Federal actions on the overdose crisis
The Government of Canada's actions to address the overdose crisis to help save lives, including government funding for projects, prevention and education efforts, evidence used to inform decision-making, substance use services and supports, like increased access to treatment and harm reduction programs, and substance controls.
Last updated: December 2023
On this page
- About the overdose crisis
- Snapshot of the overdose crisis
- Recent federal actions
- Government funding
- Prevention and education
- Evidence
- Substance use services and supports
- Substance controls
About the overdose crisis
The overdose crisis continues to have significant impacts on Canadian communities and families. People who use drugs face many barriers and risks, such as:
- the highly toxic and unpredictable illegal drug supply
- over-burdened health and social services, including life-saving harm reduction and treatment services and supports
- ongoing stigma surrounding substance use that discourages people from seeking health and social services, and can reduce the quality and availability of services received
The Government of Canada is committed to a comprehensive public health approach to the overdose crisis that is focused on reducing harms, saving lives, and getting people the supports they desire and need.
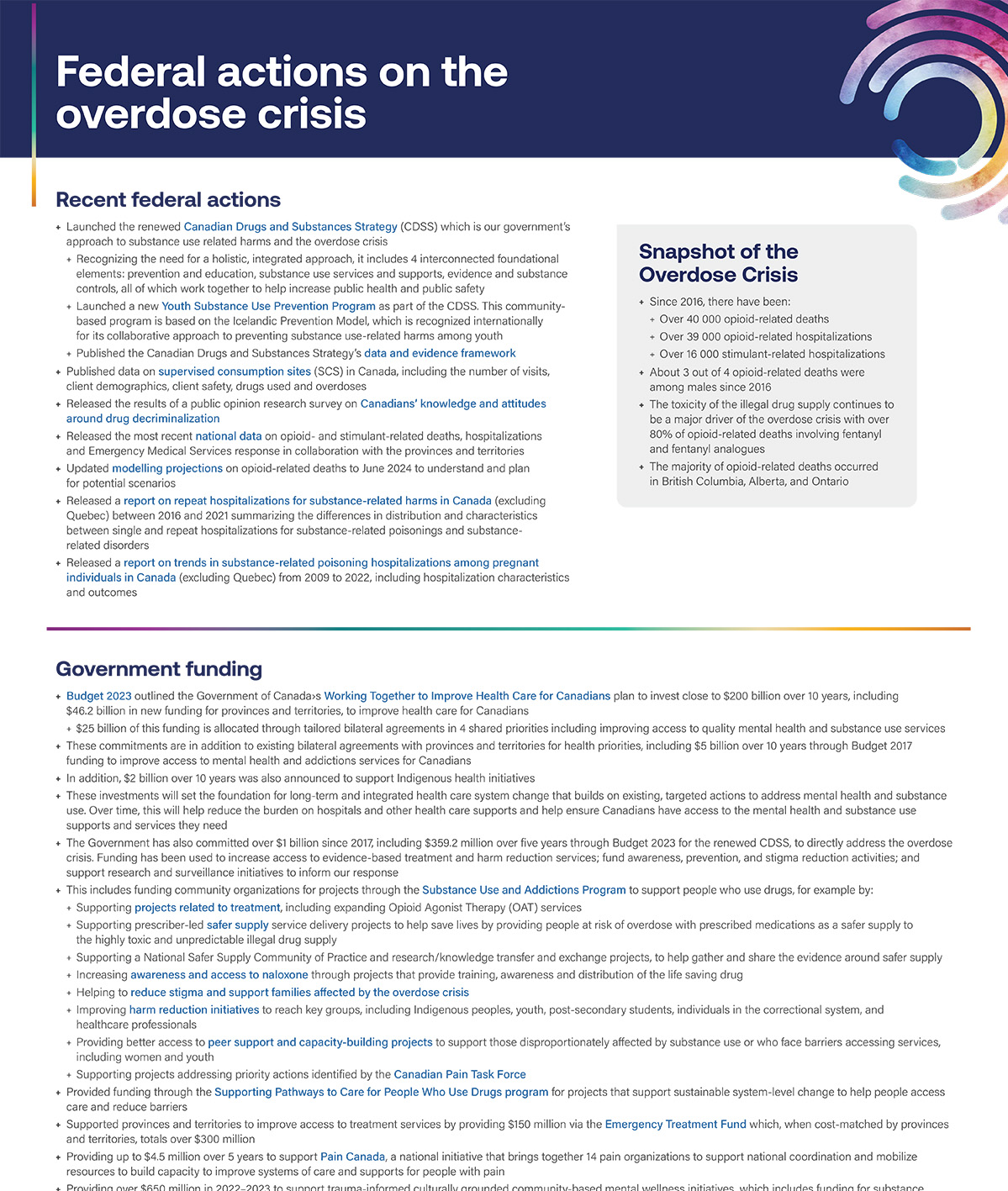
Snapshot of the overdose crisis
- Since 2016, there have been:
- over 40 000 opioid-related deaths
- over 39 000 opioid-related hospitalizations
- over 16 000 stimulant-related hospitalizations
- About 3 out of 4 opioid-related deaths were among males since 2016
- The toxicity of the illegal drug supply continues to be a major driver of the overdose crisis with over 80% of opioid-related deaths involving fentanyl and fentanyl analogues
- The majority of opioid-related deaths occurred in British Columbia, Alberta, and Ontario
Recent federal actions
- Launched the renewed Canadian Drugs and Substances Strategy (CDSS) which is our government's approach to substance use related harms and the overdose crisis
- Recognizing the need for a holistic, integrated approach, it includes 4 interconnected foundational elements: prevention and education, substance use services and supports, evidence and substance controls, all of which work together to help increase public health and public safety
- Launched a new Youth Substance Use Prevention Program as part of the CDSS. This community-based program is based on the Icelandic Prevention Model, which is recognized internationally for its collaborative approach to preventing substance use-related harms among youth
- Published the data and evidence framework as part of the CDSS
- Published data on supervised consumption sites (SCS) in Canada, including the number of visits, client demographics, client safety, drugs used and overdoses
- Released the results of a public opinion research survey on Canadians' knowledge and attitudes around drug decriminalization
- Released the most recent national data on opioid- and stimulant-related deaths, hospitalizations and Emergency Medical Services response in collaboration with the provinces and territories
- Updated modelling projections on opioid-related deaths to June 2024 to understand and plan for potential scenarios
- Released a report on repeat hospitalizations for substance-related harms in Canada (excluding Quebec) between 2016 and 2021 summarizing the differences in distribution and characteristics between single and repeat hospitalizations for substance-related poisonings and substance-related disorders
- Released a report on trends in substance-related poisoning hospitalizations among pregnant individuals in Canada (excluding Quebec) from 2009 to 2022, including hospitalization characteristics and outcomes
Government funding
- Budget 2023 outlined the Government of Canada's Working Together to Improve Health Care for Canadians plan to invest close to $200 billion over 10 years, including $46.2 billion in new funding for provinces and territories, to improve health care for Canadians
