurse Practitioner, Thunder Bay and Temagami First Nation
- Robert Kucheran, Chairman of the Executive Board, Canada's Building Trades Unions
- Frankie Lambert, Communications Officer, AQPSUD (Association Québécoise pour la promotion de la santé des personnes utilisatrices de drogues / Québec Association for Drug User Health Promotion)
- Anne Elizabeth Lapointe, Executive Director, Maison Jean Lapointe and Addiction Prevention Centre
- Dr. Shaohua Lu, Addiction Forensic Psychiatrist, Clinical Associate Professor, University of British Columbia
- Donald MacPherson, Director, Canadian Drug Policy Coalition
- Akwasi Owusu-Bempah, PhD, Assistant professor, Department of Sociology, University of Toronto
- Hawkfeather Peterson, President of BCYADWS (BC/Yukon Association of Drug War Survivors), Regional Peer Coordinator of the Northern Health Authority in BC
- Dan Werb, PhD, Executive Director, Centre on Drug Policy Evaluation, MAP Centre for Urban Health Solutions, Li Ka Shing Knowledge Institute of St. Michael's Hospital, Assistant Professor, University of Toronto Institute of Health Policy, Management and Evaluation, and Assistant Professor, University of California San Diego Division of Infectious Diseases and Global Public Health