- $25 billion of this funding is allocated through tailored bilateral agreements in 4 shared priorities including improving access to quality mental health and substance use services
- These commitments are in addition to existing bilateral agreements with provinces and territories for health priorities, including $5 billion over 10 years through Budget 2017 funding to improve access to mental health and addictions services for Canadians
- In addition, $2 billion over 10 years was also announced to support Indigenous health initiatives
- These investments will set the foundation for long-term and integrated health care system change that builds on existing, targeted actions to address mental health and substance use. Over time, this will help reduce the burden on hospitals and other health care supports and help ensure Canadians have access to the mental health and substance use supports and services they need
- The Government has also committed over $1 billion since 2017, including $359.2 million over five years through Budget 2023 for the renewed CDSS, to directly address the overdose crisis. Funding has been used to increase access to evidence-based treatment and harm reduction services; fund awareness, prevention, and stigma reduction activities; and support research and surveillance initiatives to inform our response
- This includes funding community organizations for projects through the Substance Use and Addictions Program to support people who use drugs, for example by:
- Supporting projects related to treatment, including expanding Opioid Agonist Therapy (OAT) services
- Supporting prescriber-led safer supply service delivery projects to help save lives by providing people at risk of overdose with prescribed medications as a safer supply to the highly toxic and unpredictable illegal drug supply
- Supporting a National Safer Supply Community of Practice and research/knowledge transfer and exchange projects, to help gather and share the evidence around safer supply
- Increasing awareness and access to naloxone through projects that provide training, awareness and distribution of the life saving drug
- Helping to reduce stigma and support families affected by the overdose crisis
- Improving harm reduction initiatives to reach key groups, including Indigenous peoples, youth, post-secondary students, individuals in the correctional system, and healthcare professionals
- Providing better access to peer support and capacity-building projects to support those disproportionately affected by substance use or who face barriers accessing services, including women and youth
- Supporting projects addressing priority actions identified by the Canadian Pain Task Force
- Provided funding through the Supporting Pathways to Care for People Who Use Drugs program for projects that support sustainable system-level change to help people access care and reduce barriers
- Supported provinces and territories to improve access to treatment services by providing $150 million via the Emergency Treatment Fund which, when cost-matched by provinces and territories, totals over $300 million
- Providing up to $4.5 million over 5 years to support Pain Canada, a national initiative that brings together 14 pain organizations to support national coordination and mobilize resources to build capacity to improve systems of care and supports for people with pain
- Providing over $650 million in 2022-2023 to support trauma-informed culturally grounded community-based mental wellness initiatives, which includes funding for substance use prevention and treatment, the continued implementation of 75 Mental Wellness Teams supporting 385 First Nations and Inuit communities, the Hope for Wellness Help Line, and more
Prevention and education
- Expanded public awareness around opioids and the harms of substance use stigma:
- Launched a multi-year campaign in 2018 to raise awareness of opioids, the signs of an overdose, the Good Samaritan Drug Overdose Act and the impacts of stigma on people who use drugs
- Continued a campaign to promote help-seeking and links to resources and supports aimed at men working in physically demanding jobs, who are disproportionately affected by the overdose crisis
- Developed and distributed awareness resources for opioids, such as videos, fact sheets, posters, wallet cards, and an audio series
- Delivered the Know More Opioids awareness program to more than 1,400 virtual and 380 in-person high school sessions, and engaged over 178,000 teens and young adults between April 2018 and December 2023
- Reached out to over 2000 festival organizers to provide information about naloxone and encourage the distribution of overdose prevention materials to event goers and staff
- Coordinated federal efforts to respond to the Canadian Pain Task Force recommendations, so that pain is understood, prevented, and effectively treated
- Supported knowledge mobilization of stakeholder developed guidance and resources to improve pain management
- Pediatric pain management standard to help guide practice, professional development, policy development, and quality improvement initiatives related to pediatric pain management in all hospital healthcare settings
- Power Over Pain portal, a virtual platform that provides Canadians rapid access to free evidenced-based virtual resources, interventions and peer-support to help youth and adults manage their chronic pain
- Development of a new national, competency-based curriculum for current and future physicians in pain management and addiction medicine
- Supported the development of Soar Above Stigma, a resource that provides outreach support and stigma education for Indigenous community members dealing with addiction or mental health issues
- Shared best practices for addressing substance use stigma within the Canadian health system, including through use of compassionate and non-stigmatizing language
- Continued engagement activities with law enforcement community to promote uptake of an online Drug Stigma Awareness Training module with free access extended to law enforcement members until December 31, 2023
- Developed a toolkit of resources for employers of Canadians working in the trades and related industries to help reduce the harms of substance use
- Developed a Blueprint for Action and policy paper for schools and community organizations that support youth, outlining practical approaches for schools to prevent substance-related harms among youth
- Adopted non-stigmatizing language in Health Services products and reviewing staff training and education aimed at reducing substance-related stigma in Canada's correctional system
Evidence
- Conducted data collection for the 2023 Canadian Alcohol and Drugs Survey
- Released the results of the 2021-22 Canadian Student Tobacco, Alcohol and Drugs Survey
- Released the results of the 2021-22 Canadian Postsecondary Education Alcohol and Drug Use Survey
- Held a Knowledge Exchange Series on Safer Supply with key stakeholders to discuss evidence around safer supply, share best practices in providing safer supply programs, and discuss how current evidence can help expand the range of models and services provided, followed by a What We Heard Report
- Held a Best Brains Exchange to enhance and share knowledge related to best practices and treatment options for people living with chronic pain and concurrent mental illnesses and/or substance use-related conditions, followed by a report highlighting the outcomes of the event
- Published "Spotlight: The Emergence of Xylazine in Canada", a report about the emergence of Xylazine (a prescription drug used in veterinary medicine) that is increasingly being detected in the toxic illegal drug supply
- Renewed investment of $17 million over 6 years for the continuation and expansion of the Canadian Research Initiative in Substance Misuse (CRISM) to conduct research and knowledge mobilization activities focused on substance use harms, such as opioids (including a national study on methamphetamine use disorder)
- Invested $2.85 million over 5 years to support an independent, scientific evaluation led by CRISM of the impacts of the section 56 exemption granted in British Columbia related to the personal possession of controlled substances
- Semi-annual reports will be published to share interim findings and results with relevant partners and stakeholders
- Continued collection of the Canadian Wastewater Survey with information on drugs and drug metabolites in wastewater samples collected (methamphetamine, amphetamine, other stimulants)
- Established an Expert Task Force on Substance Use that provided independent, expert recommendations on the federal government's drug policy and potential alternatives to criminal penalties for personal possession
- Published a toolkit with resources for stakeholders to respond to a need for information on medications for people at risk of overdose during the pandemic
- Funded a preliminary qualitative assessment of 10 safer supply pilot projects, conducted by an independent contractor to capture early learnings, including effective strategies for program delivery
- Invested over $3 million over 4 years to evaluate program implementation and impacts of safer supply pilot projects and to assess the public health impacts of supervised consumption sites (SCS) located in British Columbia, the Prairies, Ontario and Quebec-Atlantic
- A summary of findings from the SCS evaluation projects is available in the end-of-grant workshop report
- A summary of findings from the Midpoint Knowledge Exchange Forum Evaluation on Safer Supply is now available
- Released several reports related to furthering knowledge around opioids
Substance use services and supports
Treatment
- Supported the development of guidance for health care providers, including:
- Clinical guidelines and operational guidance for injectable opioid agonist treatment
- National treatment guidelines for opioid use disorders
- Removed barriers to accessing drugs used for the treatment of opioid use disorder by:
- Issuing a class exemption for patients, practitioners, and pharmacists prescribing and providing controlled substances in Canada to ensure continuity of care
- Approving injectable hydromorphone and diacetylmorphine as treatment options for patients with severe opioid use disorder
- Facilitating the prescribing and dispensing of methadone and diacetylmorphine through regulatory amendments
- Developing national standards based deliverables for mental health and substance use services to provide an evidence-based framework for service delivery
- Supporting federally-funded treatment centres for First Nations and Inuit to create and enhance their virtual treatment services, allowing for increased reach and accessibility to those who may not otherwise seek treatment
- Supporting Opioid Agonist Therapy wraparound supports in 82 First Nations and Inuit Communities
- Increasing the provision of opioid agonist treatment and implementing SMART (Self-Management and Recovery Training) in Canada's correctional institutions
Harm reduction
- Supported the establishment of supervised consumption sites (SCS) to provide health, social and treatment services
- Authorized different modes of consumption that include injection, oral (swallowing), intranasal (snorting), and inhalation
- Authorized supportive services at sites including drug checking, peer assistance consumption and drug splitting and sharing
- Streamlined the exemption application process
- As of July 2023:
- there are 39 SCS offering services
- SCS received over 4.3 million visits
- SCS attended to almost 50,000 overdoses
- SCS made 271,000 referrals to health and social services
- Improved access to overdose prevention services by allowing provinces and territories to establish temporary spaces where people can consume drugs under supervision to reduce risk of overdose death
- Supported the Good Samaritan Drug Overdose Act, which provides some legal protection related to drug possession for people who seek emergency help during an overdose
- Supported the development of guidance on take-home naloxone programs
- Funded national projects to increase awareness and access to naloxone through training, awareness and distribution of the life saving drug. As of September 2023, these investments have resulted in:
- the training of nearly 2 million people on how to respond to an overdose
- more than 82,800 nasal naloxone kits distributed across Canada
- Continued to improve access to naloxone, including to remote and isolated First Nations and Inuit communities and people experiencing homelessness, through the coordination of bulk purchases of naloxone, increasing access to take-home naloxone kits, and training in their use
- Funding Thunderbird Partnership Foundation to create and distribute take-home nasal naloxone kits directly to communities and individuals
- Supported a drug checking technology challenge to promote development of new drug checking technologies, which included awarding a grand prize of $1 million to Scatr Inc.
- Opened Overdose Prevention Services in two correctional institutions to reduce overdose incidents
- Continuing to support the delivery of harm reduction activities to help reduce risks and connect individuals and families experiencing homelessness with key health and social services through the Reaching Home program
Substance controls
- Granted a 3 year exemption under the Controlled Drugs and Substances Act (CDSA), so that adults aged 18 and over in British Columbia will not be subject to criminal charges for the possession of up to 2.5 grams total of certain illegal drugs for personal use between January 31, 2023 and January 31, 2026
- Former Bill C-5 came into force in November 2022. It repealed mandatory minimum penalties for all drug offences in the CDSA, and requires police and prosecutors to consider diversion for drug possession offences
- It also requires past and future convictions for drug possession to be sequestered apart after a certain period of time
- Made scheduling amendments to the CDSA and Precursor Control Regulations to help address the illegal importation and distribution of a group of novel fentanyl precursors that are used in the illegal production of fentanyl and its analogues
- Advancing additional scheduling amendments to control a group of novel synthetic opioids and a new group of emerging fentanyl precursors
- Released guidance to consider alternatives to prosecution for simple drug possession offences, except when there are serious public safety concerns
- Identified opioids, including nitazenes, 135,923 times from January 2018 to October 2023 in samples submitted to the Drug Analysis Service by law enforcement and public health partners (samples may contain more than one opioid)
- Seizing illegal opioids and precursor chemicals that can be used in the production of illegal synthetic drugs
- Providing border services officers with tools to safely identify and interdict fentanyl and other toxic substances at the border, including:
- Implementing 82 safe examination areas at high-risk ports of entry to help border services officers to identify and safely examine shipments suspected to contain opioids
- Maintaining field drug analysis sites with on-site chemists in Toronto, Montreal, and Vancouver
- Added fentanyl detection to the scent profile of 6 drug and firearm detector dog teams strategically located across the country
- Working with private sector partners to address money laundering of the proceeds of fentanyl trafficking
- Continuing to investigate and charge criminal actors suspected of manufacturing and/or trafficking illegal substances, including:
- Working with private sector partners to limit the flow of legitimate chemicals for the purpose of manufacturing illegal substances
- Investigating and dismantling clandestine drug labs capable of producing large quantities of synthetic drugs
- Targeting organized crime groups involved in the illicit production and trafficking of synthetic drugs
Page details
- Date modified: